Sustainable design methods aim to obtain architectural solutions that assure the coexistence and welfare of human beings, inorganic structures, and living things that constitute ecosystems. The novel coronavirus emergence, inadequate vaccines against the present severe acute respiratory syndrome-coronavirus-(SARS-CoV-2), and increases in microbial resistance have made it essential to review the preventative approaches used during pre-antibiotic periods. Apart from low carbon emissions and energy, sustainable architecture for facilities, building designs, and digital modeling should incorporate design approaches to confront the impacts of communicable infections. This review aims to determine how architectural design can protect people and employees from harm; it models viewpoints to highlight the architects’ roles in combating coronavirus disease 2019 (COVID-19) and designing guidelines as a biomedical system for policymakers. The goals include exploring the hospital architecture evolution and the connection between architectural space and communicable infections and recommending design and digital modeling strategies to improve infection prevention and controls. Based on a wide-ranging literature review, it was found that design methods have often played important roles in the prevention and control of infectious diseases and could be a solution for combating the wide spread of the novel coronavirus or coronavirus variants or delta.
- risk assessment
- building design
- modeling
- COVID-19 pandemic
- SARS-CoV-2
- hospital architecture
1. Introduction
Sustainable architectures are integrating the inhabitants into natural environments and micro-environment controls and adopting efficient material resources and energy in buildings. Sustainable designs aim to foster the coexistence and welfare of human beings, inorganic elements, and living things that make up the ecosystem and find architectural responses [1][2][3]. An integral portion of infection inhibition and management mechanisms should be the hospital’s architectural design process. Apart from low carbon emissions and low energy, Van-Khai [4] supported the idea that the sustainable architecture purpose for health facility designs should incorporate design methods for the prevention and control of communicable infections. The World Health Organization (WHO) emphasizes that combating infectious diseases and protecting population centers from their spread is a scientific strategy, based on well-studied solutions aimed at preventing the health risks and harms