Parkinson Disease (PD) primarily affects older adults. It is the second-most common neurodegenerative disease after Alzheimer’s disease. Freezing of Gait (FoG) is a symptom present in approximately 80% of advanced-stage PD’s patients. FoG episodes alter the continuity of gait, and may be the cause of falls that can lead to injuries and even death. The recent advances in the development of hardware and software systems for the monitoring, stimulus, or rehabilitation of patients with FoG has been of great interest to researchers because detection and minimization of the duration of FoG events is an important factor in improving the quality of life.
- Parkinson Disease
- freezing of gait
1. Introduction
2. Brain Activity during a FoG Episode
3. Motor Characteristics during FoG
This entry is adapted from the peer-reviewed paper 10.3390/healthcare10060976
References
- Dauer, W.; Przedborski, S. Parkinson’s Disease. Neuron 2003, 39, 889–909.
- Kalia, L.; Lang, A. Parkinson’s disease. Lancet 2015, 386, 896–912.
- Pringsheim, T.; Jette, N.; Frolkis, A.; Steeves, T. The prevalence of Parkinson’s disease: A systematic review and meta-analysis. Mov. Disord. 2014, 29, 1583–1590.
- Van Den Eeden, S. Incidence of Parkinson’s Disease: Variation by Age, Gender, and Race/Ethnicity. Am. J. Epidemiol. 2003, 157, 1015–1022.
- Lee, A.; Gilbert, R. Epidemiology of Parkinson Disease. Neurol. Clin. 2016, 34, 955–965.
- Driver, J.; Logroscino, G.; Gaziano, J.; Kurth, T. Incidence and remaining lifetime risk of Parkinson disease in advanced age. Neurology 2009, 72, 432–438.
- Calabrese, V.; Dorsey, E.; Constantinescu, R.; Thompson, J.; Biglan, K.; Holloway, R.; Kieburtz, K.; Marshall, F.; Ravina, B.; Schifitto, G.; et al. Projected Number of People With Parkinson Disease in the Most Populous Nations, 2005 Through 2030. Neurology 2007, 69, 223–224.
- Gelb, D.; Oliver, E.; Gilman, S. Diagnostic Criteria for Parkinson Disease. Arch. Neurol. 1999, 56, 33.
- Heremans, E.; Nieuwboer, A.; Vercruysse, S. Freezing of Gait in Parkinson’s Disease: Where Are We Now? Curr. Neurol. Neurosci. Rep. 2013, 13, 350.
- Nutt, J.; Bloem, B.; Giladi, N.; Hallett, M.; Horak, F.; Nieuwboer, A. Freezing of gait: Moving forward on a mysterious clinical phenomenon. Lancet Neurol. 2011, 10, 734–744.
- Rahman, S.; Griffin, H.; Quinn, N.; Jahanshahi, M. Quality of life in Parkinson’s disease: The relative importance of the symptoms. Mov. Disord. 2008, 23, 1428–1434.
- Tan, D.; Danoudis, M.; McGinley, J.; Morris, M. Relationships between motor aspects of gait impairments and activity limitations in people with Parkinson’s disease: A systematic review. Park. Relat. Disord. 2012, 18, 117–124.
- Giladi, N.; McDermott, M.; Fahn, S.; Przedborski, S.; Jankovic, J.; Stern, M.; Tanner, C. Freezing of gait in PD: Prospective assessment in the DATATOP cohort. Neurology 2001, 56, 1712–1721.
- Tan, D.; McGinley, J.; Danoudis, M.; Iansek, R.; Morris, M. Freezing of Gait and Activity Limitations in People With Parkinson’s Disease. Arch. Phys. Med. Rehabil. 2011, 92, 1159–1165.
- Hely, M.; Morris, J.; Reid, W.; Trafficante, R. Sydney multicenter study of Parkinson’s disease: Non-L-dopa-responsive problems dominate at 15 years. Mov. Disord. 2005, 20, 190–199.
- Peterson, D.; Pickett, K.; Duncan, R.; Perlmutter, J.; Earhart, G. Gait-Related Brain Activity in People with Parkinson Disease with Freezing of Gait. PLoS ONE 2014, 9, e90634.
- Peterson, D.; Fling, B.; Mancini, M.; Cohen, R.; Nutt, J.; Horak, F. Dual-task interference and brain structural connectivity in people with Parkinson’s disease who freeze. J. Neurol. Neurosurg. Psychiatry 2014, 86, 786–792.
