Retention of foreign bodies (FB) in the liver parenchyma is a rare event in children but it can bring a heavy burden in terms of immediate and long-term complications. Multiple materials can migrate inside the liver. Clinical manifestations may vary, depending on the nature of the foreign body, its route of penetration and timing after the initial event. Moreover, the location of the FB inside the liver parenchyma may pose specific issues related to the possible complications of a challenging surgical extraction. Different clinical settings and the need for highly specialized surgical skills may influence the overall management of these children.
- liver
- foreign body
- children
- penetrating
- trauma
1. Introduction
2. Foreign Bodies in the Liver in Children
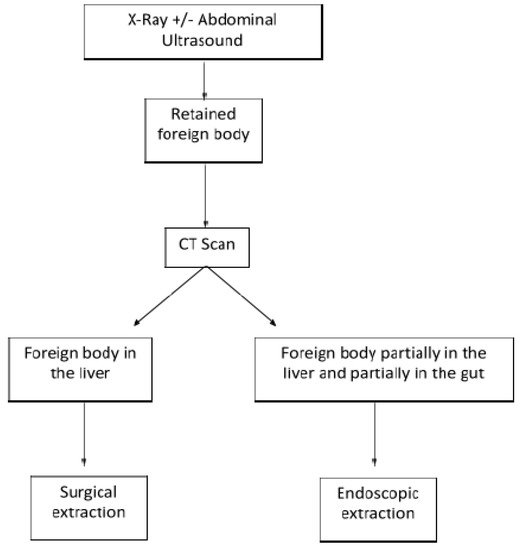
As reported in multiple adult and pediatric series and case reports, retained hepatic FBs are distinguished in three categories, based on the route used to reach the liver: penetrating, ingested, and bloodstream [2][12].
3. Conclusions
This entry is adapted from the peer-reviewed paper 10.3390/children9020120
References
- Crankson, S.J. Hepatic Foreign Body in a Child. Pediatr. Surg. Int. 1997, 12, 426–427.
- Dominguez, S.; Wildhaber, B.E.; Spadola, L.; Mehrak, A.D.; Chardot, C. Laparoscopic Extraction of an Intrahepatic Foreign Body after Transduodenal Migration in a Child. J. Pediatr. Surg. 2009, 44, e17–e20.
- Xu, J.; Wang, H.; Song, Z.-W.; Shen, M.-D.; Shi, S.-H.; Zhang, W.; Zhang, M.; Zheng, S.-S. Foreign Body Retained in Liver Long after Gauze Packing. World J. Gastroenterol. 2013, 19, 3364–3368.
- Thipphavong, S.; Kellenberger, C.J.; Rutka, J.T.; Manson, D.E. Hepatic and Colonic Perforation by an Abandoned Ventriculoperitoneal Shunt. Pediatr. Radiol. 2004, 34, 750–752.
- Adams, S.D.; Baker, D.; Takhar, A.; Beattie, R.M.; Stanton, M.P. Complication of Percutaneous Endoscopic Gastrostomy. Arch. Dis. Child. 2014, 99, 788.
- Glick, W.A.; Simo, K.A.; Swan, R.Z.; Sindram, D.; Iannitti, D.A.; Martinie, J.B. Pyogenic Hepatic Abscess Secondary to Endolumenal Perforation of an Ingested Foreign Body. J. Gastrointest. Surg. 2012, 16, 885–887.
- Geramizadeh, B.; Jahangiri, R.; Moradi, E. Causes of Hepatic Granuloma: A 12-Year Single Center Experience from Southern Iran. Arch. Iran. Med. 2011, 14, 4.
- Santos, S.A. Hepatic Abscess Induced by Foreign Body: Case Report and Literature Review. World J. Gastroenterol. 2007, 13, 1466–1470.
- Giestas, S.; Mendes, S.; Gomes, D.; Sofia, C. Obstructive Jaundice Due to Foreign Body in the Bile Duct: An Unusual Finding. GE Port. J. Gastroenterol. 2016, 23, 228–230.
- Greene, B.; Jones, D.; Sarrazin, J.; Coburn, N.G. Porta Hepatis Abscess and Portal Vein Thrombosis Following Ingestion of a Fishbone. BMJ Case Rep. 2019, 12, e227271.
