Cardiovascular diseases remain the most common cause of morbidity and mortality in chronic kidney disease patients undergoing hemodialysis. Epicardial adipose tissue (EAT), visceral fat depot of the heart, was found to be associated with coronary artery disease in cardiac and non-cardiac patients. Additionally, EAT has been proposed as a novel cardiovascular risk in the general population and in end-stage renal disease patients. It has also been shown that EAT, more than other subcutaneous adipose tissue deposits, acts as a highly active organ producing several bioactive adipokines, and proinflammatory and proatherogenic cytokines.
- epicardial adipose tissue
- cardiovascular morbidity and mortality
- hemodialysis
1. Relationship between CVD and EAT in End Stage Renal Disease (ESRD) Patients and Patients Receiving Hemodialysis Treatment
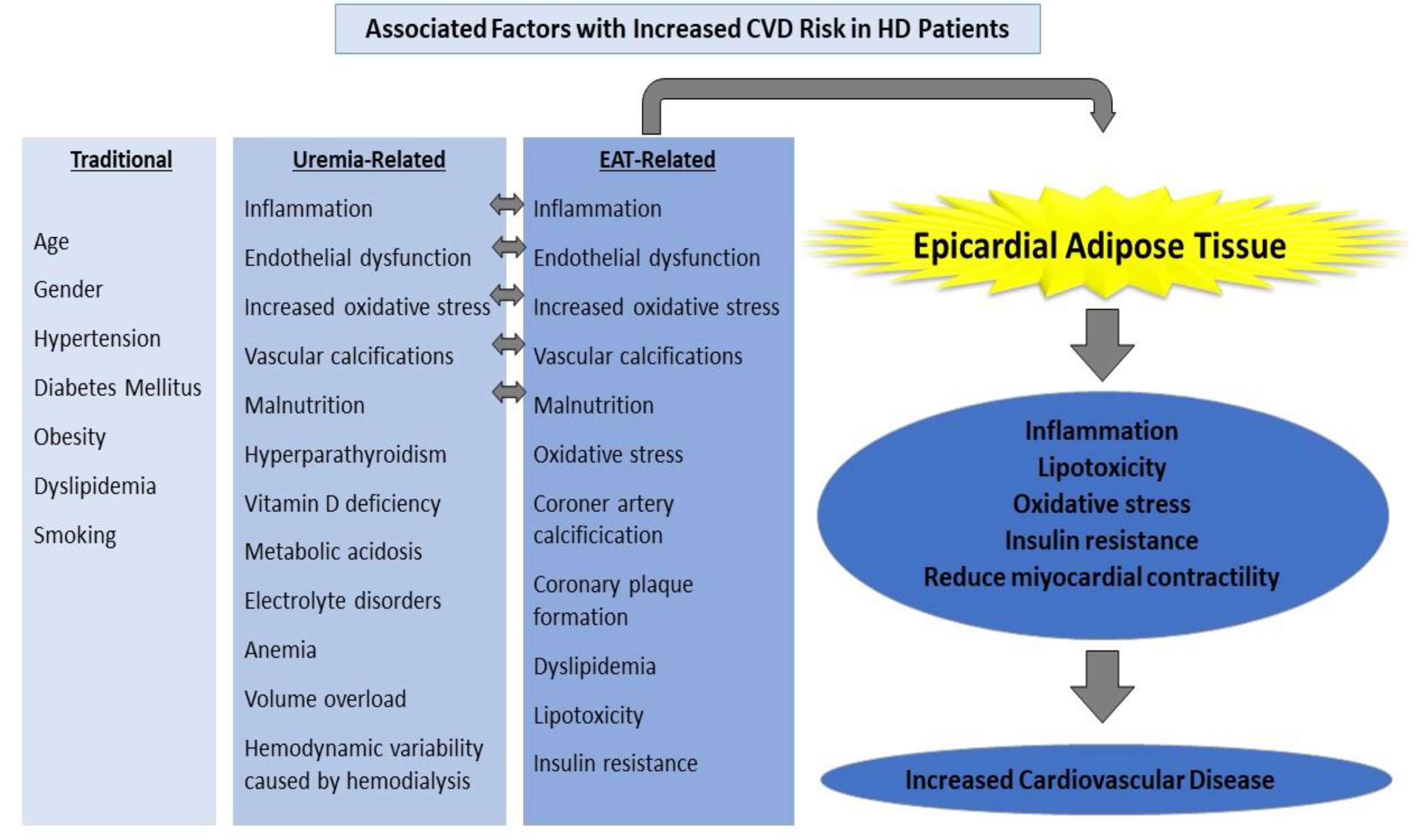
2. Risk Factors
3. Potential Solutions
This entry is adapted from the peer-reviewed paper 10.3390/jcm11051308
References
- Sarnak, M.J.; Amann, K.; Bangalore, S.; Cavalcante, J.L.; Charytan, D.M.; Craig, J.C.; Gill, J.S.; Hlatky, M.A.; Jardine, A.G.; Landmesser, U.; et al. Chronic Kidney Disease and Coronary Artery Disease: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2019, 74, 1823–1838.
