Coronavirus disease 2019 (COVID-19) patients can develop interstitial pneumonia, which, in turn, can evolve into acute respiratory distress syndrome (ARDS). This is accompanied by an inflammatory cytokine storm. severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2) has proteins capable of promoting the cytokine storm, especially in patients with comorbidities, including obesity. Since currently no resolutive therapy for ARDS has been found and given the scientific literature regarding the use of adenosine, its application has been hypothesized. Through its receptors, adenosine is able to inhibit the acute inflammatory process, increase the protection capacity of the epithelial barrier, and reduce the damage due to an overactivation of the immune system, such as that occurring in cytokine storms. These features are known in ischemia/reperfusion models and could also be exploited in acute lung injury with hypoxia. Considering these hypotheses, a COVID-19 patient with unresponsive respiratory failure was treated with adenosine for compassionate use. The results showed a rapid improvement of clinical conditions, with negativity of SARS-CoV2 detection.
- COVID-19
- ARDS
- Adenosine
- CT-scan
- Cytokines Storm
Introduction
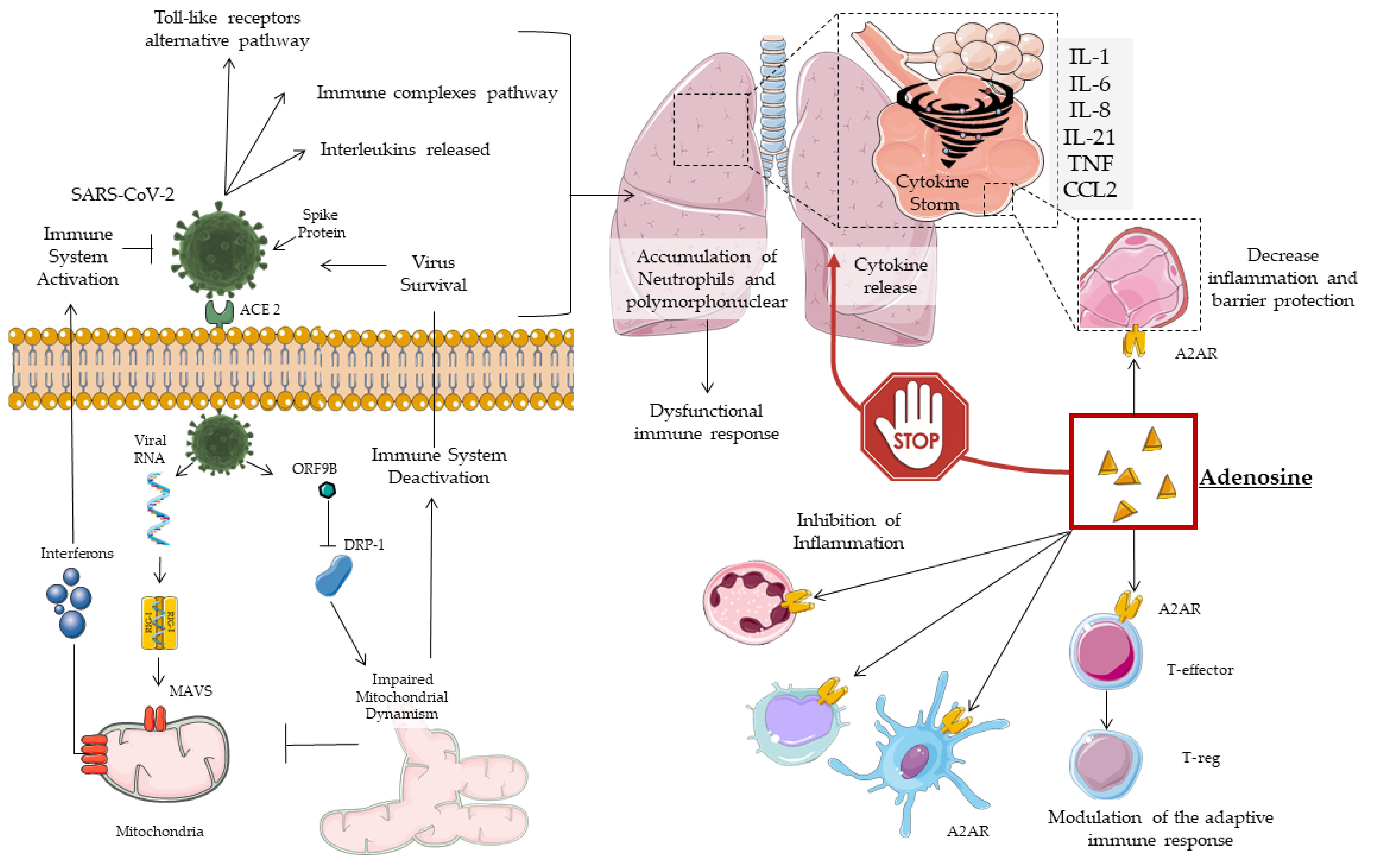
The current coronavirus disease 2019 (COVID-19) outbreak has been declared a pandemic by the World Health Organization (WHO), reporting more than 13 million new cases worldwide with 572,539 related deaths [1]. Part of these patients develops interstitial pneumonia, which can, in turn, evolve into acute respiratory distress syndrome (ARDS). ARDS patients require active hyperoxic ventilation, with mainly fatal outcomes [2]. The pathogenesis of COVID-19-related lung injury is still unclear and under study, but the cytokine storm is a severe event with a poor prognosis [2]. For this reason, various drugs have been tested to block such storm. Dramatically, over 50% of COVID-19 patients needed respiratory support. Studies have shown that some lung complications are due to iatrogenic injury [3]. A previous preclinical study using an animal model [3] observed that oxygenation inhibits the physiological mechanism of protection of the tissues, and this could aggravate ARDS. For this reason, the role of the puraminergic system in preventing respiratory complications in COVID-19 has been investigated. In fact, respiratory support to the COVID-19 patient could contribute to the inhibition of the adenosine pathway mediated by the A2A receptor (A2AR). This pathway involves shutting down the acute inflammatory process in cases of hypoxia.