- Perlmutter, J.S.; Mink, J.W. Deep brain stimulation. Annu. Rev. Neurosci. 2006, 29, 229–257.
- George, M.S.; Sackeim, H.A.; Rush, A.J.; Marangell, L.B.; Nahas, Z.; Husain, M.M.; Lisanby, S.; Burt, T.; Goldman, J.; Ballenger, J.C. Vagus nerve stimulation: A new tool for brain research and therapy. Biol. Psychiatry 2000, 47, 287–295.
- Rattay, F. The basic mechanism for the electrical stimulation of the nervous system. Neuroscience 1999, 89, 335–346.
- Fukuyama, H.; Ouchi, Y.; Matsuzaki, S.; Nagahama, Y.; Yamauchi, H.; Ogawa, M.; Kimura, J.; Shibasaki, H. Brain functional activity during gait in normal subjects: A SPECT study. Neurosci. Lett. 1997, 228, 183–186.
- Rivlin-Etzion, M.; Marmor, O.; Saban, G.; Rosin, B.; Haber, S.N.; Vaadia, E.; Prut, Y.; Bergman, H. Low-Pass filter properties of basal ganglia–cortical–muscle loops in the normal and MPTP primate model of Parkinsonism. J. Neurosci. 2008, 28, 633–649.
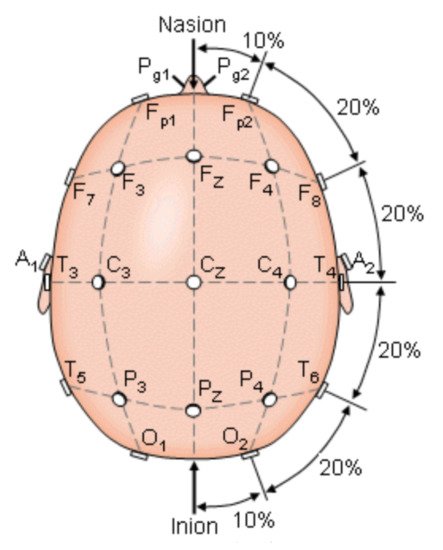
- Bhavsar, R.; Sun, Y.; Helian, N.; Davey, N.; Mayor, D.; Steffert, T. The correlation between EEG signals as measured in different positions on scalp varying with distance. Procedia Comput. Sci. 2018, 123, 92–97.
- Handojoseno, M.A.; Shine, J.M.; Nguyen, T.N.; Tran, Y.; Lewis, S.J.G.; Nguyen, H.T. The detection of Freezing of Gait in Parkinson’s disease patients using EEG signals based on Wavelet decomposition. In Proceedings of the 2012 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, San Diego, CA, USA, 28 August–1 September 2012; pp. 69–72.
- Handojoseno, A.M.A.; Shine, J.M.; Nguyen, T.N.; Tran, Y.; Lewis, S.J.G.; Nguyen, H.T. Using EEG spatial correlation, cross frequency energy, and wavelet coefficients for the prediction of Freezing of Gait in Parkinson’s Disease patients. In Proceedings of the 2013 35th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Osaka, Japan, 3–7 July 2013; pp. 4263–4266.
- Amboni, M.; Barone, P.; Picillo, M.; Cozzolino, A.; Longo, K.; Erro, R.; Iavarone, A. A two-year follow-up study of executive dysfunctions in Parkinsonian patients with freezing of gait at on-state. Mov. Disord. 2010, 25, 800–802.
- Tessitore, A.; Amboni, M.; Esposito, F.; Russo, A.; Picillo, M.; Marcuccio, L.; Pellecchia, M.; Vitale, C.; Cirillo, M.; Tedeschi, G.; et al. Resting-state brain connectivity in patients with Parkinson’s disease and freezing of gait. Park. Relat. Disord. 2012, 18, 781–787.
- Almeida, Q.; Lebold, C. Freezing of gait in Parkinson’s disease: A perceptual cause for a motor impairment? J. Neurol. Neurosurg. Psychiatry 2009, 81, 513–518.
- Grabli, D.; Karachi, C.; Welter, M.; Lau, B.; Hirsch, E.; Vidailhet, M.; François, C. Normal and pathological gait: What we learn from Parkinson’s disease. J. Neurol. Neurosurg. Psychiatry 2012, 83, 979–985.
