Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Myopia is a global health issue, and the prevalence of high myopia has increased significantly in the past five to six decades. Artificial intelligence (AI) has been identified as one of the key drivers of the Fourth Industrial Revolution. Because of the growth of digital databases, the number of AI-based applications in the medical field based on Python or C has increased immensely in recent years.
- diagnosis and management
- high myopia
- pathologic myopia
1. Introduction
Myopia is a global health issue, and the prevalence of myopia has increased significantly in the past five to six decades [1]. In urban areas of China, Taiwan, Hong Kong, Japan, Singapore, and South Korea [2][3][4][5][6][7], 80–90% of high school students are myopic and 10–20% of them have high myopia [1][8]. The same prevalence has been observed in North America, Germany, Spain, and Russia [9][10][11][12]. The worldwide increase in the prevalence of myopia and PM indicates that myopia-related blindness will increase worldwide in the future [13][14][15][16][17][18][19][20][21][22][23][24][25][26][27][28][29]. A lack or shortage of myopia specialists is a great concern to governmental leaders, and the control of myopia has been a national policy in China [30].
In PM eyes, there is an increase in the axial length and the presence of a posterior staphyloma, a deformity of the posterior segment of the eye [31][32][33][34][35]. Following a deformation of the sclera, the neural retina is mechanically damaged and blinding pathologic changes develop in the macular region. The eyes are then said to have myopic maculopathy, which is the main sight-threatening complication. In addition, it has been reported that the cost for one myopic patient would be over seven hundred United States dollars/year and 17 thousand United States dollars during the patient’s lifetime in Singapore [36]. In China, it is estimated that myopia-associated productivity loss is about 244 billion United States dollars/year [30][37]. These values indicate that myopia is an increasingly serious public health problem with a high economic burden. Because myopic maculopathy is generally progressive and irreversible, interventions to prevent the progression of myopic eyes to PM, continuous surveillance, and slowing the progression of PM are highly recommended. However, the number of well-trained myopia specialists is insufficient worldwide and the diagnosis of myopic maculopathy is difficult for general eye care providers, e.g., optometrists or general ophthalmologists, and a continuous monitoring of every myopic patient is inefficient in both time and cost. For example, various lesions of myopic maculopathy often co-exist in the same eye, which makes their appearance difficult to interpret. Thus, there is a great need for automated methods that can be used in a cost-efficient way to assist physicians in monitoring PM and to manage PM patients who need the care of specialists.
Artificial intelligence (AI) has been identified as one of the key drivers of the Fourth Industrial Revolution [38]. Because of the growth of digital databases, the number of AI-based applications in the medical field based on Python or C has increased immensely in recent years [39][40]. One of the main parts of AI is machine learning (ML), which not only has a powerful capacity for statistical analyses but also has a great ability to manipulate data and perform complex operations to find relationships among the many biological characteristics. As an evolutionary form of ML, deep learning (DL) enhances these advantages and has reached a new high by processing data through information in hidden layers.
Many successful models and platforms have been established for screening and diagnosing age-related macular degeneration [41][42][43], diabetic retinopathy [44][45], and glaucoma [46]. These applications focused on analyzing ophthalmic images to diagnose the disease and to determine prognosis from these images. However, in addition to a general workflow, which is shown in Figure 1, high myopia and PM generate even more data because both the ophthalmic information and morphological changes of the retina and choroid need to be analyzed.