caused by the infection of people and health workers [5]. Given the quick and ongoing changes in the healthcare environment in the context of advances in medicine, innovation, and strategic culture, this requires a strategy to operate the facilities throughout their lifespan [6]. It is also reported that the architectural designs of the hospitals took a significant share of the pandemic in the Tugela Ferry outbreak in South Africa in 2006, which showed the importance of facility design to expand hospitalization [7]. Hospitals must be built and designed using strong human-factor concepts; they must also be able to adapt to emerging problems and urgent demands, as well as accommodate future requirements, particularly when dealing with emergency situations such as COVID-19 [8][9][10][11]. The implications are that the well-being and health of humans are strongly linked with constructed environments. Based on the current reports from the disease control center regarding the Coronavirus transmission mode, it has become essential to balance the need for control measures and the open-access design concept to reduce the infection rates [12]. Modular and quick building, repurposing of places, and temporary setting equipment have all evolved as ways to address the pressing demand for adaptable and robust solutions [13][14]. Recent and past research has indicated that unstable climates and climate change play essential roles in driving global emergence, resurgence, and redistributions of communicable infections [15][16]. In addition to that, the climate’s continuous change has a significant impact on the constructed environments [17][18]. Today’s healthcare infrastructures are developed and built with the idea in mind that they should be important for a long lifetime, which does not allow for changes in service need on a regular basis [19].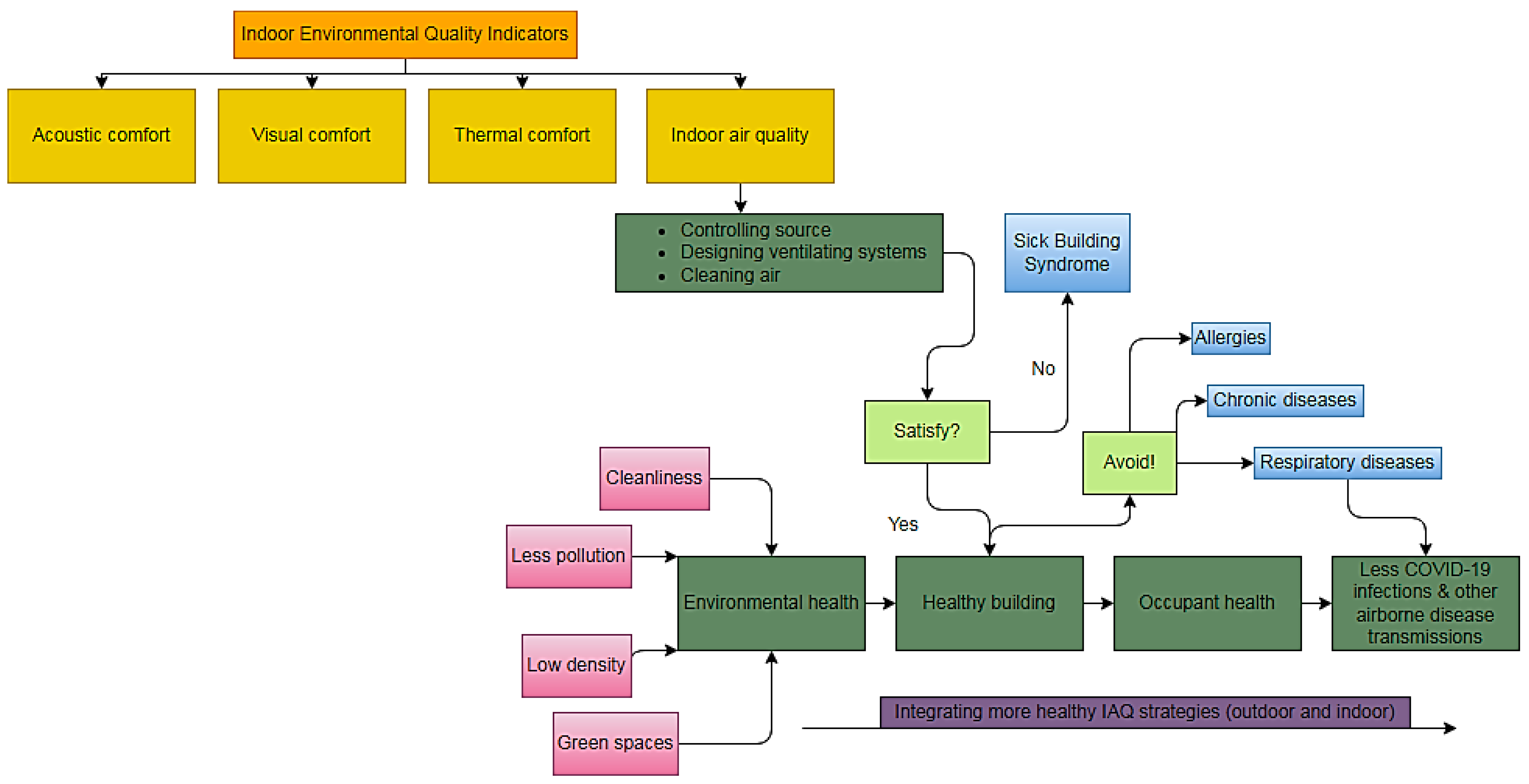
2. Controls, Mitigations, and Health Care Setting Special Consideration
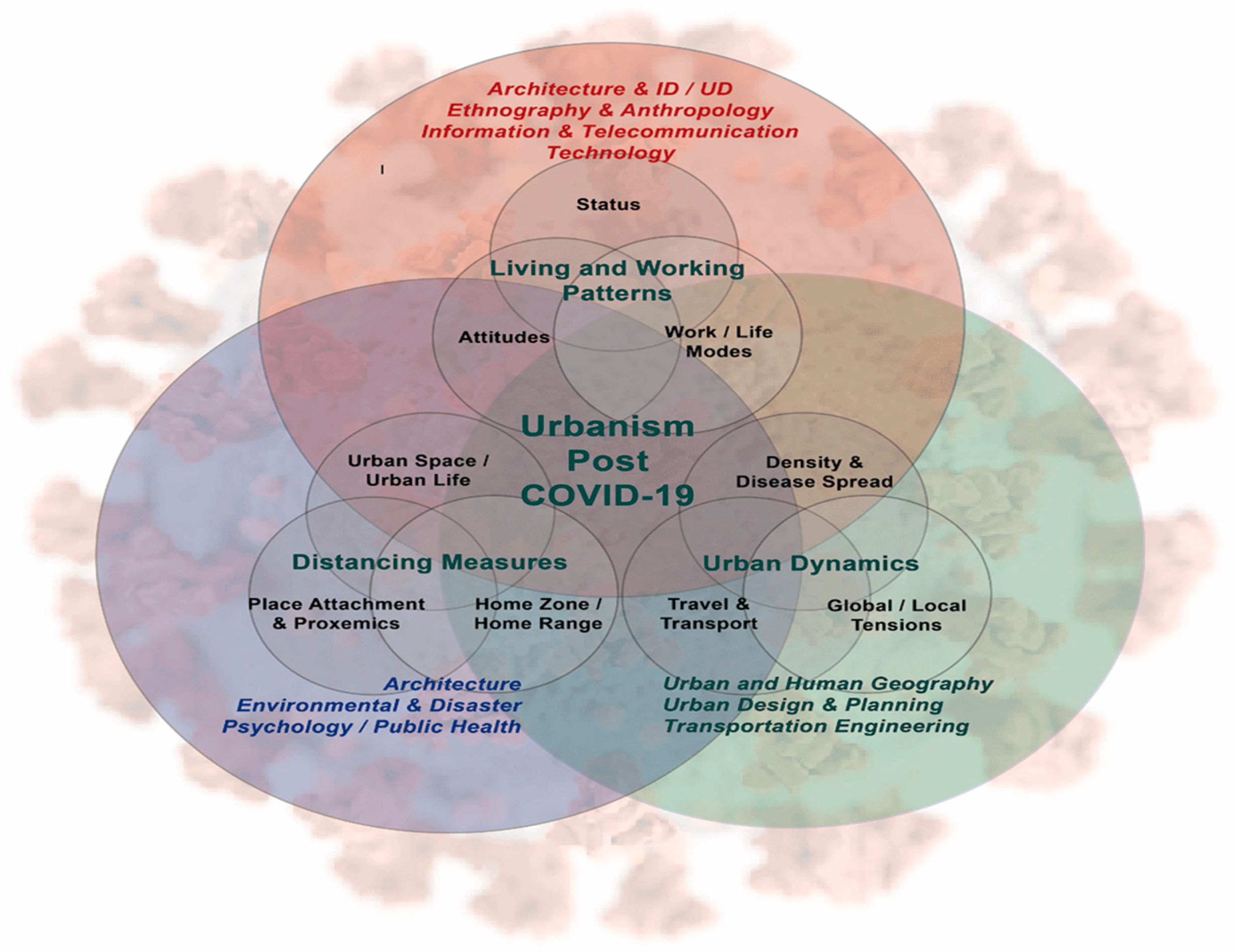
3. Architectural and Design Engineering for the Controls in Post-Pandemic
3.1. Future Human-Centered Design
3.2. In Post-COVID-19 Architectural Design: An Auxiliary Decision-Making Strategy
4. Proposed Roles by Real Estate to Mitigate Transmission of COVID-19
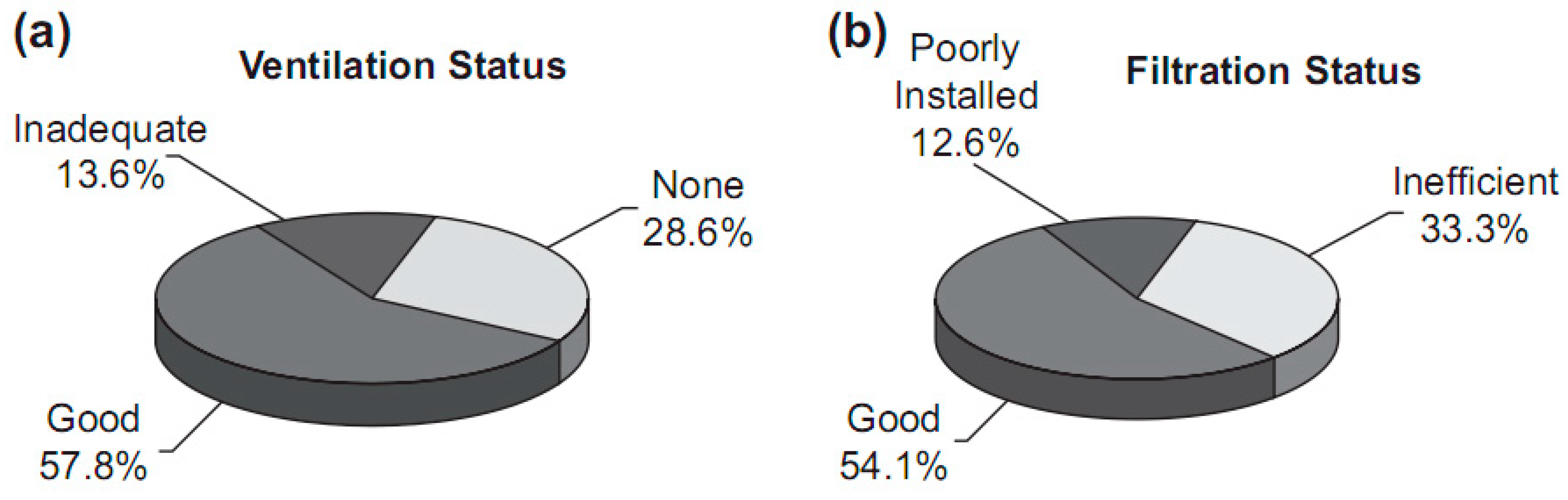
4.1. Purification of Indoor Air and Accentuating Ventilation of Buildings
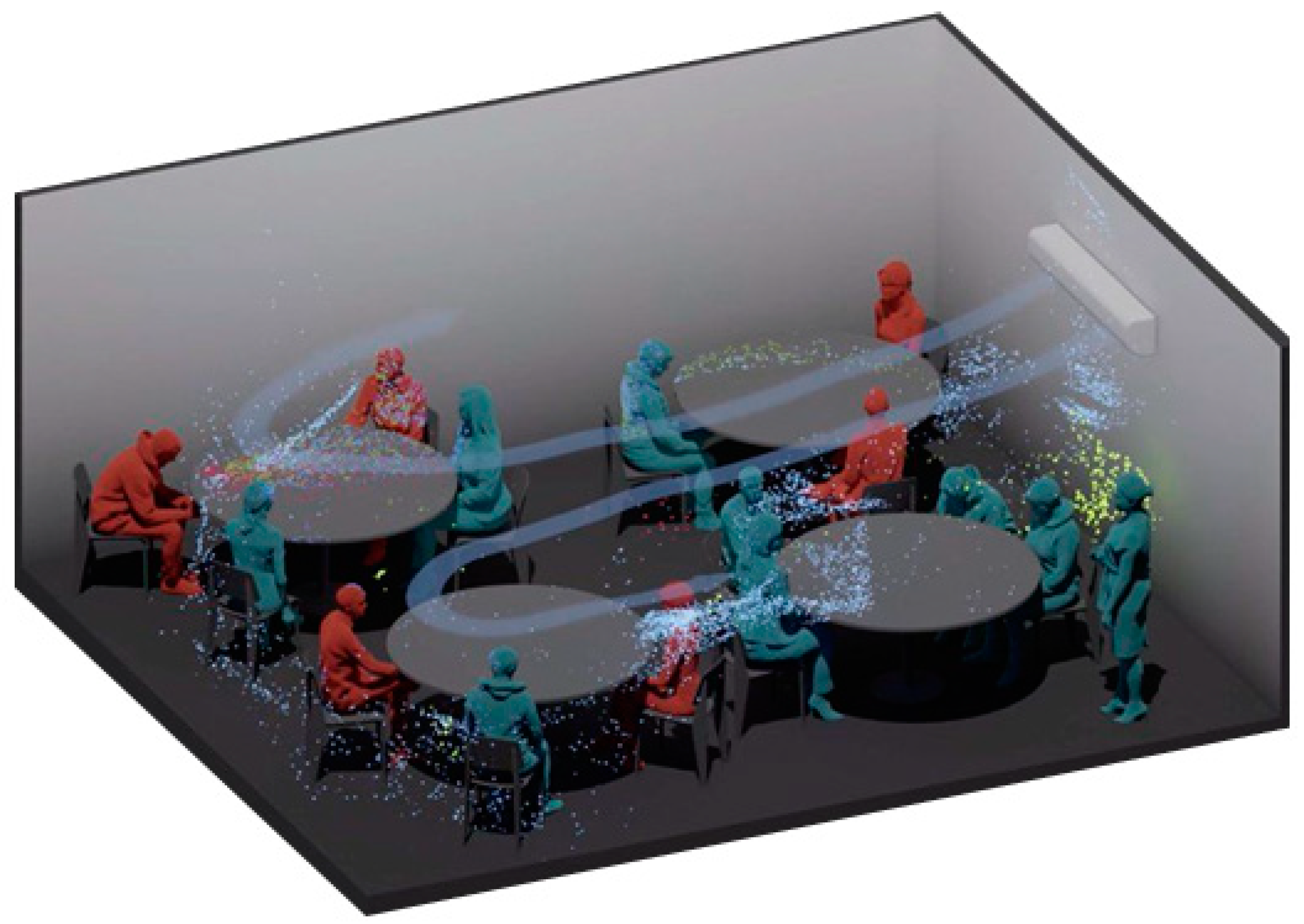
4.2. Airborne Dissemination
4.3. Preserving Optimal Humidity and Emphasizing Cleaning Protocols
