Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
The ocular prostheses, used for the prosthetic rehabilitation of ocular defects, are generally made from acrylic resin. As the thickness of clear acrylic over the iris is increased on the ocular prosthesis, the size of the iris is also increased, due to magnification through the clear resin.
- ocular prosthesis
- eye prosthesis
- iris
- magnification
- clear acrylic
- acrylic resin
- polymethyl methacrylate
1. Introduction
Anophthalmic sockets or loss of an eyeball can be caused by various reasons, mainly due to trauma (46%) and malignant tumor (44%), followed by nonspecific (8%) and congenital (2%) [1][2]. Among malignant tumors, retinoblastoma and malignant melanoma were the most common pathological diagnoses [3][4]. The prosthetic rehabilitation of an ophthalmic socket is important, as an eye defect undeniably impacts patient self-esteem and causes esthetic and psychological problems [5][6]. An ocular prosthesis, or fake eye (Figure 1), generally fabricated from polymethyl methacrylate (PMMA) or acrylic resin, replaces the missing organ and provides esthetics and psychological comfort to the patient. The ocular prosthesis of appropriate contour, size, and color bars patients from being handicapped and allows them to pursue their normal lives [7][8].

Figure 1. Ocular prosthesis.
The ocular prosthesis can be prefabricated or custom-made [9]. The latter provides a better fit to the eye socket, better cosmetic results, and more comfort to the patients. The custom-made prosthesis can be fabricated by conventional techniques or assisted with digital technologies [10][11]. In the conventional technique, following the impression of the ocular defect, the base shell is fabricated following curing, and staining is done manually to match the patient’s natural eye [11]. In digitally-assisted techniques, the base shell can be 3D printed, and staining can be assisted and printed with digital photography [12][13]. Following staining, in both fabrication techniques, the addition and curing of a thin superficial layer of acrylic resin are required to resemble the human cornea [9][10].
The common problems of fitting the ocular prosthesis are in the proper shape or size of the prosthesis, as well as the difficulty in matching color, eyelid aperture, and iris size to the normal eye. Rasmussen [14] found that the most frequent complications associated with ocular prostheses are secretion, lagophthalmos, enophthalmos, rotating prosthesis, prosthesis falling out, and exophthalmos. Anophthalmic patients are likely to experience problems with their prosthetic eye, and a survey on patients’ concerns and satisfaction with custom ocular prostheses found that the most common prosthesis-related concerns were reduction of eye motility, eye discharge, and difference in the size of the prosthetic eye, relative to the other eye [15].
The larger-than-expected iris size is usually caused by the magnification of the iris during the fabrication of a new ocular prosthesis and relining of the old ocular prosthesis which results in an unesthetic prosthesis (Figure 2). The clear acrylic over the iris acts as a lens and causes the magnification of the iris. However, the research on the magnification of the clear acrylic resin is still lacking. Hence, this research investigated the magnification of the iris in the ocular prosthesis with various thicknesses of clear heat cure acrylic resin. Ocular prostheses were equally divided into six groups with various thicknesses of clear heat cure acrylic resin (polymethyl methacrylate, PMMA) over the iris; no acrylic resin over the iris (control); and 2, 4, 6, 8, and 10 mm thickness of clear acrylic resin over the iris. The sizes of the iris among groups were compared. It was found that the magnification of the iris increases significantly as the thickness of clear heat cure acrylic resin over the iris is increased on the ocular prosthesis.
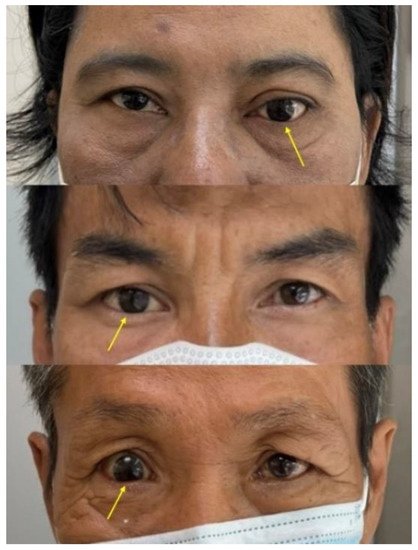
Figure 2. The iris size of the ocular prosthesis not matching the normal eye, due to the magnification of the iris from the clear acrylic resin.