- Abdallah, E.; El-Shishtawy, S.; Sherif, N.; Ali, A.; El-Bendary, O. Assessment of the relationship between serum paraoxonase activity and epicardial adipose tissue in hemodialysis patients. Int. Urol. Nephrol. 2017, 49, 329–335.
- Tonelli, M.; Karumanchi, S.A.; Thadhani, R. Epidemiology and Mechanisms of Uremia-Related Cardiovascular Disease. Circulation 2016, 133, 518–536.
- Nusair, M.B.; Rajpurohit, N.; Alpert, M.A. Chronic Inflammation and Coronary Atherosclerosis in Patients with End-Stage Renal Disease. Cardiorenal Med. 2012, 2, 117–124.
- Collins, A.J. Cardiovascular mortality in end-stage renal disease. Am. J. Med. Sci. 2003, 325, 163–167.
- Guérin, A.P.; London, G.M.; Marchais, S.J.; Metivier, F. Arterial stiffening and vascular calcifications in end-stage renal disease. Nephrol. Dial. Transplant. 2000, 15, 1014–1021.
- Stenvinkel, P.; Heimbürger, O.; Paultre, F.; Diczfalusy, U.; Wang, T.; Berglund, L.; Jogestrand, T. Strong association between malnutrition, inflammation, and atherosclerosis in chronic renal failure. Kidney Int. 1999, 55, 1899–1911.
- Tintut, Y.; Patel, J.; Parhami, F.; Demer, L.L. Tumor Necrosis Factor-α Promotes In Vitro Calcification of Vascular Cells via the cAMP Pathway. Circulation 2000, 102, 2636–2642.
- Miyazaki, H.; Matsuoka, H.; Itabe, H.; Usui, M.; Ueda, S.; Okuda, S.; Imaizumi, T. Hemodialysis impairs endothelial function via oxidative stress: Effects of vitamin E-coated dialyzer. Circulation 2000, 101, 1002–1006.
- Sasso, F.C.; Pafundi, P.C.; Simeon, V.; De Nicola, L.; Chiodini, P.; Galiero, R.; Rinaldi, L.; Nevola, R.; Salvatore, T.; Sardu, C.; et al. Efficacy and durability of multifactorial intervention on mortality and MACEs: A randomized clinical trial in type-2 diabetic kidney disease. Cardiovasc. Diabetol. 2021, 20, 1–12.
- Pimentel-Ramos, L.; Molina, F. Epicardial fatty tissue in association with adipocytokines as prognostic factors of cardiovascular disease in patients with advanced chronic kidney desease and hemodialysis. Nefrologia 2021.
- D’Marco, L.G.; Bellasi, A.; Kim, S.; Chen, Z.; Block, G.A.; Raggi, P. Epicardial adipose tissue predicts mortality in incident hemodialysis patients: A substudy of the Renagel in New Dialysis trial. Nephrol. Dial. Transplant. 2013, 28, 2586–2595.
- Baloglu, I.; Turkmen, K.; Selcuk, N.Y.; Tonbul, H.Z.; Ozcicek, A.; Hamur, H.; Iylsoy, S.; Akbas, E.M. The Relationship between Visceral Adiposity Index and Epicardial Adipose Tissue in Patients with Type 2 Diabetes Mellitus. Exp. Clin. Endocrinol. Diabetes 2019, 129, 390–395.
- Wilund, K.R.; Tomayko, E.J.; Wu, P.T.; Ryong Chung, H.; Vallurupalli, S.; Lakshminarayanan, B.; Fernhall, B. Intradialytic exercise training reduces oxidative stress and epicardial fat: A pilot study. Nephrol. Dial. Transplant. 2010, 25, 2695–2701.
- Akbas, E.M.; Demirtas, L.; Ozcicek, A.; Timuroglu, A.; Bakirci, E.M.; Hamur, H.; Ozcicek, F.; Turkmen, K. Association of epicardial adipose tissue, neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio with diabetic nephropathy. Int. J. Clin. Exp. Med. 2014, 7, 1794–1801.