This entry is adapted from the peer-reviewed paper 10.3390/buildings12050582
References
- Kim, J.-J.; Rigdon, B. Sustainable Architecture Module: Introduction to Sustainable Design; National Pollution Prevention Center for Higher Education: Ann Arbor, MI, USA, 1998.
- Fediuk, R.S.; Yevdokimova, Y.G.; Smoliakov, A.K.; Stoyushko, N.Y.; Lesovik, V.S. Use of geonics scientific positions for designing of building composites for protective (fortification) structures. IOP Conf. Ser. Mater. Sci. Eng. 2017, 221, 012011.
- Fediuk, R.S.; Lesovik, V.S.; Mochalov, A.V.; Otsokov, K.A.; Lashina, I.V.; Timokhin, R.A. Timokhin, Composite binders for concrete of protective structures. Mag. Civ. Eng. 2018, 6, 208–218.
- Van Khai, T. Adaptive Architecture and the Prevention of Infections in Hospitals. Civ. Eng. Ser. 2016, 16, 2016–2028.
- WHO. Infection Prevention and Control; World Health Organization: Geneva, Switzerland, 2020.
- Mauri, M. The future of the hospital and the structures of the NHS. TECHNE0-J. Technol. Arch. Environ. 2015, 9, 27–34.
- Alcorn, K. Tugela Ferry XDR-TB out Break Continues to Grow, but Treatment in KZN Provides Hope. Available online: https://www.aidsmap.com/news/nov-2007/tugela-ferry-xdr-tb-outbreak-continues-grow-treatment-kzn-provides-hope (accessed on 12 September 2020).
