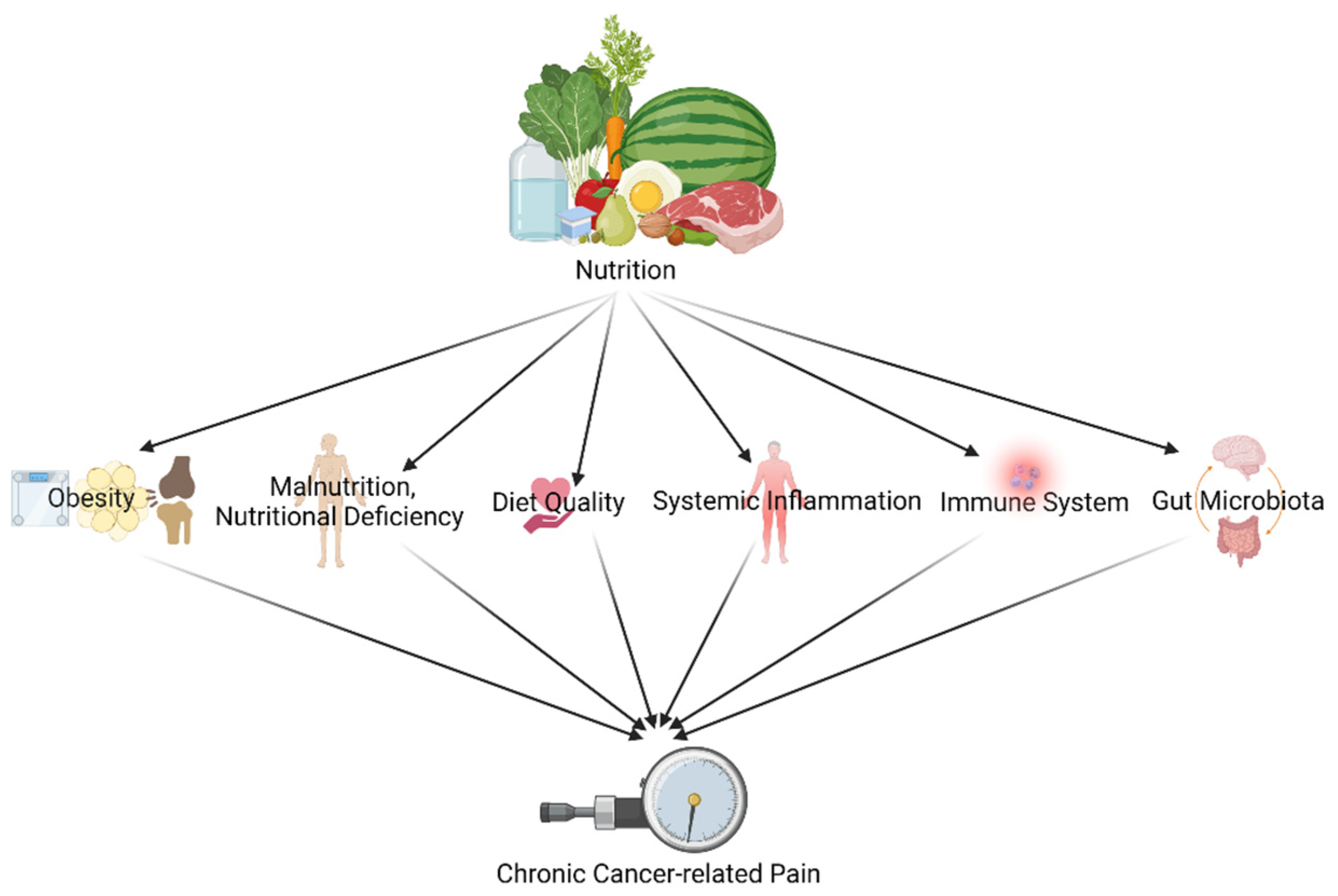
Chronic pain in cancer survivors is related to obesity, malnutrition, nutritional deficiency, diet quality, immune system, systemic inflammation, and gut microbiota. As seen clearly, dietary interventions may provide weight reduction, a healthy body weight, good diet quality, regulations in systemic inflammation and immune system, and a healthy gut microbiota environment that could modify aforementioned pain-related pathways/mechanisms. For that reason, nutrition might have the potential to transition from being only prevention for cancer recurrence or cancer itself to a modality for chronic pain management for cancer survivors.
