Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Virology
The influenza virus is a worldwide disease that affects up to 5–15% of the global population. The mortality from influenza-associated respiratory disease is estimated to be more than half a million each year, and that number significantly increases when a new strain emerges to cause a pandemic. The influenza virus has a high mutation rate, which is the basis for the evolutionary variability of the influenza virus. One cycle of virus replication may lead to a new strain with significant changes in its viral biocharacteristics and pathogenicity.
- A(H1N1)pdm09 influenza viruses
- evolution
- viral toxicity
- viral pathogenicity
- thermal stability of the hemagglutinin
- temperature sensitivity of reproduction
- polymerase complex
1. Introduction
The first known influenza pandemic was the Spanish flu (1918–1920, death toll ~17.4 million) [2], the second was the Asian flu (1957–1958, death toll 1–4 million), the third was the Hong Kong flu (1968–1969, death toll 1–4 million), [3] and after that came the Russian flu (1977–1979, over 700,000 deaths) [4]. The last pandemic was influenza A(H1N1) in 2009–2010, which is estimated to have caused about 400,000 deaths in 2009 alone [5]. To date, it is impossible to know when influenza pandemics are going to arise, which makes evolutionary studies of the influenza virus highly important. Influenza is an RNA virus that is part of the Orthomyxoviruses family, which is divided into four subfamilies: A, B, C, and D. Influenza A is also divided into several subtypes depending on the combination of the hemagglutinin protein (HA), which has 18 subtypes, and the neuraminidase protein (NA), which has 11 subtypes [6]. This study will focus on the evolution of the H1N1pdm09 pandemic of the virus.There are three essential properties that an influenza virus strain must have to cause a pandemic: firstly, the strain must not be previously recognized by human immunity; secondly, the strain should have high pathogenicity for the human, and finally, the virus strain should be transmissible and able to cause infection on person-to-person interaction [7]. In 2009, a new A(H1N1)pdm09 influenza virus strain appeared that had all of the three previously mentioned properties. The new pandemic influenza virus had numerous biological features typical of pandemic viruses; in particular, it had pronounced non-ts and non-ca phenotypes and resistance to sera non-specific inhibitors [8].
A comparative analysis of essential biological properties of evolving H1 viruses has not yet been carried out. Of these characteristics, the HA thermal stability, toxicity, and non-ts phenotype warrant the most attention. A Non-ts phenotype is the virus’ ability to reproduce at elevated temperatures of the low respiratory tract [10,11,12,13]. For human influenza A viruses, this ability might be inherited from their ancestor that replicated in animal hosts (birds or pigs) that have higher physiological body temperatures (40–42 °C) [14]. Some of the influenza viruses are characterized as lethal in animal models two to four days after inoculation with a high dose of the viral particles [15,16,17]; this characteristic is referred to as viral toxicity. HA stability is the ability of the hemagglutinin protein to resist denaturation and maintain its function in stress conditions such as elevated temperature [18]. The evolution of and changes in these characteristics result from mutations acquired in the viral genome.
The influenza A virus contains eight negative-sense, single-stranded viral RNA gene segments, which encode the 10 essential viral proteins (HA, NA, M2, M1, NP, NS1, NS2, PB1, PB2, and PA). A mutation in any of these proteins might change the viral characteristic and thus affect its pathogenicity. The heterotrimeric polymerase complex, consisting of three subunits—PB1 (polymerase basic protein 1), PB2 (polymerase basic protein 2), and PA (polymerase acidic protein)—has gained the most interest [19]. Each of these subunits contributes to polymerase function: the PA snitches the Cap of cellular mRNA through its endonuclease domain [20], while the PB2’s functions are mRNA recognition and binding of “cap” structures and the PB1 participates in transcriptase primer elongation and endonuclease activity [21]. In addition, the polymerase complex has a significant effect on the manifestation of the ts/non-ts phenotype. Several studies showed that mutations in the complex can dramatically affect and change the properties of the virus [22,23,24,25].
2. Current Inisghts
The researchers analyzed 21 A(H1N1)pdm09 viruses—starting from A/California/07/2009 and ending with last year’s strains—according to a variety of parameters, in particular, the pathogenicity and toxicity for mice, the temperature sensitivity of their reproduction in developing chicken embryos, and the thermal stability of hemagglutinin. We sought to detect any relationship between these traits and possible mutational changes.
Non-ts phenotype viruses can infect lower respiratory tracts as they can replicate at temperatures higher than 37 °C, which increases their pathogenicity and allows them to resist the organism’s response [35,36]. For this reason, temperature-sensitive (ts) viruses are much less virulent [35]. Temperature sensitivity is also an essential property required for the development of attenuated reassortant strains for live influenza vaccines [37,38]. It has been suggested that the circulation of only temperature-sensitive viruses for several years can be considered as a sign of the coming appearance of a new virus that is antigenically distant from the circulating strains [39].