- Chisci, E.; Masciello, F.; Michelagnoli, S. The Italian USL Toscana Centro model of a vascular hub responding to the COVID-19 emergency. J. Vasc. Surg. 2020, 72, 8–11.
- Smolova, M.; Smolova, D. Emergency architecture. Modular construction of healthcare facilities as a response to pandemic outbreak. In E3S Web of Conferences, Proceedings of the 2nd International Scientific Conference on Socio-Technical Construction and Civil Engineering (STCCE-2021), Kazan, Russia, 21–28 April 2021; Vdovin, E., Ed.; EDP Sciences: Les Ulis, France, 2021; Volume 274, p. 01013.
- Romani, G.; Mas, F.D.; Massaro, M.; Cobianchi, L.; Modenese, M.; Barcellini, A.; Ricciardi, W.; Barach, P.; Lucà, R.; Ferrara, M. Population Health Strategies to Support Hospital and Intensive Care Unit Resiliency During the COVID-19 Pandemic: The Italian Experience. Popul. Health Manag. 2021, 24, 174–181.
- Ali, M.; de Azevedo, A.; Marvila, M.; Khan, M.; Memon, A.; Masood, F.; Almahbashi, N.; Shad, M.; Khan, M.; Fediuk, R.; et al. The Influence of COVID-19-Induced Daily Activities on Health Parameters—A Case Study in Malaysia. Sustainability 2021, 13, 7465.
- Lateef, F. Hospital design for better infection control. J. Emergencies Trauma Shock 2009, 2, 175–179.
- Brown, O.D.R.; Hennecke, R.P.; Nottebrock, D. Vancouver Convention Health Centre (COVID-19 Response): Planning, implementation, and four lessons learned. Am. J. Disaster Med. 2020, 15, 143–148.
- Marinelli, M. Emergency Healthcare Facilities: Managing Design in a Post Covid-19 World. IEEE Eng. Manag. Rev. 2020, 48, 65–71.
- A Volodchenko, A.; Lesovik, V.S.; A Cherepanova, I.; Zagorodnjuk, L.H.; Elistratkin, M.Y.; Volodchenko, A.N. Peculiarities of non-autoclaved lime wall materials production using clays. IOP Conf. Ser. Mater. Sci. Eng. 2018, 327, 022021.
- Chernysheva, N.; Lesovik, V.; Fediuk, R.; Vatin, N. Improvement of Performances of the Gypsum-Cement Fiber Reinforced Composite (GCFRC). Materials 2020, 13, 3847.
- Wu, X.; Lu, Y.; Zhou, S.; Chen, L.; Xu, B. Impact of climate change on human infectious diseases: Empirical evidence and human adaptation. Environ. Int. 2016, 86, 14–23.
- Marlene, C. Infectious Diseases Likes It Hot: How Climate Change Helps Cholera and Salmonella. Available online: https://www.nationalnursesunited.org/news/infectious-diseases-it-hot-how-climate-change-helps-cholera-and-salmonella-outbreaks (accessed on 17 September 2021).
- de Neufville, R.; Lee, Y.S.; Scholtes, S. Flexibility in Hospital Infrastructure Design. In Proceedings of the 2008 First International Conference on Infrastructure Systems and Services: Building Networks for a Brighter Future (INFRA), Rotterdam, The Netherlands, 10–12 November 2008.
- Filippini, T.; Rothman, K.J.; Goffi, A.; Ferrari, F.; Maffeis, G.; Orsini, N.; Vinceti, M. Satellite-detected tropospheric nitrogen dioxide and spread of SARS-CoV-2 infection in Northern Italy. Sci. Total Environ. 2020, 739, 140278.
- WHO/Europe. WHO Guidelines for Indoor Air Quality: Selected Pollutants; World Health Organization Regional Office for Europe: Copenhagen, Denmark, 2010.