- Wang, M.; Jiang, S.; Yuan, Y.; Zhang, L.; Ding, J.; Wang, J.; Zhang, J.; Zhang, K.; Wang, J. Alterations of functional and structural connectivity of freezing of gait in Parkinson’s disease. J. Neurol. 2016, 263, 1583–1592.
- Sage, M.; Almeida, Q. A positive influence of vision on motor symptoms during sensory attention focused exercise for Parkinson’s disease. Mov. Disord. 2010, 25, 64–69.
- Uc, E.; Rizzo, M.; Anderson, S.; Qian, S.; Rodnitzky, R.; Dawson, J. Visual dysfunction in Parkinson disease without dementia. Neurology 2005, 65, 1907–1913.
- Yogev-Seligmann, G.; Hausdorff, J.; Giladi, N. The role of executive function and attention in gait. Mov. Disord. 2008, 23, 329–342.
- Lenka, A.; Naduthota, R.; Jha, M.; Panda, R.; Prajapati, A.; Jhunjhunwala, K.; Saini, J.; Yadav, R.; Bharath, R.; Pal, P. Freezing of gait in Parkinson’s disease is associated with altered functional brain connectivity. Park. Relat. Disord. 2016, 24, 100–106.
- Ricciardi, L.; Bloem, B.R.; Snijders, A.H.; Daniele, A.; Quaranta, D.; Bentivoglio, A.R.; Fasano, A. Freezing of gait in Parkinson’s disease: The paradoxical interplay between gait and cognition. Park. Relat. Disord. 2014, 20, 824–829.
- Tripoliti, E.; Tzallas, A.; Tsipouras, M.; Rigas, G.; Bougia, P.; Leontiou, M.; Konitsiotis, S.; Chondrogiorgi, M.; Tsouli, S.; Fotiadis, D. Automatic detection of freezing of gait events in patients with Parkinson’s disease. Comput. Methods Programs Biomed. 2013, 110, 12–26.
- Schaafsma, J.; Balash, Y.; Gurevich, T.; Bartels, A.; Hausdorff, J.; Giladi, N. Characterization of freezing of gait subtypes and the response of each to levodopa in Parkinson’s disease. Eur. J. Neurol. 2003, 10, 391–398.
- Dietz, M.; Goetz, C.; Stebbins, G. Evaluation of a modified inverted walking stick as a treatment for Parkinsonian freezing episodes. Mov. Disord. 1990, 5, 243–247.
- Okuma, Y. Freezing of gait in Parkinson’s disease. J. Neurol. 2006, 253, vii27–vii32.
- Freeman, J.S.; Cody, F.W.; Schady, W. The influence of external timing cues upon the rhythm of voluntary movements in Parkinsonś disease. J. Neurol. Neurosurg. Psychiatry 1993, 56, 1078–1084.
- Rutz, D.G.; Benninger, D.H. Physical therapy for freezing of gait and gait impairments in Parkinson disease: A systematic review. PM&R 2020, 12, 1140–1156.
- Bartels, A.; Balash, Y.; Gurevich, T.; Schaafsma, J.; Hausdorff, J.; Giladi, N. Relationship between freezing of gait (FOG) and other features of Parkinson’s: FOG is not correlated with bradykinesia. J. Clin. Neurosci. 2003, 10, 584–588.
- Hausdorff, J.; Schaafsma, J.; Balash, Y.; Bartels, A.; Gurevich, T.; Giladi, N. Impaired regulation of stride variability in Parkinson’s disease subjects with freezing of gait. Exp. Brain Res. 2003, 149, 187–194.
- Plotnik, M.; Giladi, N.; Hausdorff, J. Bilateral coordination of walking and freezing of gait in Parkinson’s disease. Eur. J. Neurosci. 2008, 27, 1999–2006.
- Fortaleza, A.d.; Mancini, M.; Carlson-Kuhta, P.; King, L.; Nutt, J.; Chagas, E.; Freitas, I.; Horak, F. Dual task interference on postural sway, postural transitions and gait in people with Parkinson’s disease and freezing of gait. Gait Posture 2017, 56, 76–81.
- Mazilu, S.; Blanke, U.; Calatroni, A.; Gazit, E.; Hausdorff, J.; Tröster, G. The role of wrist-mounted inertial sensors in detecting gait freeze episodes in Parkinson’s disease. Pervasive Mob. Comput. 2016, 33, 1–16.
- Daneault, J.F.; Vergara-Diaz, G.; Parisi, F.; Admati, C.; Alfonso, C.; Bertoli, M.; Bonizzoni, E.; Carvalho, G.F.; Costante, G.; Fabara, E.E.; et al. Accelerometer data collected with a minimum set of wearable sensors from subjects with Parkinson’s disease. Sci. Data 2021, 8, 48.