This suggestion is supported by the observation that the evolutionary variability of the ts/non-ts phenotype has a fluctuating trend where the non-ts phenotype is dominant at the beginning of the pandemic cycle. Subsequently, the percentage of ts viruses after the emergence of a new strain increases stably over the years [14,39]. For instance, in 1949–1957, ts isolates accounted for 8.3% of all investigated A(H1N1) viruses, whereas they made up 76.5% in 1977–1978 [35], which provided the opportunity for new non-ts strains (A/Khabarovsk/90/77 “Russian flu”) to appear and circulate, causing the 1977 pandemic [14].
The same phenomenon was observed just before the 2009 influenza pandemic. All influenza A (H1N1), influenza A (H3N2), and influenza B viruses isolated from 2006 to 2009 had a ts phenotype [14]. In other words, the ts viruses circulated until 2009, when they were replaced by the viciously spreading non-ts A/California/07/09 (H1N1)pdm influenza virus, causing the 2009 pandemic. The A/California/07/09 (H1N1)pdm virus has begun another wave of circulation of non-ts viruses.
Although there were only 21 viruses in our study group, the fluctuating trend persevered, whereby drift variants of the A/California/07/09 (H1N1)pdm virus kept the non-ts phenotype until 2015, after which the first ts strain (9, A/Slovenia/2903/2015) appeared and the proportion of the ts phenotype started to increase gradually, indicating that the ts phenotype will dominate in the coming years.
The newly emerged human influenza A viruses might have kept two of the three genes, as a minimum, of the polymerase complex from their progenitor, which could explain the ability of these viruses to withstand and produce new copies in temperatures over 37 °C since these progenitors used to replicate in animals that have a higher physiological body temperature than humans, such as birds or pigs [14]. In addition, a variety of studies showed that the ts/non-ts phenotype of influenza viruses is connected with mutations in the protein PB2 [40,41,42].
The phenomenon of influenza viral toxicity has been known since the 1940s [16,43]. However, the mechanism of viral toxicity is still poorly studied. Most works were published in the 1990s [44,45,46]. The idea was that the toxicity of the influenza virus is probably caused by viral dsRNA, produced during viral replication, either directly because it shares many biological and physical properties of bacterial toxins or as a result of the interferon (IFN) it induces [46,47]. The direct mechanism theory is supported by the antitoxic effect of rimantadine, which works as an M2 ion channel membrane protein blocker, preventing detachment of the viral RNP from the matrix, which blocks influenza A virus entry into the cells [37,38]. However, rimantadine did not show specific activity against influenza B viruses’ primary pneumonia [48]. Furthermore, though rimantadine created a significant reduction in the mortality of mice from toxic effects caused by influenza A viruses, influenza B viruses, or exotoxin of Staphylococcus aureus, it did not prevent the toxic effect of adrenaline [48]. This suggests that bacterial toxins and influenza viruses might have the same toxic mechanism that can be eliminated by rimantadine even if the strain is resistant to it [48]. Moreover, viral dsRNA causes cytotoxic effects through two mechanisms: either it inhibits protein synthesis indirectly through its induction of 2’–5’ oligo (A) synthetase and/or a dsRNA-dependent protein kinase, or it enhances degradation of ssRNA through activation of the endonuclease RNase. These cellular effects may cause local tissue necrosis in addition to the classical antiviral effect of IFN. During cell lysis, dsRNA, which can resist degradation by intracellular nucleases [47], is released into the extracellular environment and interacts with macrophages, invoking cytokine production [46,47] and triggering the toxic effect [44,45]. These toxicity mechanisms might explain why there is no one mutation or amino acid substitution that can be associated with the different levels of toxicity of the studied viruses.
The research concluded that for a virus to have properties such as toxicity, or the thermal stability of the hemagglutinin, it is necessary but not sufficient to be characterized as a non-ts phenotype. In other words, if the virus has a toxic effect or thermally stable hemagglutinin, it is adequate evidence that the virus has a non-ts phenotype but it is not the other way around. Furthermore, having a non-ts phenotype, toxicity and thermally stable hemagglutinin are necessary but not sufficient for the virus to become pathogenic for laboratory animals, indicating that there are still some properties that might also contribute to the degree of pathogenicity. The strongest candidates are the virus transmissibility and resistance to sera non-specific inhibitors. However, if the virus is pathogenic for laboratory animals, that means that it has all of the other three properties (Figure 8).