- Wang, Z.; Zhang, J.S. Characterization and performance evaluation of a full-scale activated carbon-based dynamic botanical air filtration system for improving indoor air quality. Build. Environ. 2011, 46, 758–768.
- Chan, I.Y.; Liu, A.M. Effects of neighborhood building density, height, greenspace, and cleanliness on indoor environment and health of building occupants. Build. Environ. 2018, 145, 213–222.
- Van Den Berg, A.E.; Maas, J.; Verheij, R.A.; Groenewegen, P.P. Green space as a buffer between stressful life events and health. Soc. Sci. Med. 2010, 70, 1203–1210.
- Gould, I. Antibiotic resistance: The perfect storm. Int. J. Antimicrob. Agents 2009, 34, S2–S5.
- Kubba, S. Chapter Seven–Indoor Environmental Quality. In LEED v4 Practices, Certification, and Accreditation Handbook, 2nd ed.; Butterworth-Heinemann: Oxford, UK, 2016; pp. 303–378.
- Wallin, A.; Lukšienė, Ž.; Žagminas, K.; Šurkienė, G. Public Health and Bioterrorism: Renewed Threat of Anthrax and Smallpox. Medicina 2007, 43, 278–284.
- Fleck, F. Conference warns of danger of re-emergence of smallpox as weapon of bioterror. Bull. World Health Organ. 2003, 81, 917.
- Van Doremalen, N.; Bushmaker, T.; Morris, D.H.; Holbrook, M.G.; Gamble, A.; Williamson, B.N.; Tamin, A.; Harcourt, J.L.; Thornburg, N.J.; Gerber, S.I.; et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N. Engl. J. Med. 2020, 382, 1564–1567.
- Elistratkin, M.; Minakov, S.; Shatalova, S. Composite binding mineral additive influence on the plasticizer efficiency. Constr. Mater. Prod. 2019, 2, 10–16.
- Evelson, L.; Lukuttsova, N. Application of statistical and multi fractalmodels for parameters optimization of nano-modified concrete. Int. J. Appl. Eng. Res. 2015, 10, 12363–12370.
- Rucka, M.; Wojtczak, E.; Knak, M.; Kurpińska, M. Characterization of fracture process in polyolefin fibre-reinforced concrete using ultrasonic waves and digital image correlation. Constr. Build. Mater. 2021, 280, 122522.
- Leventsov, V.; Gluhov, V.; Leventcov, A. Investment attractiveness of the telecommunications economic sector during the coronavirus pandemic. In Internet of Things, Smart Spaces, and Next Generation Networks and Systems; Springer: Cham, Germany, 2020; pp. 285–296.
- Salama, A.M. Coronavirus questions that will not go away: Interrogating urban and socio-spatial implications of COVID-19 measures. Emerald Open Res. 2020, 2, 14.
- Bolashikov, Z.; Melikov, A.; Bolashikov, Z.; Melikov, A. Methods for air cleaning and protection of building occupants from airborne pathogens. Build. Environ. 2009, 44, 1378–1385.
- Rassia, S.T. How Architecture Fails in Conditions of Crisis: A Discussion on the Value of Interior Design over the COVID-19 Outbreak. Oper. Res. Forum 2020, 1, 1–3.
- Brittain, O.S.; Wood, H.; Kumar, P. Prioritising Indoor Air Quality in Building Design Can Mitigate Future Airborne Viral Outbreaks. Cities Health. Available online: https://www.tandfonline.com/doi/full/10.1080/23748834.2020 (accessed on 28 September 2021).
- Zhao, B.; Liu, Y.; Chen, C. Air purifiers: A supplementary measure to remove airborne SARS-CoV-2. Build. Environ. 2020, 177, 106918.
- Cummings, B.E.; Waring, M.S. Potted plants do not improve indoor air quality: A review and analysis of reported VOC removal efficiencies. J. Expos. Sci. Environ. Epidemiol. 2020, 30, 253–261.