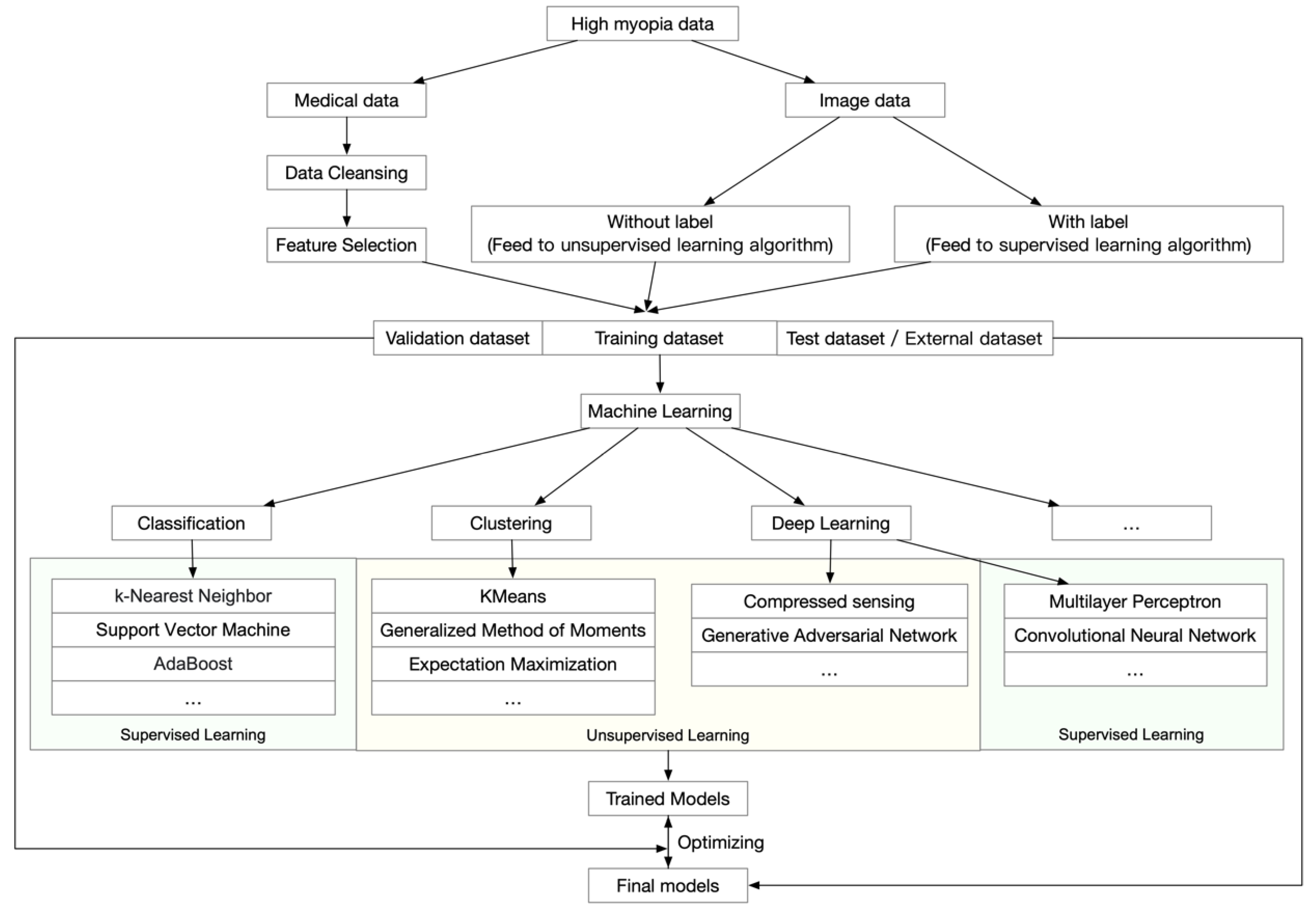 Figure 1. General workflow of artificial intelligence analyses of high myopia and pathologic myopia.
Figure 1. General workflow of artificial intelligence analyses of high myopia and pathologic myopia.2. Data-Driven AI in High Myopia and Pathologic Myopia
PM is associated with an elongation of the axial length of the eye, which is usually associated with morphological changes in the sclera, choroid, Bruch’s membrane, retinal pigment epithelium, and neural retina. In addition, due to increases in the progressive and excessive axial lengths, highly myopic eyes also have high refractive errors and related ophthalmic changes. These changes may be further amplified when the eye undergoes refractive or cataract surgery due to the excessive length of the eye. Thus, it is expected that high myopia will generate a considerable amount of data during a long-term follow-up period, which would require an efficient method to analyze and interpret the findings.
Earlier, redundant and inconsistent data were collected due to the non-integrated and fragmented data management procedures. This has led to information quality problems, which has hampered the acquisition of an accurate diagnosis, resulting in poor management of myopic eyes.