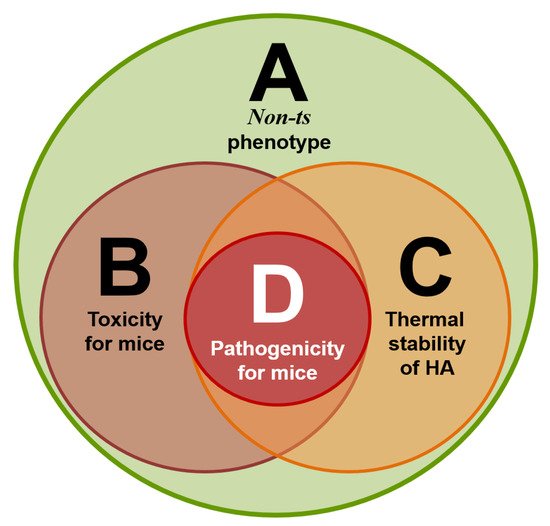
Figure 8. Four circle diagram: correlations of four sets of virus properties—A (non-ts phenotype), B (toxicity for mice), C (thermal stability of the hemagglutinin), and D (pathogenicity for mice).
Earlier, we showed that the A/South Africa/3626/2013 influenza virus has the unique property of high pathogenicity for mice without preliminary adaptation to them, but the ancestor virus A/California/07/2009 does not have such a property [29]. The interaction between the influenza virus and the host cells on the molecular level defined the viral virulence and its ability to infect this particular host. In addition, the virus has different methods of avoiding the antiviral response of the host. The process of the adaptation of the influenza virus to a new host requires mutations and/or the reassortment of the viral genome, and these events present themselves as a level of pathogenicity [49].
Practically all of the viral genes participate in virus pathogenicity; this fact was established in numerous studies [50,51,52,53,54,55,56,57,58,59,60,61]. HA and NA always work in harmony, are responsible for tissue tropism and interspecies transmission [49], and strongly affect transmissibility between humans [62], while NS1 virus proteins increase the viral pathogenicity by working as interferon antagonists and inhibiting the interferon transcription factors [63], which give the virus the ability to escape from the immune system. The polymerase complex also plays an essential role in viral pathogenicity. For instance, to adapt to mammals, one of the avian influenza viral strategies is increasing the activity of the viral polymerase complex [10]. Moreover, the polymerase complex plays a special role in the pathogenicity or attenuation of influenza viruses. Attenuation may be considered as the reverse of pathogenicity [18]. In particular, mutations in PB2 and PB1 can convert the non-ts phenotype to ts, resulting in the attenuation of the strain. For instance, the modification of a cold-adapted attenuated influenza virus model and its wild-type (WT) progenitor using different methods (classical reassortment or plasmid-based reverse genetics system) demonstrated how replacing PB2 mutant genes in the attenuated model with PB2 from its WT progenitor results in a non-ts reassortant. On the other hand, replacing PB2 genes in the WT progenitor with mutant PB2 from the attenuated model results in a ts attenuated reassortant. The same results were obtained with a PB1 substitution [22,23,24,25].
Our molecular study showed that the A/South Africa/3626/2013 virus has three unique mutations in the polymerase complex (two in PB2 Asn-102-Thr, Glu-358-Glu/Lys and one in PB1 Gln-687-Arg). Gln-687-Arg localized in the C-terminus of PB1 [64]. Residues 678–757 in the C-terminus of PB1 form a binding site, which is required for tight-binding with PB2 through its N-terminus. Mutations in this position strongly affect polymerase activity [65]. Asn-102-Thr falls in the (PB2-N1) subdomain of the N-terminal third, and this subdomain acts as a support for the PB1 thumb domain [64]. Due to these data, we can assume that the two mutations might increase the polymerase stability and thus its activity, which could explain the high pathogenicity of the A/South Africa/3626/2013 virus.
Regarding the Glu-358-Glu/Lys substitution in PB2, Glu in this position is highly conservative among different influenza subtypes (in the alignment of 517 PB2 protein sequences of H1N1, H3N2, H2N2, H5N1, H5N8, H7N7, H7N9, and H9N2 animal and human influenza isolates; see Table 4). The Lys variant was detected in only one A/northern shoveler/Mississippi/11OS202/2011 (H7N7) influenza virus (GISAID sequence ID EPI419570) [34]. This amino acid position is part of the cap-binding domain of the PB2 protein [64], which suggests that this mutation might directly affect the polymerase activity. However, in our study, the heterogeneity persisted with an equal ratio even after passage in mice, demonstrating that the two variants had been replicated equally in mice’s lungs, which indicates that this substitution might not sufficiently affect the viral pathogenicity. Nevertheless, further investigation—including the reassortment of the gene fragments containing these three mutations—is required to affirm the roles of these three mutations in viral pathogenicity.
This entry is adapted from the peer-reviewed paper 10.3390/vaccines10030395
This entry is offline, you can click here to edit this entry!