- Yu, C.W.F.; Kim, J.T. Building Environmental Assessment Schemes for Rating of IAQ in Sustainable Buildings. Indoor Built Environ. 2011, 20, 5–15.
- Megahed, N.A.; Ghoneim, E.M. Indoor Air Quality: Rethinking rules of building design strategies in post-pandemic architecture. Environ. Res. 2020, 193, 110471.
- Hassan, A.M.; El Mokadem, A.A.F.; Megahed, N.A.; Eleinen, O.M.A. Improving outdoor air quality based on building morphology: Numerical investigation. Front. Arch. Res. 2020, 9, 319–334.
- Hassan, A.M.; Elmokadem, A.A.; Megahed, N.A.; Eleinen, O.M.A. Urban morphology as a passive strategy in promoting outdoor air quality. J. Build. Eng. 2020, 29, 101204.
- Mangili, A.; Gendreau, M.A. Transmission of infectious diseases during commercial air travel. Lancet 2005, 365, 989–996.
- Aliabadi, A.A.; Rogak, S.N.; Bartlett, K.H.; Green, S.I. Preventing Airborne Disease Transmission: Review of Methods for Ventilation Design in Health Care Facilities. Adv. Prev. Med. 2011, 2011, 1–21.
- Qian, H.; Li, Y.; Seto, W.H.; Ching, P.; Ching, W.H.; Sun, H.Q. Natural Ventilation for reducing Airborne Infection in Hospital. Build. Environ. 2010, 45, 1651–1658.
- Atkinson, J.; Chartier, Y.; Lúcia Pessoa-Silva, C.; Jensen, P.; Li, Y.; Seto, W.-H. Natural Ventilation for Infection Control in Health-Care Settings; World Health Organization: Geneva, Switzerland, 2016.
- Smieszek, T.; Lazzari, G.; Salathé, M. Assessing the Dynamics and Control of Droplet- and Aerosol-Transmitted Influenza Using an Indoor Positioning System. Sci. Rep. 2019, 9, 1–10.
- Bischoff, W.E.; Swett, K.; Leng, I.; Peters, T.R. Exposure to Influenza Virus Aerosols During Routine Patient Care. J. Infect. Dis. 2013, 207, 1037–1046.
- ASHRAE. ASHRAE Position Document on Infectious Aerosols; ASHRAE: Atlanta, GA, USA, 2020.
- Baron, P. Generation and Behavior of Airborne Particles (Aerosols); Centers for Disease Control and Prevention: Atlanta, GA, USA, 2020.
- Yan, J.; Grantham, M.; Pantelic, J.; de Mesquita, P.J.B.; Albert, B.; Liu, F.; Ehrman, S.; Milton, D.K.; Adamson, W.; Beato-Arribas, B.; et al. Infectious virus in exhaled breath of symptomatic seasonal influenza cases from a college community. Proc. Natl. Acad. Sci. USA 2018, 115, 1081–1086.
- Li, Y. The secret behind the mask. Indoor Air 2011, 21, 89–91.
- Siegel, J.D.; Rhinehart, E.; Jackson, M.; Chiarello, L.; the Healthcare Infection Control Practices Advisory Committee. 2007 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2007.
- Reiman, J.M.; Das, B.; Sindberg, G.M.; Urban, M.D.; Hammerlund, M.E.M.; Lee, H.B.; Spring, K.M.; Lyman-Gingerich, J.; Generous, A.R.; Koep, T.H.; et al. Humidity as a non-pharmaceutical intervention for influenza A. PLoS ONE 2018, 13, e0204337.
- Tuladhar, E.; Hazeleger, W.C.; Koopmans, M.; Zwietering, M.H.; Beumer, R.R.; Duizer, E. Residual Viral and Bacterial Contamination of Surfaces after Cleaning and Disinfection. Appl. Environ. Microbiol. 2012, 78, 7769–7775.
