Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Coronavirus belongs to the vast group of viruses, under the family Coronaviridae with the subfamily of Ortocoronavirinae found in the order Nidovirales and realm Riboviria.
- SARS-CoV-2
- pandemic
- economy
- climate
- SDGs
1. Human Coronaviruses
Four groups of genera are classified for coronaviruses, i.e., Alpha, Beta, Gama, and Delta. Among these, Alpha and Beta capture mammals, whereas Gamma and Delta are responsible for birds. There are seven known segments of human coronaviruses (Table 1), out of which four are found to be of mild symptoms similar to the common cold, and three are respectively severe in nature [1][2].
Table 1. Classification of Human coronavirus at its critical bar.
| Type (Coronaviruses) | Symptoms | Classified |
|---|---|---|
| 1 | Mild | Human coronavirus OC43 (HCoV-OC43) |
| 2 | Mild | Human coronavirus HKU1 |
| 3 | Mild | Human coronavirus NL63 (HCoV-NL63, New Haven coronavirus) |
| 4 | Mild | Human coronavirus 229E (HCoV-229E) |
| 5 | Severe | The Middle East respiratory syndrome-related coronavirus (MERS-CoV) |
| 6 | Severe | Severe acute respiratory syndrome coronavirus (SARS-CoV or “SARS-classic”) |
| 7 | Severe | Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) |
In the initial phase of the outbreak, Chinese authorities identified an individual with pneumonia hospitalized in Wuhan. Afterwards, authorities precluded SARS-CoV, MERS-CoV, influenza, avian influenza, adenovirus, and the rest of the common respiratory pathogens [3][4]. Initially, the name given to this pandemic by World Health Organization (WHO) was 2019-nCoV, but in the later phase of surveillance it was renamed as SARS-CoV-2 by the International Committee on Taxonomy of Viruses. There is a significant risk factor in coronaviruses that varies widely at its bar. Death rate varies broadly from 0 to 30% in the common cold and MERS-CoV, respectively. Symptoms of SARS-CoV-2 were found to be cough, high fever, and shortness of breath. Its transmission is from person to person through droplets of cough and sneeze from the infected source. It can be potentially severe, and in some cases, it can claim human life [5].
1.1. Taxonomy and Classification
Coronavirus belongs to the vast group of viruses, from under the family Coronaviridae with the subfamily of Ortocoronavirinae found in the order Nidovirales and realm Riboviria. The crown-like viral particle enveloping CoVs lends it its name: coronavirus. On the way to RNA synthesis or host response modulation, the involvement of polymerase (RdRp) and other non-structural proteins are enumerated [6][7]. The diameter of the virion in coronaviruses is enumerated as approximately 120 nm, with the surface projection of club-shaped protein. There are four canonical structural proteins found in coronaviruses: the outer biggest transmembrane spike protein (S), followed by small envelope protein (E), membrane (M), and nucleocapsid (N) and some accessory proteins [8].
1.2. Novelty of SARS-CoV-2 in Contrast with Earlier Outbreak
In the wake of rapid transmission, the last two decades were dominated by major zoonotic coronaviruses that claimed thousands of human lives. In 2002, typical pneumonia was reported called severe acute respiratory syndrome (SARS), which marked the first pandemic of the 21st century, with its origin and epicenter in Southern China (Guangdong). It started on 16 November 2002 and ended in July 2003; its incubation period was 2 to 7 days, which was measured to be less effective in comparison with the rest of the viruses. It spread to approximately 30 countries including China, with 8422 reported cases and fatalities around 916, which promptly bothered the WHO enough to announce it as a worldwide health threat [9]. During the SARS outbreak, it was considered that the virus-host was the bat and that it had the ability to jump over another, which mutated in such a way that it could infect another intermediate host, probably civet [10]. The intermediate host, later on, made all the differences and mutated to humans [9][11][12].