With the recent creation and general distribution of digital hospital information systems, an opportunity has opened up for determining the onset and progression of PM through a much larger set of data. This has advanced the understanding of PM with more comprehensive perspectives and on more solid theoretical bases.
Data-driven AI studies are usually performed using ML techniques because they can detect different categories, obtain information buried in a large amount of data, and optimize the model that best fits the data. The models that are regressed by training data would verify the capacity for data categorization. ML techniques involve supervised learning, semi-supervised learning, and unsupervised learning. They include many methods such as kernel ridge regression, support vector machines (SVM), nearest neighbors, gaussian processes, naive Bayes, random forests, neural networks, and others. Further evolutional methods such as extreme gradient boosting (XGBoost) and light gradient boosting machine (LightGBM) supply more chances in regression models and can determine potential relationships to understand the occurrence and progression of high and pathologic myopia. With these powerful methods, representative patterns can be statistically calculated and extracted for ensemble predictive models.
Earlier studies reported that the incidence of myopia had reached 84.6% in elementary school children and 95.5% in university students in China [47][48][49], and it is not difficult to believe that such levels are not unique to China. Thus, it is urgent to monitor eyes with high myopia at an earlier stage, which raises the need for AI-assisted screening techniques. In areas with high levels of myopia, several data-driven studies on high myopia have reported that DL learning models can be used to solve real problems with sensible solutions (Table 1). The ML models have shown that the refractive errors and the risk of high myopia (myopia ≤ −6.0 diopters) that develop within ten years are predictable in school-aged children [50]. In this approach, the random forest model, generalized estimating equation model, and mixed-effects model were fitted and evaluated by the coefficient of determination (R2), the root mean square error (RMSE), mean absolute error (MAE), and characteristics of the area under the receiver operating curves (AUC). The model was tested by both internal and external datasets. Typically, the random forest model had the best performance and the AUC reached as high as 0.802 to 0.976. This approach provided evidence for transforming clinical practice, health policy-making, and precise individualized interventions regarding the practical control of school-aged myopia by employing big data and ML. However, in some circumstances where the clinical data are not available, it may be difficult for physicians to manage high myopia patients. To address this, ML models were also designed and trained to play roles in analyzing eyes with high myopia. By training with the wavefront aberrometry values through the XGBoost algorithm, DL models have been used to predict the subjective refractive errors, and the mean absolute error between true values and predicted values ranged from 0.094 to 0.301 diopters, and the combination of machine learning and aberrometry based on wavefront decomposition basis will aid in the development of refined algorithms [51]. Furthermore, highly myopic eyes often have hyperopic refractive errors after cataract surgery, despite the use of partial coherence interferometry, which could eliminate biometric errors. Through XGBoost regression, AI models trained by medical records extracted from myopia patients could improve the accuracy of implementing IOL power in high myopia with cataracts [52].
Table 1. Data-driven artificial intelligence (AI) models in high myopia and pathologic myopia.
| Research | Year | Materials | Participants | AI Methods | Main Outcome | Evolutions and Performance |
|---|---|---|---|---|---|---|
| Lin, H. et al. [50] | 2018 | Refraction data | School-aged children | ML | Predicting the presence of high myopia | AUC: 0.802–0.976 |
| Kaya, C. et al. [53] | 2018 | electrooculographic data | Adults (25–65 years old) | ML | Detecting hypermetropia and myopia refractive disorders | Sensitivity: 95.5%; specificity: 96%; classification accuracy: 90.91% |
| Ye, B. et al. [54] | 2019 | luminance, ultraviolet light levels, and step number data | Myopia patients | ML | Differentiating indoor and outdoor locations | Accuracy: 0.827–0.996; AUC: 0.90–0.99 |
| Rampat, R. et al. [51] | 2020 | Wavefront aberrometry data | General population | ML | Predicting subjective refraction | mean absolute error: 0.094–0.301 diopters |
| Tang, T. et al. [55] | 2020 | Medical data | School-age myopic children | ML | Estimating physiological elongation of axial length | R square equals 0.87 |
| Wei, L. et al. [52] | 2020 | Medical data | Myopia patients | ML | Improving the accuracy of IOL power predictions | mean absolute error: 0.25–0.29; median squared errors: 0.06–0.09 |
| Yang, X. et al. [56] | 2020 | Medical data | Primary school children | ML | Studying influence of related factors on incidence of myopia in adolescents | Accuracy equals 0.92–0.93; Precision equals 0.95; Sensitivity equals 0.94; f1 equals 0.94; AUC equals 0.98; Specificity equals 0.94 |
| Li, S.M. et al. [57] | 2022 | Medical data | Primary school children | ML | Detecting risk factors for myopia progression | Combined weight: 77%; Accuracy: over 80% |
AUC, area under the receiver operating characteristic curves; ML, machine learning.