- Marisa Costa, V.; Carvalho, F.; Kulkarni, P.; Salvatore, T.; Galiero, R.; Caturano, A.; Vetrano, E.; Rinaldi, L.; Coviello, F.; Di Martino, A.; et al. Dysregulated Epicardial Adipose Tissue as a Risk Factor and Potential Therapeutic Target of Heart Failure with Preserved Ejection Fraction in Diabetes. Biomolecules 2022, 12, 176.
- Kwon, S.S.; Choi, K.; Da Nam, B.; Lee, H.; Cho, N.J.; Park, B.W.; Kim, H.; Noh, H.; Jeon, J.S.; Han, D.C.; et al. Epicardial adipose tissue radiodensity is associated with all-cause mortality in patients undergoing hemodialysis. Sci. Rep. 2021, 11, 1–9.
- Cano Megías, M.; Guisado Vasco, P.; Bouarich, H.; Lara Aguilera, I.; de Arriba-de la Fuente, G.; Rodríguez-Puyol, D. Epicardial fat tissue, coronary arterial calcification and mortality in patients with advanced chronic kidney disease and hemodialysis. Nefrol 2021, 41, 174–181.
- Jeong, J.W.; Myung, H.J.; Kyeong, H.Y.; Seok, K.O.; Eun, M.P.; Yun, K.K.; Sang, J.R.; Eun, M.L.; Lee, J.; Nam, J.Y.; et al. Echocardiographic epicardial fat thickness and coronary artery disease. Circ. J. 2007, 71, 536–539.
- Chen, Y.C.; Lee, W.H.; Lee, M.K.; Hsu, P.C.; Tsai, W.C.; Chu, C.Y.; Lee, C.S.; Yen, H.W.; Lin, T.H.; Voon, W.C.; et al. Epicardial adipose tissue thickness is not associated with adverse cardiovascular events in patients undergoing haemodialysis. Sci. Rep. 2020, 10.
- Turkmen, K.; Tonbul, H.Z.; Erdur, F.M.; Guney, I.; Kayikcioglu, H.; Altintepe, L.; Ozbek, O.; Yilmaz, M.I.; Gaipov, A.; Turk, S.; et al. Peri-aortic fat tissue and malnutrition-inflammation-atherosclerosis/calcification syndrome in end-stage renal disease patients. Int. Urol. Nephrol. 2013, 45, 857–867.
- Turkmen, K.; Kayikcioglu, H.; Ozbek, O.; Solak, Y.; Kayrak, M.; Samur, C.; Anil, M.; Tonbul, H.Z. The relationship between epicardial adipose tissue and malnutrition, inflammation, atherosclerosis/calcification syndrome in ESRD patients. Clin. J. Am. Soc. Nephrol. 2011, 6, 1920–1925.
- Turkmen, K.; Ozbek, O.; Kayikcioğlu, H.; Kayrak, M.; Solak, Y.; Nayman, A.; Anil, M.; Babur, H.; Tonbul, H.Z. The Relationship between Epicardial Adipose Tissue and Coronary Artery Calcification in Peritoneal Dialysis Patients. Cardiorenal. Med. 2012, 2, 43–51.
- Barros, X.; Dirrichs, T.; Koos, R.; Reinartz, S.; Kaesler, N.; Kramann, R.; Gladziwa, U.; Ketteler, M.; Floege, J.; Marx, N.; et al. Epicardial adipose tissue in long-term hemodialysis patients: Its association with vascular calcification and long-term development. J. Nephrol. 2016, 29, 241–250.
- Atakan, A.; Macunluoglu, B.; Kaya, Y.; Ari, E.; Demir, H.; Asicioglu, E.; Kaspar, C. Epicardial fat thickness is associated with impaired coronary flow reserve in hemodialysis patients. Hemodial. Int. 2014, 18, 62–69.
- Le Jemtel, T.H.; Samson, R.; Milligan, G.; Jaiswal, A.; Oparil, S. Visceral Adipose Tissue Accumulation and Residual Cardiovascular Risk. Curr. Hypertens Rep. 2018, 20, 1–14.
- Cherian, S.; Lopaschuk, G.D.; Carvalho, E. Cellular cross-talk between epicardial adipose tissue and myocardium in relation to the pathogenesis of cardiovascular disease. Am. J. Physiol. Endocrinol. Metab. 2012, 303, 937–949.