A decade later, it happened again. Now the epicenter of the virus found a new spot in Saudi Arabia, which spread its wings in the peak period of March 2014 and folded back by the end of 2015. The very first case of Middle East respiratory syndrome (MERS-CoV) was reported in Saudi Arabia in June 2012. From then till October 2018, 2260 confirmed cases were reported, with 803 fatalities. The cases flourished in 27 countries, with Saudi Arabia alone contributing 71% of cases [13]. At the emergence of the SARS-CoV-2 outbreak, the case fatality rate (CFR) was higher (approximately 35%) because of its novelty and lack of preparedness, but as the time passed, the decline in CFR was marked, which was controlled mainly by vaccination and herd immunity, and it came down to 1.35%. Its fatality rate was comparably higher than the rest of the viruses, which was estimated at around 35%, and the bat reservoir had enough capability to mutate to the animal reservoir (Table 2), with the result being that it has been found that it mutated to the camel as an intermediate host [14][15].
Table 2. Illustrates the distinction among recent bat-borne coronaviruses.
| Viruses | Source | Mediator | Acceptor | Case Fatality Rate | Incubation Period | Reference |
|---|---|---|---|---|---|---|
| SARS (2002) | Bat | Civet | Human | 916/8422 × 100 = 10.8% | 2–7 days | [12][14] |
| MERS (2012) | Bat | Camel | Human | 850/2500 × 100 = 34% | 2–14 days | [10][16] |
| COVID (2019) | Bat | Pangolin | Human | 6.1 M/444.12 M × 100 = 1.35% † | 2–14 days (still uncertain) | [17][18] |
(† Case fatality rate is calculated as of 5 March 2022, with the available data provided by coronavirus world meter; these figures may vary as the containment time increases).
The emergence of a novel coronavirus SARS-CoV-2 brings back the images of SARS-CoV from two decades ago—a déjà vu—as if researchers were looking into a rear-view mirror. In 2019 during the nCoV outbreak, it was being estimated that the bat reservoir mutated enough and directly jumped into humans, but in some studies, it has been enumerated that the bat virus initially mutated to angolin and then passed on to humans [17]. The basic reproduction number was calculated in Wuhan and in the Diamond Princess cruise to understand the passage of virus with the help of the exponential growth model method, and it was found to be in the range of 2.24–3.58 [15][19]. This was certainly not the end, and changes took place in the genetic sequence, which gave rise to mutation. Subsequently, differences in the genetic sequence came out with several variants. The WHO has listed variants of concern (VOC) that emerged from the outbreak; Alpha, Beta, Gamma, Delta, and Omicron were the most prominent ones that triggered the major waves across the globe [9][20][21].
2. Revolutionizing Epidemic to Pandemic
The first two phases of distribution were relatively marginal as the cases started emerging from one to another. The reproductive number (Ro) for the COVID cases was found to be in the range of 1–3; later on, there was a debate in the scientific community with regard to the fluctuation of range.
The novel strain of the coronavirus was considered to have originated from the fish market or wet market of Hubei province; since the virus was novel, the people were not aware of the gravity of this pandemic. The disease was initially found to be of virus-induced pneumonia symptoms as per the report of clinicians, with the additional symptoms of rising body temperature and depletion in the lymphocytes number and white blood cells [22]. In the initial phase of the outbreak, Japan and Thailand were registering their presence in the death marathon, and suddenly Diamond Princess started raising its hand, and South Korea came into the picture. Now, one could see the panicked faces of other countries. It was certain that no one was prepared enough to tackle the situation, which was worsening day by day. The prime concern about this virus was the incubation period (3–14 days), which usually occurs before the symptoms start to begin. Still, the majority of the population were busy in solving the conspiracy puzzle of whether it was a manufactured virus in the laboratory or a natural one, rather than being busy in solving how to contain it. On 11 March, the WHO announced this outbreak as a COVID-19 global pandemic. During the first wave, China was exasperated by trying to contain the virus, and it was recorded as the first country with the maximum number of active cases. However, from the second wave onwards to the present, the US overtook the race with a massive margin and even now the US holds the first position in the chart (Figure 1).