In addition, in situations where only limited information can be accessed, electrooculographic (EOG) data could also be used to train ML models in classifying myopic refractive disorders. It has been reported that when the logistic regression model, Naïve Bayes model, and random forest model were trained by EOG data, the random forest model had the best performance with a sensitivity of 95.5% and a specificity of 96%. The total classification accuracy reached 90.91%, and the achieved models could inspire novel approaches to clinical screening of myopia when general data are not available [53]. Furthermore, because the axial length value is a key indicator for high myopia, simply assessing the change in axial length can be used to evaluate the myopia progression. More specifically, these methods can be used by practitioners to judge the true extent of myopia progression before performing a cycloplegic refraction examination. Linear regression, SVM, and bagged trees have been used to predict increases in axial length in adolescents. From an evaluation of the performance of models by five-folded cross-validation, the linear model achieved a high level of precision with an R square value of 0.87 [55].
In addition to these methods of predicting the actual outputs, there are other ways to use AI algorithms. It is generally accepted that clinical data tend to be imperfect and may lack different parts during clinical research because each performed examination is required to test the evidence-based hypothesis. However, these imperfect data would be a high barrier for research and the understanding of these disease processes. One of the benefits of ML algorithms is that they can fill in the missing values based on a scientific method, and the results can be closer to the true value. This will lead to a better understanding of the occurrences and progression of the disease processes. Furthermore, even with abundant data or features that can be assessed, physicians still need to determine how to filter out important values to test a hypothesis. In addition to traditional methods such as the principal component analysis (PCA), ML algorithms supply multiple choices for data dimension reduction, such as randomized singular value decomposition-based PCA, spectral embedding, isomap embedding, and others. These algorithms offer opportunities for clinicians to analyze the abundant data and to determine ways to test their hypotheses.
For myopia control, it is widely known that the environment, especially luminance and ultraviolet, plays important roles in affecting the progression of myopia. As the nature of collecting monitoring environmental data is complex, it is difficult to implement monitoring widely in the public. Through luminance, ultraviolet light levels, and step number data, AI models could be trained in different indoor and outdoor locations. These methods can be useful monitoring tools for community- or school-based public health interventions or individual health management [54].
ML models have been typically used to fill in missing clinical data and to select features that were highly correlated with the myopia in adolescents [56]. Features selected by ML learning algorithms have been used to explore the potential risk factors that affect the severe axial length elongation in highly myopic eyes. These approaches are particularly important because they provide reference data for physicians when faced with complex situations. To screen for high myopia in rural areas where myopia specialists or essential instruments are not available, these predictive values would be important indicators for high myopia screening and for monitoring the progression of myopia.
This entry is adapted from the peer-reviewed paper 10.3390/diagnostics12051210
References
- Morgan, I.G.; Ohno-Matsui, K.; Saw, S.M. Myopia. Lancet 2012, 379, 1739–1748.
- Dong, L.; Kang, Y.K.; Li, Y.; Wei, W.B.; Jonas, J.B. Prevalence and time trends of myopia in children and adolescents in China: A Systemic Review and Meta-Analysis. Retina 2020, 40, 399–411.
- Lin, L.L.; Shih, Y.F.; Hsiao, C.K.; Chen, C.J. Prevalence of myopia in Taiwanese schoolchildren: 1983 to 2000. Ann. Acad. Med. Singap. 2004, 33, 27–33.
- Edwards, M.H.; Lam, C.S. The epidemiology of myopia in Hong Kong. Ann. Acad. Med. Singap. 2004, 33, 34–38.