- Eguchi, S.; Matsuo, S.; Hidaka, M.; Azuma, T.; Yamaguchi, S.; Kanematsu, T. Impaction of a Shrapnel Splinter in the Common Bile Duct After Migrating from the Right Thoracic Cavity: Report of a Case. Surg. Today 2002, 32, 383–385.
- Azili, M.N.; Karaman, A.; Karaman, I.; Erdoǧan, D.; Çavuşoǧlu, Y.H.; Aslan, M.K.; Çakmak, Ö. A Sewing Needle Migrating into the Liver in a Child: Case Report and Review of the Literature. Pediatr. Surg. Int. 2007, 23, 1135–1137.
- Fragulidis, G.P.; Chondrogiannis, K.D.; Karakatsanis, A.; Lykoudis, P.M.; Melemeni, A.; Polydorou, A.; Voros, D. Cystoid Gossypiboma of the Liver 15 Years after Cholecystectomy. Am. Surg. 2011, 77, 17–18.
- Haq, A.; Morris, J.; Goddard, C.; Mahmud, S.; Nassar, A.H.M. Delayed Cholangitis Resulting from a Retained T-Tube Fragment Encased within a Stone. Surg. Endosc. 2002, 16, 714.
- Matsumoto, H.; Ikeda, E.; Mitsunaga, S.; Naitoh, M.; Nawa, S.; Furutani, S. Choledochal Stenosis and Lithiasis Caused by Penetration and Migration of Surgical Metal Clips. J. Hepato-Biliary-Pancreat. Surg. 2000, 7, 603–605.
- Tsumura, H.; Ichikawa, T.; Kagawa, T.; Nishihara, M.; Yoshikawa, K.; Yamamoto, G. Failure of Endoscopic Removal of Common Bile Duct Stones Due to Endo-Clip Migration Following Laparoscopic Cholecystectomy. J. Hepato-Biliary-Pancreat. Surg. 2002, 9, 274–277.
- Cimsit, B.; Keskin, M.; Ozden, I.; Alper, A. Obstructive Jaundice Due to a Textiloma Mimicking a Common Bile Duct Stone. J. Hepato-Biliary-Pancreat. Surg. 2006, 13, 172–173.
- Singhal, V.; Lubhana, P.; Durkhere, R.; Bhandari, S. Liver Abscess Secondary to a Broken Needle Migration—A Case Report. BMC Surg. 2003, 3, 8.
- Abel, R.M.; Fischer, J.E.; Hendren, W.H. Penetration of the Alimentary Tract by a Foreign Body with Migration to the Liver Report of a Case. Arch. Surg. 1971, 102, 227–228.
- Senol, A.; Işler, M.; Minkar, T.; Oyar, O. A Sewing Needle in the Liver: 6 Years Later. Am. J. Med. Sci. 2010, 339, 390–391.
- Nishimoto, Y.; Suita, S.; Taguchi, T.; Noguchi, S.I.; Ieiri, S. Hepatic Foreign Body-A Sewing Needle-In a Child. Asian J. Surg. 2003, 26, 231–233.
- Bakal, U.; Tartar, T.; Kazez, A. A Rare Mode of Entry for Needles Observed in the Abdomen of Children: Penetration. J. Indian Assoc. Pediatr. Surg. 2012, 17, 130–131.
- Marya, K.M.; Yadav, V.; Rattan, K.N.; Kundu, Z.S.; Sangwan, S.S. Unusual K-Wire Migration. Indian J. Pediatr. 2006, 73, 1107–1108.
- le Mandat-Schultz, A.; Arnaud, B.; Nadia, B.; Aigrain, Y.; de Lagausie, P. Intrahepatic Foreign Body Laparoscopic Extraction. Surg. Endosc. 2003, 17, 1849.
- Chen, J.; Wang, C.; Zhuo, J.; Wen, X.; Ling, Q.; Liu, Z.; Guo, H.; Xu, X.; Zheng, S. Laparoscopic Management of Enterohepatic Migrated Fish Bone Mimicking Liver Neoplasm. Medicine 2019, 98, e14705.
- Akçam, M.; Koçkar, C.; Tola, H.T.; Duman, L.; Gündüz, M. Endoscopic Removal of an Ingested Pin Migrated into the Liver and Affixed by Its Head to the Duodenum. Gastrointest. Endosc. 2009, 69, 382–384.
