Osteoarthritis (OA) can be defined as the result of pathological processes of various etiologies leading to damage to the articular structures. Although the mechanism of degenerative changes has become better understood due to the plethora of biochemical and genetic studies, the drug that could stop the degenerative cascade is still unknown. All available forms of OA therapy are based on symptomatic treatment.
- osteoarthritis (OA)
- pharmacotherapies
- disease-modifying drugs for osteoarthritis (DMOADs)
1. Introduction
Arthritis is classified into various types, including osteoarthritis, rheumatoid arthritis (RA, ICD-10-CM code: M06 [1]), gouty arthritis, septic arthritis (SA), and psoriatic arthritis (PsA). Among them, RA and OA are the most common types of arthritis in the human population affecting about 302 million people [2]. Hallmarks of RA include inflammatory changes in the synovial membranes and articular structures, widespread fibrinoid degeneration of the collagen fibers in mesenchymal tissues as well as atrophy and rarefaction of bony structures. RA can also affect body parts other than joints, such as the eyes, mouth, and lungs. The etiology of RA is unknown, but most commonly autoimmune mechanisms have been implicated. In autoimmune diseases, the body’s immune cells attack the body’s tissues [3]. On the other hand, OA (ICD-10-CM code: M15-M19 [4]) is a complex, multifactorial disease. It can occur in any joint, mainly targeting the major joints (knee, hip, and back); nevertheless, it commonly affects hands, elbows, and ankles [5]. It is characterized by degeneration of the articular cartilage that ultimately leads to joint destruction [6]. The pathological changes of OA involve the entire joint, which is composed of multiple types of tissues and cells, exemplified by cartilage degradation, subchondral bone thickening, osteophyte formation, synovium inflammation, and hypertrophy, as well as ligament degeneration [7][8]. Both RA and OA commonly cause chronic pain, reduce motion in joints, and will become more prevalent given the aging population [9]. They have several underlying causes, including biochemical and mechanical factors [10][11]. In general, these diseases are progressive and no widely applied effective therapy is available [12].
2. The First-Line Therapy of Osteoarthritis
3. Platelet-Rich Plasma (PRP)/Platelet-Rich Fibrin (PRF) as Second Line Treatment
This entry is adapted from the peer-reviewed paper 10.3390/ijms23031566
References
- International Classification of Diseases. Available online: https://www.icd10data.com/ICD10CM/Codes/M00-M99/M05-M14/M06-/M06.9 (accessed on 10 January 2022).
- Kolasinski, S.L.; Neogi, T.; Hochberg, M.C.; Oatis, C.; Guyatt, G.; Block, J.; Callahan, L.; Copenhaver, C.; Dodge, C.; Felson, D. 2019 American College of Rheumatology/Arthritis Foundation guideline for the management of osteoarthritis of the hand, hip, and knee. Arthritis Rheumatol. 2020, 72, 220–233.
- Neidhart, S.; Neidhart, M. Rheumatoid arthritis and the concept of autoimmune disease. Int. J. Clin. Rheumatol. 2019, 14, 75.
- International Classification of Diseases. Available online: https://www.icd10data.com/ICD10CM/Codes/M00-M99/M15-M19 (accessed on 10 January 2022).
- Gabay, O. Osteoarthritis: New perspectives. J. Spine 2012, 1, e101.
- Zhu, Y.; Yuan, M.; Meng, H.; Wang, A.; Guo, Q.; Wang, Y.; Peng, J. Basic science and clinical application of platelet-rich plasma for cartilage defects and osteoarthritis: A review. Osteoarthr. Cartil. 2013, 21, 1627–1637.
- Huang, J.; Zhao, L.; Chen, D. Growth factor signalling in osteoarthritis. Growth Factors 2018, 36, 187–195.
- Szwedowski, D.; Szczepanek, J.; Paczesny, Ł.; Pękała, P.; Zabrzyński, J.; Kruczyński, J. Genetics in Cartilage Lesions: Basic Science and Therapy Approaches. IJMS 2020, 21, 5430.
- Denk, F.; Bennett, D.L.; McMahon, S.B. Nerve growth factor and pain mechanisms. Annu. Rev. Neurosci. 2017, 40, 307–325.
- Abramson, S.B. Nitric oxide in inflammation and pain associated with osteoarthritis. Arthritis Res. Ther. 2008, 10, 1–7.
- Malemud, C.J. The biological basis of osteoarthritis: State of the evidence. Curr. Opin. Rheumatol. 2015, 27, 289.
- Van Der Kraan, P.M. Differential role of transforming growth factor-beta in an osteoarthritic or a healthy joint. J. Bone Metab. 2018, 25, 65.
- Glazier, R.H.; Dalby, D.M.; Badley, E.M.; Hawker, G.A.; Bell, M.J.; Buchbinder, R.; Lineker, S.C. Management of common musculoskeletal problems: Survey of Ontario primary care physicians. CMAJ 1998, 158, 1037–1040.