- Ueda, E.; Yasuda, M.; Fujiwara, K.; Hashimoto, S.; Ohno-Matsui, K.; Hata, J.; Ishibashi, T.; Ninomiya, T.; Sonoda, K.H. Trends in the Prevalence of Myopia and Myopic Maculopathy in a Japanese Population: The Hisayama Study. Investig. Ophthalmol. Vis. Sci. 2019, 60, 2781–2786.
- Sensaki, S.; Sabanayagam, C.; Verkicharla, P.K.; Awodele, A.; Tan, K.H.; Chia, A.; Saw, S.M. An Ecologic Study of Trends in the Prevalence of Myopia in Chinese Adults in Singapore Born from the 1920s to 1980s. Ann. Acad. Med. Singap. 2017, 46, 229–236.
- Han, S.B.; Jang, J.; Yang, H.K.; Hwang, J.M.; Park, S.K. Prevalence and risk factors of myopia in adult Korean population: Korea national health and nutrition examination survey 2013-2014 (KNHANES VI). PLoS ONE 2019, 14, e0211204.
- Morgan, I.G.; French, A.N.; Ashby, R.S.; Guo, X.; Ding, X.; He, M.; Rose, K.A. The epidemics of myopia: Aetiology and prevention. Prog Retin Eye Res. 2018, 62, 134–149.
- Reed, D.S.; Ferris, L.M.; Santamaria, J.; Mehta, A.; Musto, M.; Apsey, D.; Legault, G.L. Prevalence of Myopia in Newly Enlisted Airmen at Joint Base San Antonio. Clin. Ophthalmol. 2020, 14, 133–137.
- Hopf, S.; Korb, C.; Nickels, S.; Schulz, A.; Munzel, T.; Wild, P.S.; Michal, M.; Schmidtmann, I.; Lackner, K.J.; Pfeiffer, N.; et al. Prevalence of myopic maculopathy in the German population: Results from the Gutenberg health study. Br. J. Ophthalmol. 2020, 104, 1254–1259.
- Alvarez-Peregrina, C.C.; Sanchez-Tena, M.; Martinez-Perez, C.C.; Villa-Collar, C.C. Prevalence and Risk Factors of Myopia in Spain. J. Ophthalmol. 2019, 2019, 3419576.
- Bikbov, M.M.; Gilmanshin, T.R.; Kazakbaeva, G.M.; Zainullin, R.M.; Rakhimova, E.M.; Rusakova, I.A.; Bolshakova, N.I.; Safiullina, K.R.; Zaynetdinov, A.F.; Zinatullin, A.A.; et al. Prevalence of Myopic Maculopathy Among Adults in a Russian Population. JAMA Netw. Open 2020, 3, e200567.
- Tang, Y.; Wang, X.; Wang, J.; Huang, W.; Gao, Y.; Luo, Y.; Lu, Y. Prevalence and Causes of Visual Impairment in a Chinese Adult Population: The Taizhou Eye Study. Ophthalmology 2015, 122, 1480–1488.
- Iwase, A.; Araie, M.; Tomidokoro, A.; Yamamoto, T.; Shimizu, H.; Kitazawa, Y.; Tajimi Study, G. Prevalence and causes of low vision and blindness in a Japanese adult population: The Tajimi Study. Ophthalmology 2006, 113, 1354–1362.
- Xu, L.; Wang, Y.; Li, Y.; Wang, Y.; Cui, T.; Li, J.; Jonas, J.B. Causes of blindness and visual impairment in urban and rural areas in Beijing: The Beijing Eye Study. Ophthalmology 2006, 113, 1134.e1–1134.e11.
- Avisar, R.; Friling, R.; Snir, M.; Avisar, I.; Weinberger, D. Estimation of prevalence and incidence rates and causes of blindness in Israel, 1998–2003. Isr. Med. Assoc. J. 2006, 8, 880–881.
- Kuang, T.M.; Tsai, S.Y.; Hsu, W.M.; Cheng, C.Y.; Liu, J.H.; Chou, P. Correctable visual impairment in an elderly Chinese population in Taiwan: The Shihpai Eye Study. Investig. Ophthalmol. Vis. Sci. 2007, 48, 1032–1037.