2. Current Insights
Although an ocular prosthesis can be fabricated from acrylic resin and ceramic, acrylic resin is the material of choice for the fabrication of ocular prostheses, due to easy handling, adaptation, good esthetics, ability to reline, and low cost [16][17]. Acrylic resin can simulate the natural color of the sclera, while the colorless resin is used to cover the characterization of blood vessels and artificial iris [17][18][19]. In addition, the acrylic resin has good physical and mechanical properties for the longevity of the ocular prosthesis [18][20][21][22]. The disadvantage of acrylic resin prosthesis is the material discoloration over time may be caused by intrinsic or extrinsic factors [23][24]. Hence, the patients need to change the prosthesis in about 5–7 years. The chemical and mechanical polishing of acrylic resin is done to reduce the ocular prosthesis surface roughness and accumulation of impurities and microorganisms [24].
In this research, it was found that, as the thickness of clear heat cure acrylic resin over the iris is increased on the ocular prosthesis, the magnification of the iris is also increased (Table 1). In addition, Equations (2) and (3) give the information on the final observed diameter of the iris by adding the amount of clear acrylic resin and magnification that occurred by adding the amount of clear acrylic resin, respectively. From this research, the researchers found how much magnification can occur by adding 2, 4, 6, 8, and 10 mm of clear acrylic resin over the iris. Hence, these results can be used in the fabrication and relining of the ocular prostheses. This information and guideline on the magnification of the iris with the thickness of clear acrylic resin, provided in this research, will reduce the error in choosing the size of the iris.
Table 1. Descriptive statistics of the magnification of the iris in various groups.
| Study Groups (n = 60) | Magnification (Mean ± SD) | 95% CI | Minimum | Maximum | |
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| No acrylic above | - | - | - | - | - |
| 2 mm clear acrylic | 1.06 ± 0.00 | 1.061 | 1.069 | 1.06 | 1.08 |
| 4 mm clear acrylic | 1.01 ± 0.01 | 1.094 | 1.104 | 1.09 | 1.11 |
| 6 mm clear acrylic | 1.16 ± 0.01 | 1.153 | 1.169 | 1.15 | 1.19 |
| 8 mm clear acrylic | 1.24 ± 0.01 | 1.236 | 1.250 | 1.23 | 1.26 |
| 10 mm clear acrylic | 1.31 ± 0.01 | 1.304 | 1.316 | 1.30 | 1.32 |
SD = standard deviation, CI = confidence interval for mean.
Magnification of the iris is due to the refraction of light, with the clear acrylic resin acting as a convex lens. Magnification depends on both refractive index differences between the medium and curvature of the lens (Figure 3). The refractive index, or index of refraction (n), of clear acrylic is 1.48, which changes the direction of light by a change in speed. In the case of the ocular prosthesis, when the light from the actual iris passes the acrylic resin into the air, it bends and causes the visual perception of a larger iris.
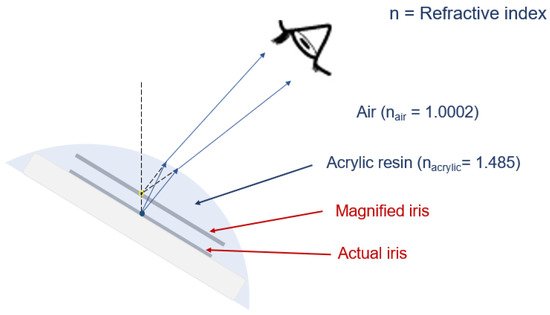
Figure 3. Magnification of the iris, due to the refraction of light, with the clear acrylic resin acting as a lens, due to the refraction of light.