- Gnylorybov, A.M.; Ter-Vartanian, S.K.; Golovach, I.Y.; Vyrva, O.E.; Burianov, O.A.; Yesirkepova, G.S.; Irismetov, M.E.; Rizamuhamedova, M.Z.; Vardanyan, V.S.; Ginosyan, K.V. Expert Opinion on the Extensive Use of Prescription Crystalline Glucosamine Sulfate in the Multimodal Treatment of Osteoarthritis in Ukraine, Kazakhstan, Uzbekistan, and Armenia. Clin. Med. Insights Arthritis Musculoskelet. Disord. 2020, 13, 1–9.
- Daste, C.; Kirren, Q.; Akoum, J.; Lefèvre-Colau, M.-M.; Rannou, F.; Nguyen, C. Physical activity for osteoarthritis: Efficiency and review of recommandations. Jt. Bone Spine 2021, 88, 105207.
- Jevsevar, D.S.; Brown, G.A.; Jones, D.L.; Matzkin, E.G.; Manner, P.A.; Mooar, P.; Schousboe, J.T.; Stovitz, S.; Sanders, J.O.; Bozic, K.J.; et al. The American Academy of Orthopaedic Surgeons Evidence-Based Guideline on: Treatment of Osteoarthritis of the Knee, 2nd Edition. JBJS 2013, 95, 1885–1886.
- Quinn, R.H.; Murray, J.; Pezold, R.; Hall, Q. Management of osteoarthritis of the hip: Evidence-based clinical practice guideline. J. Am. Acad. Orthop. Surg. 2017, 26, e434–e436.
- Bannuru, R.R.; Osani, M.; Vaysbrot, E.; Arden, N.; Bennell, K.; Bierma-Zeinstra, S.; Kraus, V.; Lohmander, L.S.; Abbott, J.; Bhandari, M. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarth. Cartil. 2019, 27, 1578–1589.
- Geenen, R.; Overman, C.L.; Christensen, R.; Åsenlöf, P.; Capela, S.; Huisinga, K.L.; Husebø, M.E.P.; Köke, A.J.; Paskins, Z.; Pitsillidou, I.A. EULAR recommendations for the health professional’s approach to pain management in inflammatory arthritis and osteoarthritis. Ann. Rheum. Dis. 2018, 77, 797–807.
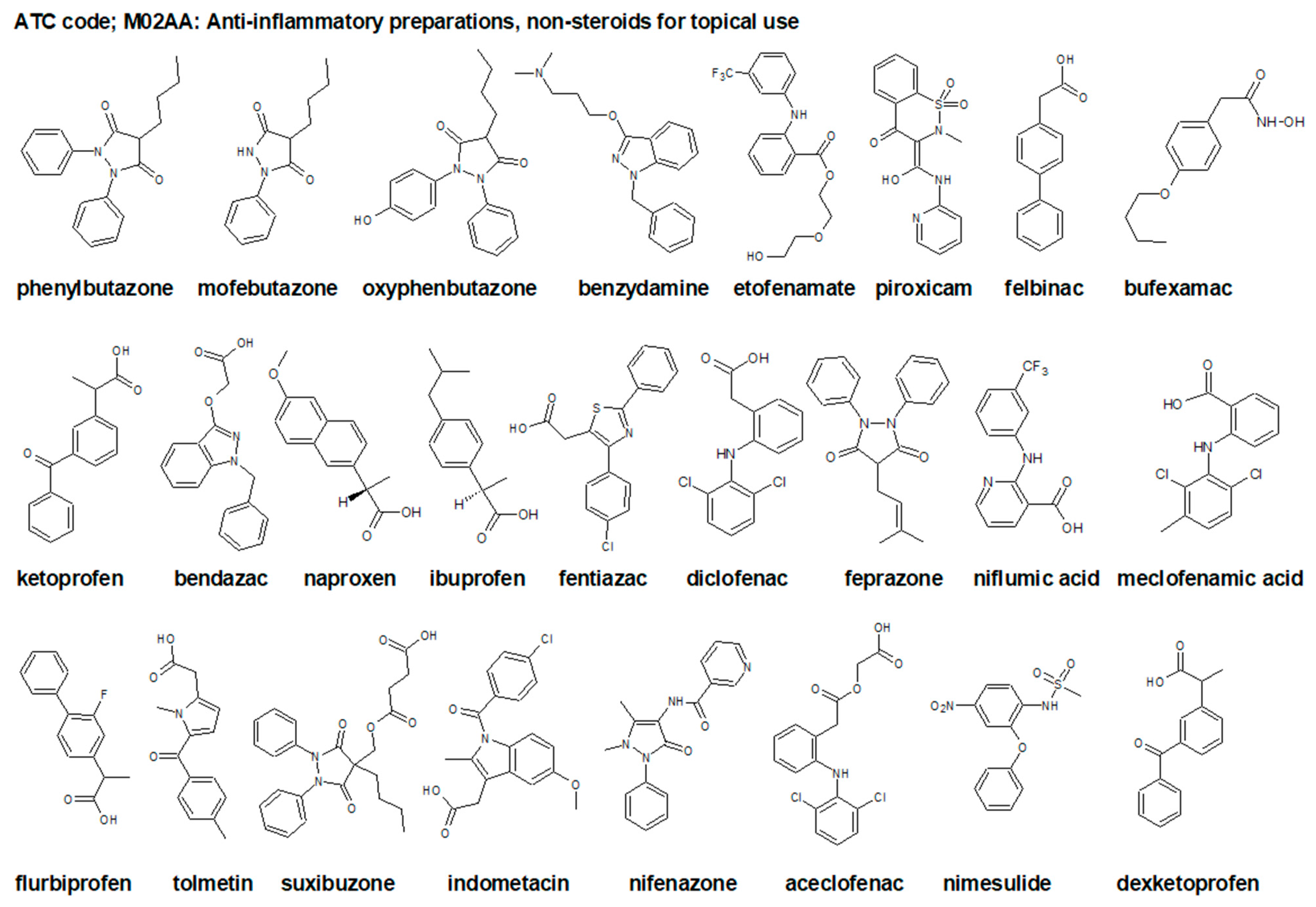
- Anatomical Therapeutic Chemical Classification System. Available online: https://www.whocc.no/atc_ddd_index/?code=M&showdescription=no (accessed on 10 January 2022).
- Anatomical Therapeutic Chemical Classification System. Available online: https://www.atccode.com/M02A (accessed on 10 January 2022).
- Anatomical Therapeutic Chemical Classification System. Available online: https://www.atccode.com/M02AA (accessed on 10 January 2022).