- Dandona, L.; Dandona, R.; Srinivas, M.; Giridhar, P.; Vilas, K.; Prasad, M.N.; John, R.K.; McCarty, C.A.; Rao, G.N. Blindness in the Indian state of Andhra Pradesh. Investig. Ophthalmol. Vis. Sci. 2001, 42, 908–916.
- Van Newkirk, M.R. The Hong Kong vision study: A pilot assessment of visual impairment in adults. Trans. Am. Ophthalmol. Soc. 1997, 95, 715–749.
- Varma, R.; Kim, J.S.; Burkemper, B.S.; Wen, G.; Torres, M.; Hsu, C.; Choudhury, F.; Azen, S.P.; McKean-Cowdin, R.; Chinese American Eye Study Group. Prevalence and Causes of Visual Impairment and Blindness in Chinese American Adults: The Chinese American Eye Study. JAMA Ophthalmol. 2016, 134, 785–793.
- Cotter, S.A.; Varma, R.; Ying-Lai, M.; Azen, S.P.; Klein, R.; Los Angeles Latino Eye Study Group. Causes of low vision and blindness in adult Latinos: The Los Angeles Latino Eye Study. Ophthalmology 2006, 113, 1574–1582.
- Sainz-Gomez, C.; Fernandez-Robredo, P.; Salinas-Alaman, A.; Montanes, J.M.; Escudero Berasategui, J.M.; Guillen-Grima, F.; Ruiz-Moreno, J.M.; Garcia-Layana, A. Prevalence and causes of bilateral blindness and visual impairment among institutionalized elderly people in Pamplona, Spain. Eur. J. Ophthalmol. 2010, 20, 442–450.
- Cedrone, C.; Culasso, F.; Cesareo, M.; Nucci, C.; Palma, S.; Mancino, R.; Cerulli, L. Incidence of blindness and low vision in a sample population: The Priverno Eye Study, Italy. Ophthalmology 2003, 110, 584–588.
- Buch, H.; Vinding, T.; La Cour, M.; Appleyard, M.; Jensen, G.B.; Nielsen, N.V. Prevalence and causes of visual impairment and blindness among 9980 Scandinavian adults: The Copenhagen City Eye Study. Ophthalmology 2004, 111, 53–61.
- Bamashmus, M.A.; Matlhaga, B.; Dutton, G.N. Causes of blindness and visual impairment in the West of Scotland. Eye 2004, 18, 257–261.
- Krumpaszky, H.G.; Ludtke, R.; Mickler, A.; Klauss, V.; Selbmann, H.K. Blindness incidence in Germany. A population-based study from Wurttemberg-Hohenzollern. Ophthalmologica 1999, 213, 176–182.
- Klaver, C.C.; Wolfs, R.C.; Vingerling, J.R.; Hofman, A.; de Jong, P.T. Age-specific prevalence and causes of blindness and visual impairment in an older population: The Rotterdam Study. Arch. Ophthalmol. 1998, 116, 653–658.
- Gao, L.Q.; Liu, W.; Liang, Y.B.; Zhang, F.; Wang, J.J.; Peng, Y.; Wong, T.Y.; Wang, N.L.; Mitchell, P.; Friedman, D.S. Prevalence and characteristics of myopic retinopathy in a rural Chinese adult population: The Handan Eye Study. Arch. Ophthalmol. 2011, 129, 1199–1204.
- Vongphanit, J.; Mitchell, P.; Wang, J.J. Prevalence and progression of myopic retinopathy in an older population. Ophthalmology 2002, 109, 704–711.
- Jan, C.; Li, L.; Keay, L.; Stafford, R.S.; Congdon, N.; Morgan, I. Prevention of myopia, China. Bull. World Health Organ. 2020, 98, 435–437.
- Moriyama, M.; Ohno-Matsui, K.; Hayashi, K.; Shimada, N.; Yoshida, T.; Tokoro, T.; Morita, I. Topographic analyses of shape of eyes with pathologic myopia by high-resolution three-dimensional magnetic resonance imaging. Ophthalmology 2011, 118, 1626–1637.