- Iacobellis, G.; Barbaro, G. The double role of epicardial adipose tissue as pro- and anti-inflammatory organ. Horm. Metab. Res. 2008, 40, 442–445.
- Wang, T.D.; Lee, W.J.; Shih, F.Y.; Huang, C.H.; Chen, W.J.; Lee, Y.T.; Shih, T.T.F.; Chen, M.F. Association of epicardial adipose tissue with coronary atherosclerosis is region-specific and independent of conventional risk factors and intra-abdominal adiposity. Atherosclerosis 2010, 213, 279–287.
- Verhagen, S.N.; Visseren, F.L.J. Perivascular adipose tissue as a cause of atherosclerosis. Atherosclerosis 2011, 214, 3–10.
- McKenney-Drake, M.L.; Rodenbeck, S.D.; Bruning, R.S.; Kole, A.; Yancey, K.W.; Alloosh, M.; Sacks, H.S.; Sturek, M. Epicardial Adipose Tissue Removal Potentiates Outward Remodeling and Arrests Coronary Atherogenesis. Ann. Thorac. Surg. 2017, 103, 1622–1630.
- Saritas, T.; Reinartz, S.D.; Nadal, J.; Schmoee, J.; Schmid, M.; Marwan, M.; Achenbach, S.; Störk, S.; Wanner, C.; Eckardt, K.U.; et al. Epicardial fat, cardiovascular risk factors and calcifications in patients with chronic kidney disease. Clin. Kidney J. 2020, 13, 571.
- Çolak, H.; Kilicarslan, B.; Tekce, H.; Tanrisev, M.; Tugmen, C.; Aktas, G.; Kursat, S. Relationship between epicardial adipose tissue, inflammation and volume markers in hemodialysis and transplant patients. Ther. Apher. Dial. 2015, 19, 56–62.
- Iacobellis, G.; Willens, H.J. Echocardiographic Epicardial Fat: A Review of Research and Clinical Applications. J. Am. Soc. Echocardiogr. 2009, 22, 1311–1319.
- Nakanishi, K.; Fukuda, S.; Tanaka, A.; Otsuka, K.; Taguchi, H.; Yoshikawa, J.; Shimada, K. Epicardial Adipose Tissue Accumulation Is Associated With Renal Dysfunction and Coronary Plaque Morphology on Multidetector Computed Tomography. Circ J. 2016, 80, 196–201.
- Odamaki, M.; Furuya, R.; Ohkawa, S.; Yoneyama, T.; Nishikino, M.; Hishida, A.; Kumagai, H. Altered abdominal fat distribution and its association with the serum lipid profile in non-diabetic haemodialysis patients. Nephrol. Dial. Transplant. 1999, 14, 2427–2432.
- Zeki Tonbul, H.; Demir, M.; Altintepe, L.; Güney, I.; Yeter, E.; Türk, S.; Yeksan, M.; Yildiz, A. Malnutrition-inflammation-atherosclerosis (MIA) syndrome components in hemodialysis and peritoneal dialysis patients. Ren. Fail. 2006, 28, 287–294.
- Lin, H.H.; Lee, J.K.; Yang, C.Y.; Lien, Y.C.; Huang, J.W.; Wu, C.K. Accumulation of epicardial fat rather than visceral fat is an independent risk factor for left ventricular diastolic dysfunction in patients undergoing peritoneal dialysis. Cardiovasc. Diabetol. 2013, 12, 127.
- Oikawa, M.; Owada, T.; Yamauchi, H.; Misaka, T.; Machii, H.; Yamaki, T.; Sugimoto, K.; Kunii, H.; Nakazato, K.; Suzuki, H.; et al. Epicardial adipose tissue reflects the presence of coronary artery disease: Comparison with abdominal visceral adipose tissue. Biomed. Res. Int. 2015, 2015.
- Versteylen, M.O.; Takx, R.A.P.; Joosen, I.A.P.G.; Nelemans, P.J.; Das, M.; Crijns, H.J.G.M.; Hofstra, L.; Leiner, T. Epicardial adipose tissue volume as a predictor for coronary artery disease in diabetic, impaired fasting glucose, and non-diabetic patients presenting with chest pain. Eur. Hear. J. Cardiovasc. Imaging. 2012, 13, 517–523.
- Cheng, K.H.; Chu, C.S.; Lee, K.T.; Lin, T.H.; Hsieh, C.C.; Chiu, C.C.; Voon, W.C.; Sheu, S.H.; Lai, W.T. Adipocytokines and proinflammatory mediators from abdominal and epicardial adipose tissue in patients with coronary artery disease. Int. J. Obes. 2008, 32, 268–274.