- Akram, M.; Daniyal, M.; Sultana, S.; Owais, A.; Akhtar, N.; Zahid, R.; Said, F.; Bouyahya, A.; Ponomarev, E.; Shariat, M.A. Traditional and modern management strategies for rheumatoid arthritis. Clin. Chim. Acta 2021, 512, 142–155.
- Pflugbeil, S.; Böckl, K.; Pongratz, R.; Leitner, M.; Graninger, W.; Ortner, A. Drug interactions in the treatment of rheumatoid arthritis and psoriatic arthritis. Rheumatol. Int. 2020, 40, 511–521.
- Marx, R.E. Platelet-Rich plasma (PRP): What is PRP and what is not PRP? Implant Dent. 2001, 10, 225–228.
- Gato-Calvo, L.; Magalhaes, J.; Ruiz-Romero, C.; Blanco, F.J.; Burguera, E.F. Platelet-Rich plasma in osteoarthritis treatment: Review of current evidence. Ther. Adv. Chronic. Dis. 2019, 10, 2040622319825567.
- Lichtenfels, M.; Colomé, L.; Sebben, A.D.; Braga-Silva, J. Effect of platelet rich plasma and platelet rich fibrin on sciatic nerve regeneration in a rat model. Microsurgery 2013, 33, 383–390.
- Eppley, B.L.; Pietrzak, W.S.; Blanton, M. Platelet-rich plasma: A review of biology and applications in plastic surgery. Plast. Reconst. Surg. 2006, 118, 147e–159e.
- Mościcka, P.; Przylipiak, A. History of autologous platelet-rich plasma: A short review. J. Cosmet. Dermatol. 2021, 20, 2712–2714.
- Anitua, E.; Aguirre, J.J.; Algorta, J.; Ayerdi, E.; Cabezas, A.I.; Orive, G.; Andia, I. Effectiveness of autologous preparation rich in growth factors for the treatment of chronic cutaneous ulcers. J. Biomed. Mater. Res. Part B Appl. Biomater. 2008, 84, 415–421.
- Anitua, E. Plasma rich in growth factors: Preliminary results of use in the preparation of future sites for implants. Int. J. Oral Maxillofac. Implant. 1999, 14, 529–535.
- Filardo, G.; Previtali, D.; Napoli, F.; Candrian, C.; Zaffagnini, S.; Grassi, A. PRP injections for the treatment of knee osteoarthritis: A meta-analysis of randomized controlled trials. Cartilage 2021, 13 (Suppl. 1), 364S–375S.
- Ahmad, H.S.; Farrag, S.E.; Okasha, A.E.; Kadry, A.O.; Ata, T.B.; Monir, A.A.; Shady, I. Clinical outcomes are associated with changes in ultrasonographic structural appearance after platelet-rich plasma treatment for knee osteoarthritis. Int. J. Rheum. Dis. 2018, 21, 960–966.