2. Cytokine Storm
The high mortality in COVID-19 patients has been closely related to the cytokine storm. This is an excessive immune response, with a complex pathogenesis, determining rapid progression and high mortality from the disease [2]. Curiously, numerous patients who quickly died of ARDS did not experience severe symptoms in the early stages of the disease but only the common mild ones.
The cytokine storm is among the causes of ARDS and multi organ failure (MOF) and is detected in COVID-19 patients [2]. It is clear that in critically ill COVID-19 patients, the pathogenesis is promoted by a specific proinflammatory response. In vitro experiments have shown that in the early stage of a SARS-CoV infection, infected cells (respiratory epithelial cells, dendritic cells, and macrophages) delay the release of cytokines and chemokines [20,21,22]. Subsequently, antiviral molecules belonging to the interferon family are secreted at low concentrations, while proinflammatory cytokines (IL-1β, IL-6, tumor necrosis factor (TNF)-α, and chemokines are widely released [20,21,22].
In previous coronavirus epidemics, high levels of cytokines and chemokines in infected patients have been observed. In particular, a high number of neutrophils and monocytes in the bloodstream and lungs have been detected [23,24,25,26]. At the same time, the delay in interferon secretion results in a reduced and altered antiviral response. Interferons represent the molecular key of the human body defense against virus infection [27].
Afterwards, the high level of cytokines and chemokines determines the infiltration of numerous inflammatory cells into the lung tissue, such as lymphocytes, monocytes, and macrophages. A greater deregulation has already been observed in older primates and other animal models [28].
In hCoV infection, the ARDS determinants are the delay in the antiviral response, the secretion of cytokines, chemokines, granulocyte-macrophage colony-stimulating factor, reactive oxygen species, chemokines, and cell apoptosis products [29]. All this causes apoptosis of the endothelium and pulmonary epithelium, destruction of the respiratory barrier, and vascular leakage with alveolar edema [30].
A positive correlation between cytokine levels and disease severity was also found in COVID-19 patients, with non-specific recruitment of inflammatory cells. In addition to the pro-inflammatory molecules described so far, COVID-19 patients also showed a reduced presence of anti-inflammatory cytokines, with an imbalance in favor of the former [17] (Figure 1).
In COVID-19, obesity and related-comorbidities increase the risk of intensive care unit (ICU) hospitalization and death. This occurs due to a rise in inflammation status, impaired immune response, and respiratory dysfunction [30,31,32,33,34,35]. Obesity has been shown to be an independent risk factor in young males [36]. Metabolic syndrome, frequent in obesity, promotes the cytokine storm [35,36]. Diabetes mellitus, due to hyperglycemia, impairs the immune response and acts to ACE2 glycosylation [37,38], favoring the infection and pathogenesis of SARS-CoV-2 [39].
In summary, obesity and its comorbidities increase the patient’s inflammatory status, resulting in a higher inflammation set-point and susceptibility to infection. This phenomenon has been called immuno-innate memory and is attributable to epigenetic changes that we know to be influenced by the environment, lifestyle, and poor nutrition [40]. In COVID-19, all these factors predispose to an immune dysfunction that leads to increased respiratory complications. Hence, the importance of anti-inflammatory therapy, such as adenosine, as well as antivirals is highlighted.
3. Conclusions
Coronavirus disease 2019 (COVID-19) patients can develop interstitial pneumonia, which, in turn, can evolve into acute respiratory distress syndrome (ARDS). This is accompanied by an inflammatory cytokine storm. severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2) has proteins capable of promoting the cytokine storm, especially in patients with comorbidities, including obesity. Since currently no resolutive therapy for ARDS has been found and given the scientific literature regarding the use of adenosine, its application has been hypothesized. Through its receptors, adenosine is able to inhibit the acute inflammatory process, increase the protection capacity of the epithelial barrier, and reduce the damage due to an overactivation of the immune system, such as that occurring in cytokine storms. These features are known in ischemia/reperfusion models and could also be exploited in acute lung injury with hypoxia. Considering these hypotheses, a COVID-19 patient with unresponsive respiratory failure was treated with adenosine for compassionate use. The results showed a rapid improvement of clinical conditions, with negativity of SARS-CoV2 detection.
This entry is adapted from the peer-reviewed paper 10.3390/jcm9093045
