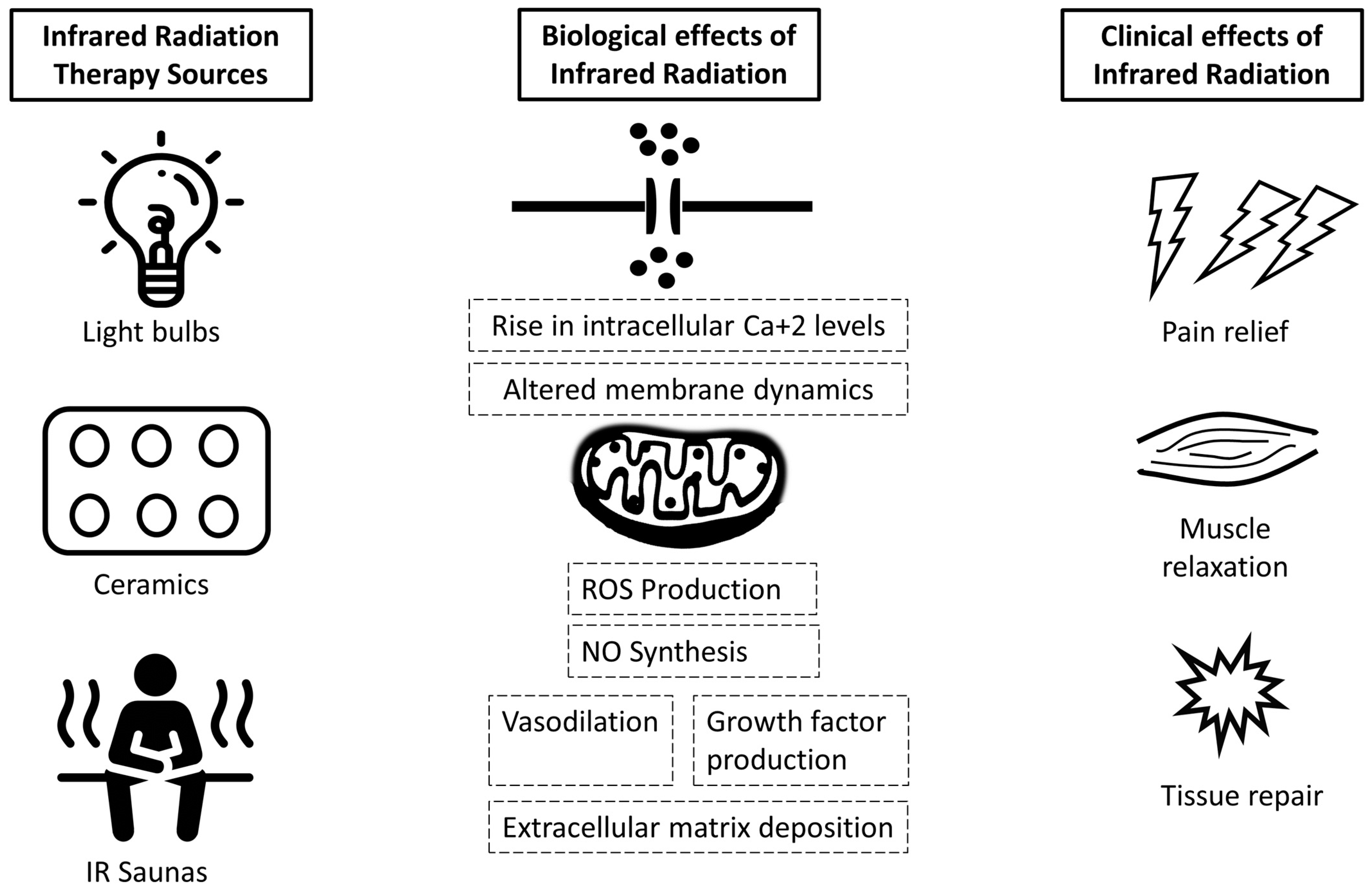
Infrared radiation (IR), also known as infrared light, consists of electromagnetic radiation with wavelengths but shorter than microwave radiation and longer than visible light (750 nm to 1 mm). IR derives from thermal energy; hence, material bodies emitting heat can produce it. Higher temperatures lead to the production of higher amounts of IR of higher frequency and shorter wavelength. IR consists of a promising complementary treatment for a wide range of musculoskeletal conditions, including knee osteoarthritis, fibromyalgia, chronic low back pain, chronic myofascial syndrome, sacroiliitis, and Gulf War Illness. Infrared therapy can be delivered with light-emitting devices (photobiomodulation), wires, ceramic materials, and IR saunas. In a number of studies, infrared therapy has also been associated with clinical and perceptual improvement in chronic-pain-related psychosomatic symptoms such as fatigue and insomnia.
- infrared phototherapy
- musculoskeletal conditions
- low back pain
- osteoarthritis
1. Introduction
1.1. Production and Provision of IR in Clinical Settings
1.2. Effects of Infrared Light on Health
2. Infrared Radiation in the Management of Musculoskeletal Conditions
3. Conclusions
This entry is adapted from the peer-reviewed paper 10.3390/ejihpe12030024
References
- Tsagkaris, C.; Corriero, A.C.; Moysidis, D.V.; Loudovikou, A.; Papazoglou, A.S. Knowing When Not to Operate: Following the Footsteps of Demokidis of Crotone in Orthopaedics. Surg. Innov. 2021, 13, 15533506211041903.