- Bonora, G.; Mancini, M.; Carpinella, I.; Chiari, L.; Ferrarin, M.; Nutt, J.; Horak, F. Investigation of Anticipatory Postural Adjustments during One-Leg Stance Using Inertial Sensors: Evidence from Subjects with Parkinsonism. Front. Neurol. 2017, 8, 361.
- Jacobs, J. Multiple balance tests improve the assessment of postural stability in subjects with Parkinson’s disease. J. Neurol. Neurosurg. Psychiatry 2005, 77, 322–326.
- Smithson, F.; Morris, M.; Iansek, R. Performance on Clinical Tests of Balance in Parkinson’s Disease. Phys. Ther. 1998, 78, 577–592.
- Morris, M.; Iansek, R.; Smithson, F.; Huxham, F. Postural instability in Parkinson’s disease: A comparison with and without a concurrent task. Gait Posture 2000, 12, 205–216.
- Adkin, A.; Frank, J.; Jog, M. Fear of falling and postural control in Parkinson’s disease. Mov. Disord. 2003, 18, 496–502.
- Vellas, B.; Wayne, S.; Romero, L.; Baumgartner, R.; Rubenstein, L.; Garry, P. One-Leg Balance Is an Important Predictor of Injurious Falls in Older Persons. J. Am. Geriatr. Soc. 1997, 45, 735–738.
- Youn, J.; Okuma, Y.; Hwang, M.; Kim, D.; Cho, J. Falling Direction can Predict the Mechanism of Recurrent Falls in Advanced Parkinson’s Disease. Sci. Rep. 2017, 7, 3921.
- Kerr, G.; Worringham, C.; Cole, M.; Lacherez, P.; Wood, J.; Silburn, P. Predictors of future falls in Parkinson disease. Neurology 2010, 75, 116–124.
- Matinolli, M.; Korpelainen, J.; Sotaniemi, K.; Myllylä, V.; Korpelainen, R. Recurrent falls and mortality in Parkinson’s disease: A prospective two-year follow-up study. Acta Neurol. Scand. 2011, 123, 193–200.
- Bloem, B.; Hausdorff, J.; Visser, J.; Giladi, N. Falls and freezing of gait in Parkinson’s disease: A review of two interconnected, episodic phenomena. Mov. Disord. 2004, 19, 871–884.
- Voss, T.; Elm, J.; Wielinski, C.; Aminoff, M.; Bandyopadhyay, D.; Chou, K.; Sudarsky, L.; Tilley, B. Fall frequency and risk assessment in early Parkinson’s disease. Park. Relat. Disord. 2012, 18, 837–841.
- Bloem, B.; Grimbergen, Y.; Cramer, M.; Willemsen, M.; Zwinderman, A. Prospective assessment of falls in Parkinson’s disease. J. Neurol. 2001, 248, 950–958.
- Lindholm, B.; Hagell, P.; Hansson, O.; Nilsson, M. Prediction of Falls and/or Near Falls in People with Mild Parkinson’s Disease. PLoS ONE 2015, 10, e0117018.
- Wood, B. Incidence and prediction of falls in Parkinson’s disease: A prospective multidisciplinary study. J. Neurol. Neurosurg. Psychiatry 2002, 72, 721–725.
- Bloem, B.; Munneke, M.; Carpenter, M.; Allum, J.; Pressley, J. The impact of comorbid disease and injuries on resource use and expenditures in parkinsonism. Neurology 2003, 61, 1023.
- Gazibara, T.; Pekmezovic, T.; Tepavcevic, D.K.; Svetel, M.; Tomic, A.; Stankovic, I.; Kostic, V. Health-related quality of life in patients with Parkinson’s disease: Implications for falling. Park. Relat. Disord. 2015, 21, 573–576.
- Walton, C.; Shine, J.; Hall, J.; O’Callaghan, C.; Mowszowski, L.; Gilat, M.; Szeto, J.; Naismith, S.; Lewis, S. The major impact of freezing of gait on quality of life in Parkinson’s disease. J. Neurol. 2002, 72, 721–725.
- Parihar, R.; Mahoney, J.; Verghese, J. Relationship of Gait and Cognition in the Elderly. Curr. Transl. Geriatr. Exp. Gerontol. Rep. 2013, 2, 167–173.