Furthermore, this research provides the information of the final observed diameter of the iris and the magnification of the iris obtained through numerical calculations. Various factors that can affect the magnification of the iris in the ocular prosthesis are the thickness of clear acrylic resin, curvature of clear acrylic resin/shape of the ocular prosthesis, diameter of the iris, and refractive index differences between the clear acrylic resin and air (refractive index of PMMA/acrylic resin is 1.47 [25], with 1.0 for air) [26]. In the human eye, the refractive index of the cornea and overlying tear film are key factors affecting refraction and overall optical properties of the eye, and the normal refractive index of the human cornea is 1.376 (range from 1.335 to 1.4391) [27]. Similarly, the refractive index of PMMA is 1.47 [25]. Hence, the refraction of light in clear acrylic resin is comparable to the human cornea. If the ocular prosthesis is made from ceramic materials, the magnification results might have been slightly altered, due to the difference in the refractive index (refractive index of glass-ceramic is 1.55) [26].
In this research, the magnification was studied by taking the same diameter of the iris (10.25 mm) and same curvature of clear acrylic resin/ shape of the ocular prosthesis in all study groups, as well as the maximum 10 mm thickness of acrylic. Hence, future studies can be done by taking different sizes of iris and thicker acrylic resin in more samples, using different optical and geometrical parameters to study the magnification. In addition, it can be useful to do more specific characterization methods, and different optical and geometric parameters will be suitable for future investigation and characterizations. Additional methods are needed to study the swelling degree and thermo-sensitivity analysis of the acrylic resin.
This entry is adapted from the peer-reviewed paper 10.3390/jfb13010029
References
- Raj, N.; Singh, M.; Raj, V.; Anwar, M.; Kumar, L. Prevalence of ocular defects among patients visiting in an institutionalized hospital setting: A cross-sectional study. Natl. J. Maxillofac. Surg. 2016, 7, 67–70.
- Hatamleh, M.M.; Abbariki, M.; Alqudah, N.; Cook, A.E. Survey of ocular prosthetics rehabilitation in the united kingdom, part 1: Anophthalmic patients’ aetiology, opinions, and attitudes. J. Craniofac. Surg. 2017, 28, 1293–1296.
- Kord Valeshabad, A.; Naseripour, M.; Asghari, R.; Parhizgar, S.H.; Parhizgar, S.E.; Taghvaei, M.; Miri, S. Enucleation and evisceration: Indications, complications and clinicopathological correlations. Int. J. Ophthalmol. 2014, 7, 677–680.
- Yousuf, S.J.; Jones, L.S.; Kidwell, E.D., Jr. Enucleation and evisceration: 20 years of experience. Orbit 2012, 31, 211–215.
- Sabel, B.A.; Wang, J.; Cárdenas-Morales, L.; Faiq, M.; Heim, C. Mental stress as consequence and cause of vision loss: The dawn of psychosomatic ophthalmology for preventive and personalized medicine. EPMA J. 2018, 9, 133–160.
- Goiato, M.C.; Nicolau, E.I.; Mazaro, J.V.; Dos Santos, D.M.; Vedovatto, E.; Zavanelli, A.C.; Filho, H.G.; Pellizzer, E.P. Mobility, aesthetic, implants, and satisfaction of the ocular prostheses wearers. J. Craniofac. Surg. 2010, 21, 160–164.
- Amornvit, P.; Rokaya, D.; Shrestha, B.; Srithavaj, T. Prosthetic rehabilitation of an ocular defect with post-enucleation socket syndrome: A case report. Saudi Dent. J. 2014, 26, 29–32.
- Patil, S.B.; Meshramkar, R.; Naveen, B.H.; Patil, N.P. Ocular prosthesis: A brief review and fabrication of an ocular prosthesis for a geriatric patient. Gerodontology 2008, 25, 57–62.
- Cevik, P.; Dilber, E.; Eraslan, O. Different techniques in fabrication of ocular prosthesis. J. Craniofac. Surg. 2012, 23, 1779–1781.
- Sethi, T.; Kheur, M.; Haylock, C.; Harianawala, H. Fabrication of a custom ocular prosthesis. Middle East Afr. J. Ophthalmol. 2014, 21, 271–274.