- Robertson, V.; Ward, A.; Low, J.; Reed, A. Infrared and visible radiations. In Electrotherapy Explained Principles and Practice, 2nd ed.; John Low & Ann Reed: Oxford, UK, 1994.
- Vatansever, F.; Hamblin, M.R. Far Infrared Radiation (FIR): Its Biological Effects and Medical Applications. Photonics Lasers Med. 2012, 4, 255–266.
- Meng, J.; Jin, W.; Liang, J.; Ding, Y.; Gan, K.; Yuan, Y. Effects of Particle Size on Far Infrared Emission Properties of Tourmaline Superfine Powders. J. Nanosci. Nanotechnol. 2010, 10, 2083–2087.
- Bundesamt fur Strahlenschutz , Applications of Infrared Radiation. 2020. Available online: https://www.bfs.de/EN/topics/opt/application-medicine-wellness/infrared/infrared_node.html (accessed on 16 October 2021).
- Lee, M.-S.; Baletto, F.; Kanhere, D.G.; Scandolo, S. Far-Infrared Absorption of Water Clusters by First-Principles Molecular Dynamics. J. Chem. Phys. 2008, 128, 214506.
- Chung, H.; Dai, T.; Sharma, S.K.; Huang, Y.-Y.; Carroll, J.D.; Hamblin, M.R. The Nuts and Bolts of Low-Level Laser (Light) Therapy. Ann. Biomed. Eng. 2012, 40, 516–533.
- Golovynska, I.; Golovynskyi, S.; Stepanov, Y.V.; Stepanova, L.I.; Qu, J.; Ohulchanskyy, T.Y. Red and near-infrared light evokes Ca2+ influx, endoplasmic reticulum release and membrane depolarization in neurons and cancer cells. J. Photochem. Photobiol. B 2021, 214, 112088.
- Hamblin, M.R. Mechanisms and Mitochondrial Redox Signaling in Photobiomodulation. Photochem. Photobiol. 2018, 94, 199–212.
- Lee, D.; Seo, Y.; Kim, Y.W.; Kim, S.; Bae, H.; Choi, J.; Lim, I.; Bang, H.; Kim, J.H.; Ko, J.H. Far-infrared radiation stimulates platelet-derived growth factor mediated skeletal muscle cell migration through extracellular matrix-integrin signaling. Korean J. Physiol. Pharmacol. 2019, 23, 141–150.
- Matsushita, K.; Masuda, A.; Tei, C. Efficacy of Waon Therapy for Fibromyalgia. Intern. Med. 2008, 47, 1473–1476.
- Lin, L.; Cheng, K.; Tan, M.T.; Zhao, L.; Huang, Z.; Yao, C.; Wu, F.; Zhang, H.; Shen, X. Comparison of the Effects of 10.6-Μm Infrared Laser and Traditional Moxibustion in the Treatment of Knee Osteoarthritis. Lasers Med. Sci. 2020, 35, 823–832.
- De Souza Guimarães, L.; Costa, L.d.C.M.; Araujo, A.C.; Nascimento, D.P.; Medeiros, F.C.; Avanzi, M.A.; Leal-Junior, E.C.P.; Costa, L.O.P.; Tomazoni, S.S. Photobiomodulation Therapy Is Not Better than Placebo in Patients with Chronic Nonspecific Low Back Pain: A Randomised Placebo-Controlled Trial: A Randomised Placebo-Controlled Trial. Pain 2021, 162, 1612–1620.
- Nunes, R.F.H.; Cidral-Filho, F.J.; Flores, L.J.F.; Nakamura, F.Y.; Rodriguez, H.F.M.; Bobinski, F.; De Sousa, A.; Petronilho, F.; Danielski, L.G.; Martins, M.M.; et al. Effects of Far-Infrared Emitting Ceramic Materials on Recovery during 2-Week Preseason of Elite Futsal Players. J. Strength Cond. Res. 2020, 34, 235–248.
- Bontemps, B.; Gruet, M.; Vercruyssen, F.; Louis, J. Utilisation of Far Infrared-Emitting Garments for Optimising Performance and Recovery in Sport: Real Potential or New Fad? A Systematic Review. PLoS ONE 2021, 16, e0251282.
- Foley, J.; Vasily, D.B.; Bradle, J.; Rudio, C.; Calderhead, R.G. 830 Nm Light-Emitting Diode (Led) Phototherapy Significantly Reduced Return-to-Play in Injured University Athletes: A Pilot Study. Laser Ther. 2016, 25, 35–42.
- Tsai, S.-R.; Hamblin, M.R. Biological Effects and Medical Applications of Infrared Radiation. J. Photochem. Photobiol. B 2017, 170, 197–207.
- Wickenheisser, V.A.; Zywot, E.M.; Rabjohns, E.M.; Lee, H.H.; Lawrence, D.S.; Tarrant, T.K. Laser Light Therapy in Inflammatory, Musculoskeletal, and Autoimmune Disease. Curr. Allergy Asthma Rep. 2019, 19, 37.
- Barros, N.D.M.; Sbroglio, L.L.; Buffara, M.D.O.; Baka, J.L.C.E.S.; Pessoa, A.D.S.; Azulay-Abulafia, L. Phototherapy. An. Bras. Dermatol. 2021, 96, 397–407.
- Wang, Y.; Shui, S.; Wang, X. Molecular Mechanism of Far-infrared Therapy and Its Applications in Biomedicine. Sci. Technol. Rev. 2014, 32, 80–84.