- Moriyama, M.; Ohno-Matsui, K.; Modegi, T.; Kondo, J.; Takahashi, Y.; Tomita, M.; Tokoro, T.; Morita, I. Quantitative analyses of high-resolution 3D MR images of highly myopic eyes to determine their shapes. Investig. Ophthalmol. Vis. Sci. 2012, 53, 4510–4518.
- Ohno-Matsui, K. Proposed classification of posterior staphylomas based on analyses of eye shape by three-dimensional magnetic resonance imaging. Ophthalmology 2014, 121, 1798–1809.
- Shinohara, K.; Tanaka, N.; Jonas, J.B.; Shimada, N.; Moriyama, M.; Yoshida, T.; Ohno-Matsui, K. Ultra-widefield optical coherence tomography to investigate relationships between myopic macular retinoschisis and posterior staphyloma. Ophthalmology 2018, 125, 1575–1586.
- Shinohara, K.; Shimada, N.; Moriyama, M.; Yoshida, T.; Jonas, J.B.; Yoshimura, N.; Ohno-Matsui, K. Posterior Staphylomas in Pathologic Myopia Imaged by Widefield Optical Coherence Tomography. Investig. Ophthalmol. Vis. Sci. 2017, 58, 3750–3758.
- Zheng, Y.F.; Pan, C.W.; Chay, J.; Wong, T.Y.; Finkelstein, E.; Saw, S.M. The economic cost of myopia in adults aged over 40 years in Singapore. Investig. Ophthalmol. Vis. Sci. 2013, 54, 7532–7537.
- Naidoo, K.S.; Fricke, T.R.; Frick, K.D.; Jong, M.; Naduvilath, T.J.; Resnikoff, S.; Sankaridurg, P. Potential Lost Productivity Resulting from the Global Burden of Myopia: Systematic Review, Meta-analysis, and Modeling. Ophthalmology 2019, 126, 338–346.
- Mahomed, S. Healthcare, artificial intelligence and the Fourth Industrial Revolution: Ethical, social and legal considerations. South Afr. J. Bioeth. Law 2018, 11, 93–95.
- Tan, M.; Le, Q.V. EfficientNet: Rethinking Model Scaling for Convolutional Neural Networks. arXiv 2019. e-prints. Available online: https://amaarora.github.io/2020/08/13/efficientnet.html (accessed on 11 May 2022).
- Ravi, D.; Wong, C.; Deligianni, F.; Berthelot, M.; Andreu-Perez, J.; Lo, B.; Yang, G.Z. Deep Learning for Health Informatics. IEEE J Biomed. Health Inf. 2017, 21, 4–21.
- Grassmann, F.; Mengelkamp, J.; Brandl, C.; Harsch, S.; Zimmermann, M.E.; Linkohr, B.; Peters, A.; Heid, I.M.; Palm, C.; Weber, B.H.F. A Deep Learning Algorithm for Prediction of Age-Related Eye Disease Study Severity Scale for Age-Related Macular Degeneration from Color Fundus Photography. Ophthalmology 2018, 125, 1410–1420.
- Burlina, P.M.; Joshi, N.; Pekala, M.; Pacheco, K.D.; Freund, D.E.; Bressler, N.M. Automated Grading of Age-Related Macular Degeneration From Color Fundus Images Using Deep Convolutional Neural Networks. JAMA Ophthalmol. 2017, 135, 1170–1176.
- Peng, Y.; Dharssi, S.; Chen, Q.; Keenan, T.D.; Agron, E.; Wong, W.T.; Chew, E.Y.; Lu, Z. DeepSeeNet: A Deep Learning Model for Automated Classification of Patient-based Age-related Macular Degeneration Severity from Color Fundus Photographs. Ophthalmology 2019, 126, 565–575.
- Abramoff, M.D.; Lou, Y.; Erginay, A.; Clarida, W.; Amelon, R.; Folk, J.C.; Niemeijer, M. Improved Automated Detection of Diabetic Retinopathy on a Publicly Available Dataset Through Integration of Deep Learning. Investig. Ophthalmol. Vis. Sci. 2016, 57, 5200–5206.