- Ko, J.; Kim, S.H.; Baek, S.W.; Chae, M.K.; Yoon, J.S. Semi-automated fabrication of customized ocular prosthesis with three-dimensional printing and sublimation transfer printing technology. Sci. Rep. 2019, 9, 2968.
- Lanzara, R.; Thakur, A.; Viswambaran, M.; Khattak, A. Fabrication of ocular prosthesis with a digital customization technique-a case report. J. Family Med. Prim. Care. 2019, 8, 1239–1242.
- Artopoulou, I.I.; Montgomery, P.C.; Wesley, P.J.; Lemon, J.C. Digital imaging in the fabrication of ocular prostheses. J. Prosthet. Dent. 2006, 95, 327–330.
- Rasmussen, M.L. Complications from eye prosthesis. Ugeskr. Laeger 2008, 170, 2456–2458.
- Dave, T.V.; Nayak, A.; Palo, M.; Goud, Y.; Tripuraneni, D.; Gupta, S. Custom ocular prosthesis-related concerns: Patient feedback survey-based report vis-à-vis objective clinical grading scales. Orbit 2021, 40, 357–363.
- Fernandes, A.U.; Goiato, M.C.; dos Santos, D.M. Effect of weathering and thickness on the superficial microhardness of acrylic resin and ocular button. Contact Lens Anterior Eye 2009, 32, 283–287.
- Fernandes, A.U.; Goiato, M.C.; Dos Santos, D.M. Effect of weathering and thickness on roughness of acrylic resin and ocular button. Contact Lens Anterior Eye 2010, 33, 124–147.
- Moreno, A.; Goiato, M.C.; dos Santos, D.M.; Haddad, M.F.; Pesqueira, A.A.; Bannwart, L.C. Effect of different disinfectants on the microhardness and roughness of acrylic resins for ocular prosthesis. Gerodontology 2013, 30, 32–39.
- Bannwart, L.C.; Goiato, M.C.; dos Santos, D.M.; Moreno, A.; Pesqueira, A.A.; Haddad, M.F.; Andreotti, A.M.; de Medeiros, R.A. Chromatic changes to artificial irises produced using different techniques. J. Biomed. Opt. 2013, 18, 58002.
- Zafar, M.S. Prosthodontic applications of polymethyl methacrylate (pmma): An update. Polymers 2020, 12, 2299.
- Fernandes, A.U.; Portugal, A.; Veloso, L.R.; Goiato, M.C.; Santos, D.M. Assessment of the flexural strength of two heat-curing acrylic resins for artificial eyes. Braz. Oral Res. 2009, 23, 263–267.
- Schulze, K.A.; Marshall, S.J.; Gansky, S.A.; Marshall, G.W. Color stability and hardness in dental composites after accelerated aging. Dent. Mater. 2003, 19, 612–619.
- Shen, C.; Rawls, H.R.; Esquivel-Upshaw, J. Phillips’ Science of Dental Materials, 13th ed.; Saunders: Saint Louis, MO, USA, 2021.
- Santos, D.M.; Nagay, B.E.; da Silva, E.V.; Bonatto Lda, R.; Sonego, M.V.; Moreno, A.; Rangel, E.C.; da Cruz, N.C.; Goiato, M.C. In vitro analysis of different properties of acrylic resins for ocular prosthesis submitted to accelerated aging with or without photopolymerized glaze. Mater. Sci. Eng. C Mater. Biol. Appl. 2016, 69, 995–1003.
- Othayoth, A.K.; Srinivas, B.; Murugan, K.; Muralidharan, K. Poly(methyl methacrylate)/polyphosphate blends with tunable refractive indices for optical applications. Opt. Mater. 2020, 104, 109841.
- Heffernan, M.J.; Aquilino, S.A.; Diaz-Arnold, A.M.; Haselton, D.R.; Stanford, C.M.; Vargas, M.A. Relative translucency of six all-ceramic systems. Part ii: Core and veneer materials. J. Prosthet. Dent. 2002, 88, 10–15.
- Patel, S.; Tutchenko, L. The refractive index of the human cornea: A review. Contact Lens Anterior Eye 2019, 42, 575–580.
This entry is offline, you can click here to edit this entry!