- Hyak, J.M.; Todd, H.; Rubalcava, D.; Vogel, A.M.; Fallon, S.; Naik-Mathuria, B. Barely Benign: The Dangers of BB and Other Nonpowder Guns. J. Pediatr. Surg. 2020, 55, 1604–1609.
- Meeks, T.; Nwomeh, B.; Abdessalam, S.; Groner, J. Paradoxical Missile Embolus to the Right Superficial Femoral Artery Following Gunshot Wound to the Liver: A Case Report. J. Trauma-Inj. Infect. Crit. Care 2004, 57, 1338–1339.
- Veenstra, M.; Prasad, J.; Schaewe, H.; Donoghue, L.; Langenburg, S. Nonpowder Firearms Cause Significant Pediatric Injuries. J. Trauma Acute Care Surg. 2015, 78, 1138–1142.
- Güsgen, C.; Willms, A.; Richardsen, I.; Bieler, D.; Kollig, E.; Schwab, R. Besonderheiten Und Versorgung Penetrierender Verletzungen Am Beispiel von Schuss—Und Explosionsopfern Ohne Ballistischen Körperschutz in Afghanistan (2009–2013). Zent. Chir. -Z. Allg. Visz. Gefasschir. 2017, 142, 386–394.
- Feliciano, D.V.; Burch, J.M.; Spjut-Patrinely, V.; Mattox, K.L.; Jordan, G.L. Abdominal Gunshot Wounds. Ann. Surg. 1988, 208, 362–370.
- Schellenberg, M.; Benjamin, E.; Piccinini, A.; Inaba, K.; Demetriades, D. Gunshot Wounds to the Liver: No Longer a Mandatory Operation. J. Trauma Acute Care Surg. 2019, 87, 350–355.
- Navsaria, P.H.; Nicol, A.J.; Krige, J.E.; Edu, S. Selective Nonoperative Management of Liver Gunshot Injuries. Ann. Surg. 2009, 249, 653–656.
- Coccolini, F.; Panel, T.W.E.; Coimbra, R.; Ordonez, C.; Kluger, Y.; Vega, F.; Moore, E.E.; Biffl, W.; Peitzman, A.; Horer, T.; et al. Liver Trauma: WSES 2020 Guidelines. World J. Emerg. Surg. 2020, 15, 24.
- Avcu, S.; Ünal, Ö.; Özen, Ö.; Bora, A.; Dülger, A.C. A Swallowed Sewing Needle Migrating to the Liver. N. Am. J. Med. Sci. 2009, 1, 193–195.
- Xu, B.-J.; Lü, C.-J.; Liu, W.-G.; Shu, Q.; Zhang, Y.-B. A Sewing Needle Within the Right Hepatic Lobe of an Infant. Pediatr. Emerg. Care 2013, 29, 1013–1015.
- Demir, S.; Ilıkan, G.B.; Ertürk, A.; Şahin, V.S.; Öztorun, C.İ.; Güney, D.; Erten, E.E.; Azılı, M.N.; Şenel, E. Removal of Two Needles from the Liver and Axillary Region Using Ultrasound: A Case Report with Current Literature Review. Med. Bull. Haseki 2020, 58, 390–394.
- Saitua, F.; Acosta, S.; Soto, G.; Herrera, P.; Tapia, D. To Remove or Not RemoveIAsymptomatic Sewing Needle Within Hepatic Right Lobe in an Infant. Pediatr. Emerg. Care 2009, 25, 463–464.
- Chan, S.C.; Chen, H.Y.; Ng, S.H.; Lee, C.M.; Tsai, C.H. Hepatic Abscess Due to Gastric Perforation by Ingested Fish Bone Demonstrated by Computed Tomography. J. Formos. Med. Assoc. 1999, 98, 145–147.
- Carver, D.; Bruckschwaiger, V.; Martel, G.; Bertens, K.A.; Abou-Khalil, J.; Balaa, F. Laparoscopic Retrieval of a Sewing Needle from the Liver: A Case Report. Int. J. Surg. Case Rep. 2018, 51, 376–378.
- Poyanli, A.; Bilge, O.; Kapran, Y.; Güven, K. Foreign Body Granuloma Mimicking Liver Metastasis. Br. J. Radiol. 2005, 78, 752–754.
- Ariyuca, S.; Doǧan, M.; Kaya, A.; Ay, M. An Unusual Cause of Liver Abscess. Liver Int. 2009, 29, 1552.