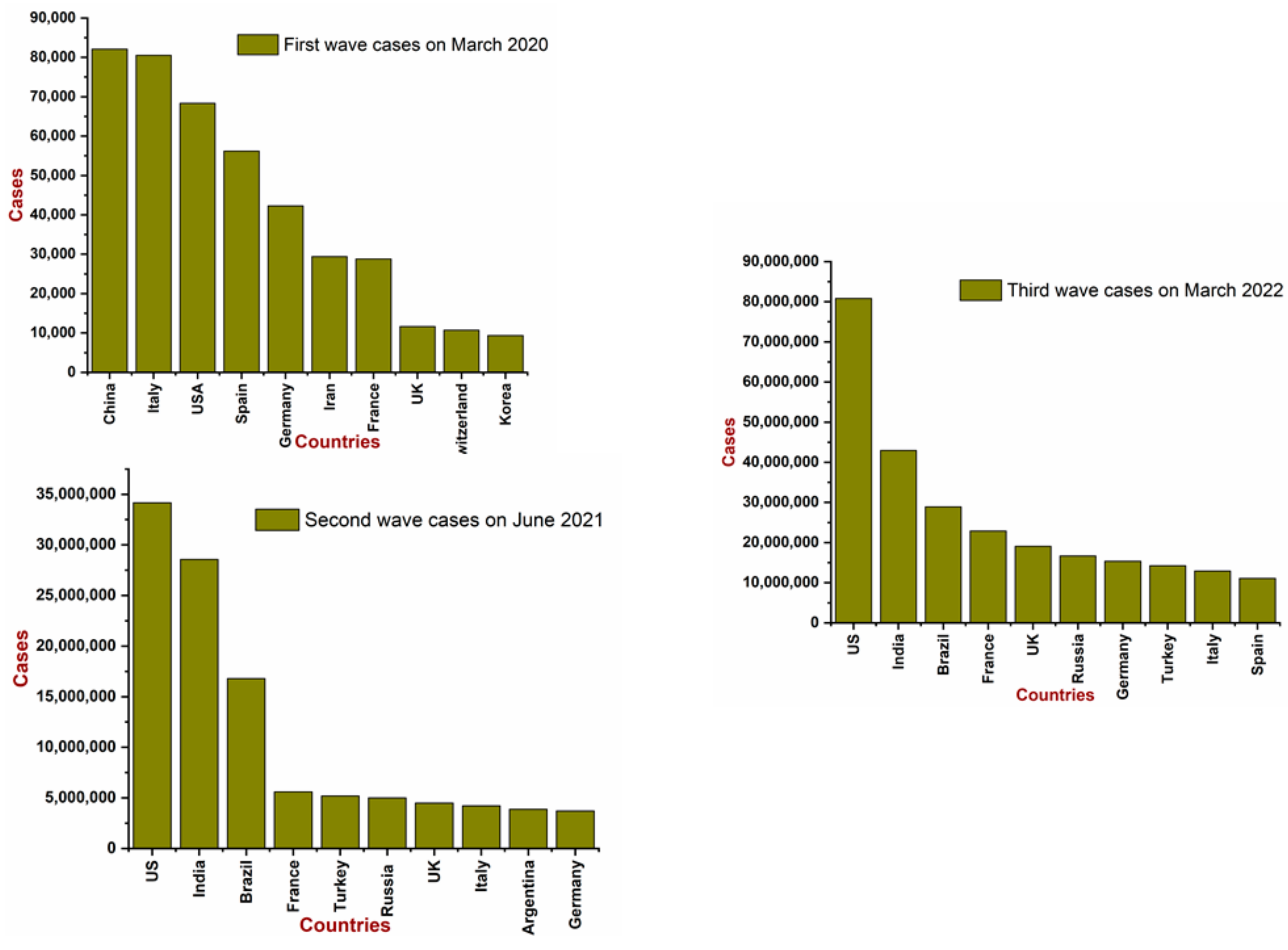 Figure 1. Migration of COVID-19 across the globe (Data source: Worldometer and WHO).
Figure 1. Migration of COVID-19 across the globe (Data source: Worldometer and WHO).So far, India and South Korea were praised by the rest of the world for containing the virus through their proactive approaches. India had taken an early decision of country lockdown, keeping in view the vulnerable health care system and the vast population, because social distancing and preventive measures seem to be very hazy in these circumstances. On the other side, African countries were so far untouched by this pandemic, but they were in a worrying situation because of a healthcare system unprepared to cope with the coronavirus pandemic. With an 11 million population, the nation of South Sudan has five vice presidents and four ventilators; 10 African countries do not have a single ventilator [23][24].
This entry is adapted from the peer-reviewed paper 10.3390/life12040520
This entry is offline, you can click here to edit this entry!