- Tonbul, H.Z.; Turkmen, K.; Kayikcioglu, H.; Ozbek, O.; Kayrak, M.; Biyik, Z. Epicardial adipose tissue and coronary artery calcification in diabetic and nondiabetic end-stage renal disease patients. Ren. Fail. 2011, 33, 770–775.
- Mazurek, T.; Zhang, L.F.; Zalewski, A.; Mannion, J.D.; Diehl, J.T.; Arafat, H.; Sarov-Blat, L.; O’Brien, S.; Keiper, E.A.; Johnson, A.G.; et al. Human Epicardial Adipose Tissue Is a Source of Inflammatory Mediators. Circulation 2003, 108, 2460–2466.
- Yilmaz, Z.; İnce, H.; Aydin, E.; Yildirim, Y.; Aydin, F.Y.; Yüksel, E.; Karabulut, A.; Dursun, L.; Kadiroğlu, A.K.; Yilmaz, M. Relationship Between Epicardial Adipose Tissue and Body Composition as Determined by Multi-Frequency Bioelectrical Impedance Analysis in Patients with Stage 5 Chronic Kidney Disease. Med. Sci. Monit. 2020, 26, e920233-1.
- Cordeiro, A.C.; Amparo, F.C.; Oliveira, M.A.C.; Amodeo, C.; Smanio, P.; Pinto, I.M.F.; Lindholm, B.; Stenvinkel, P.; Carrero, J.J. Epicardial fat accumulation, cardiometabolic profile and cardiovascular events in patients with stages 3-5 chronic kidney disease. J. Intern. Med. 2015, 278, 77–87.
- Gaeta, M.; Bandera, F.; Tassinari, F.; Capasso, L.; Cargnelutti, M.; Pelissero, G.; Malavazos, A.E.; Ricci, C. Is epicardial fat depot associated with atrial fibrillation? A systematic review and meta-analysis. Europace 2017, 19, 747–752.
- Fitzgibbons, T.P.; Czech, M.P. Epicardial and perivascular adipose tissues and their influence on cardiovascular disease: Basic mechanisms and clinical associations. J. Am. Heart Assoc. 2014, 3.
- Altun, B.; Tasolar, H.; Eren, N.; Binnetoʇlu, E.; Altun, M.; Temiz, A.; Gazi, E.; Barutcu, A.; Altunoren, O.; Colkesen, Y.; et al. Epicardial adipose tissue thickness in hemodialysis patients. Echocardiography 2014, 31, 941–946.
- Cai, S.; Wald, R.; Deva, D.P.; Kiaii, M.; Ng, M.Y.; Karur, G.R.; Bello, O.; Li, Z.J.; Leipsic, J.; Jimenez-Juan, L. Cardiac MRI measurements of pericardial adipose tissue volumes in patients on in-centre nocturnal hemodialysis. J. Nephrol. 2020, 33, 355–363.
- Ulusal Okyay, G.; Okyay, K.; Polattaş Solak, E.; Sahinarslan, A.; Paşaoğlu, Ö.; Ayerden Ebinç, F.; Paşaoğlu, H.; Boztepe Derici, Ü.; Sindel, Ş.; Arinsoy, T. Echocardiographic epicardial adipose tissue measurements provide information about cardiovascular risk in hemodialysis patients. Hemodial. Int. 2015, 19, 452–462.
- Graham-Brown, M.P.M.; McCann, G.P.; Burton, J.O. Epicardial adipose tissue in patients with end-stage renal disease on haemodialysis. Curr. Opin. Nephrol. Hypertens. 2015, 24, 517–524.
- Iacobellis, G.; Singh, N.; Wharton, S.; Sharma, A.M. Substantial changes in epicardial fat thickness after weight loss in severely obese subjects. Obesity 2008, 16, 1693–1697.
- Launbo, N.; Zobel, E.H.; von Scholten, B.J.; Færch, K.; Jørgensen, P.G.; Christensen, R.H. Targeting epicardial adipose tissue with exercise, diet, bariatric surgery or pharmaceutical interventions: A systematic review and meta-analysis. Obes. Rev. 2021, 22.
- Parisi, V.; Petraglia, L.; D’Esposito, V.; Cabaro, S.; Rengo, G.; Caruso, A.; Grimaldi, M.G.; Baldascino, F.; De Bellis, A.; Vitale, D.; et al. Statin therapy modulates thickness and inflammatory profile of human epicardial adipose tissue. Int. J. Cardiol. 2019, 274, 326–330.