- Ting, D.S.W.; Cheung, C.Y.; Lim, G.; Tan, G.S.W.; Quang, N.D.; Gan, A.; Hamzah, H.; Garcia-Franco, R.; San Yeo, I.Y.; Lee, S.Y.; et al. Development and Validation of a Deep Learning System for Diabetic Retinopathy and Related Eye Diseases Using Retinal Images From Multiethnic Populations With Diabetes. JAMA 2017, 318, 2211–2223.
- Li, Z.; He, Y.; Keel, S.; Meng, W.; Chang, R.T.; He, M. Efficacy of a Deep Learning System for Detecting Glaucomatous Optic Neuropathy Based on Color Fundus Photographs. Ophthalmology 2018, 125, 1199–1206.
- Chen, M.; Wu, A.; Zhang, L.; Wang, W.; Chen, X.; Yu, X.; Wang, K. The increasing prevalence of myopia and high myopia among high school students in Fenghua city, eastern China: A 15-year population-based survey. BMC Ophthalmol. 2018, 18, 159.
- Sun, J.; Zhou, J.; Zhao, P.; Lian, J.; Zhu, H.; Zhou, Y.; Sun, Y.; Wang, Y.; Zhao, L.; Wei, Y.; et al. High prevalence of myopia and high myopia in 5060 Chinese university students in Shanghai. Investig. Ophthalmol. Vis. Sci. 2012, 53, 7504–7509.
- Wu, J.F.; Bi, H.S.; Wang, S.M.; Hu, Y.Y.; Wu, H.; Sun, W.; Lu, T.L.; Wang, X.R.; Jonas, J.B. Refractive error, visual acuity and causes of vision loss in children in Shandong, China. The Shandong Children Eye Study. PLoS ONE 2013, 8, e82763.
- Lin, H.; Long, E.; Ding, X.; Diao, H.; Chen, Z.; Liu, R.; Huang, J.; Cai, J.; Xu, S.; Zhang, X.; et al. Prediction of myopia development among Chinese school-aged children using refraction data from electronic medical records: A retrospective, multicentre machine learning study. PLoS Med. 2018, 15, e1002674.
- Rampat, R.; Debellemaniere, G.; Malet, J.; Gatinel, D. Using Artificial Intelligence and Novel Polynomials to Predict Subjective Refraction. Sci. Rep. 2020, 10, 8565.
- Wei, L.; Song, Y.; He, W.; Chen, X.; Ma, B.; Lu, Y.; Zhu, X. Accuracy Improvement of IOL Power Prediction for Highly Myopic Eyes With an XGBoost Machine Learning-Based Calculator. Front. Med. Lausanne 2020, 7, 592663.
- Kaya, C.; Erkaymaz, O.; Ayar, O.; Özer, M. Classification of refractive disorders from electrooculogram (EOG) signals by using data mining techniques. In Proceedings of the 2018 26th Signal Processing and Communications Applications Conference (SIU), Izmir, Turkey, 2–5 May 2018; pp. 1–4.
- Ye, B.; Liu, K.; Cao, S.; Sankaridurg, P.; Li, W.; Luan, M.; Zhang, B.; Zhu, J.; Zou, H.; Xu, X.; et al. Discrimination of indoor versus outdoor environmental state with machine learning algorithms in myopia observational studies. J. Transl. Med. 2019, 17, 314.
- Tang, T.; Yu, Z.; Xu, Q.; Peng, Z.; Fan, Y.; Wang, K.; Ren, Q.; Qu, J.; Zhao, M. A machine learning-based algorithm used to estimate the physiological elongation of ocular axial length in myopic children. Eye Vis. Lond. 2020, 7, 50.
- Yang, X.; Chen, G.; Qian, Y.; Wang, Y.; Zhai, Y.; Fan, D.; Xu, Y. Prediction of Myopia in Adolescents through Machine Learning Methods. Int. J. Env. Res. Public Health 2020, 17, 463.
- Li, S.M.; Ren, M.Y.; Gan, J.; Zhang, S.G.; Kang, M.T.; Li, H.; Atchison, D.A.; Rozema, J.; Grzybowski, A.; Wang, N. Machine Learning to Determine Risk Factors for Myopia Progression in Primary School Children: The Anyang Childhood Eye Study. Ophthalmol. Ther. 2022, 11, 573–585.
This entry is offline, you can click here to edit this entry!