- cancer survivors
- chronic pain
- pain management
- nutrition
- diet
1. Pain and Nutrition in Cancer Survivors: An Update from Cancer and Chronic Pain Literature
2. Impact of Diet and Nutrition on Pain in Cancer Survivors through Obesity
3. Impact of Diet and Nutrition on Pain in Cancer Survivors through Malnutrition, Nutritional Deficiency, and Diet Quality
4. Impact of Diet and Nutrition on Pain in Cancer Survivors through the Immune System and Systemic Inflammation
5. Impact of Diet and Nutrition on Pain in Cancer Survivors through Gut Microbiota
This entry is adapted from the peer-reviewed paper 10.3390/jcm11030653
References
- Bjørklund, G.; Aaseth, J.; Doşa, M.D.; Pivina, L.; Dadar, M.; Pen, J.J.; Chirumbolo, S. Does diet play a role in reducing nociception related to inflammation and chronic pain? Nutrition 2019, 66, 153–165. [Google Scholar] [CrossRef] [PubMed]
- Tapsell, L.C. Dietary behaviour changes to improve nutritional quality and health outcomes. Chronic Dis. Transl. Med. 2017, 3, 154–158. [Google Scholar] [CrossRef]
- Ren, K.; Dubner, R. Interactions between the immune and nervous systems in pain. Nat. Med. 2010, 16, 1267–1276. [Google Scholar] [CrossRef]
- Malafoglia, V.; Ilari, S.; Vitiello, L.; Tenti, M.; Balzani, E.; Muscoli, C.; Raffaeli, W.; Bonci, A. The Interplay between Chronic Pain, Opioids, and the Immune System. Neuroscientist 2021, 10738584211030493. [Google Scholar] [CrossRef]
- Parekh, N.; Chandran, U.; Bandera, E.V. Obesity in Cancer Survival. Annu. Rev. Nutr. 2012, 32, 311–342. [Google Scholar] [CrossRef]
- Buch, K.; Gunmalm, V.; Andersson, M.; Schwarz, P.; Brøns, C. Effect of chemotherapy and aromatase inhibitors in the adjuvant treatment of breast cancer on glucose and insulin metabolism-A systematic review. Cancer Med. 2019, 8, 238–245. [Google Scholar] [CrossRef] [PubMed]
- Cox-Martin, E.; Trahan, L.H.; Cox, M.G.; Dougherty, P.M.; Lai, E.A.; Novy, D.M. Disease burden and pain in obese cancer patients with chemotherapy-induced peripheral neuropathy. Support. Care Cancer 2017, 25, 1873–1879. [Google Scholar] [CrossRef] [PubMed]
- Morelhão, P.K.; Tufik, S.; Andersen, M.L. The Interactions Between Obesity, Sleep Quality, and Chronic Pain. J. Clin. Sleep Med. 2018, 14, 1965–1966. [Google Scholar] [CrossRef] [PubMed]
- Mínguez-Olaondo, A.; Martínez-Valbuena, I.; Romero, S.; Frühbeck, G.; Luquin, M.R.; Martínez-Vila, E.; Irimia, P. Excess abdominal fat is associated with cutaneous allodynia in individuals with migraine: A prospective cohort study. J. Headache Pain 2020, 21, 9. [Google Scholar] [CrossRef]
- Emery, C.F.; Olson, K.L.; Bodine, A.; Lee, V.; Habash, D.L. Dietary intake mediates the relationship of body fat to pain. Pain 2017, 158, 273–277. [Google Scholar] [CrossRef]
- Pellegrini, M.; Ippolito, M.; Monge, T.; Violi, R.; Cappello, P.; Ferrocino, I.; Cocolin, L.S.; De Francesco, A.; Bo, S.; Finocchiaro, C. Gut microbiota composition after diet and probiotics in overweight breast cancer survivors: A randomized open-label pilot intervention trial. Nutrition 2020, 74, 110749. [Google Scholar] [CrossRef]
- Minerbi, A.; Gonzalez, E.; Brereton, N.J.; Anjarkouchian, A.; Dewar, K.; Fitzcharles, M.-A.; Chevalier, S.; Shir, Y. Altered microbiome composition in individuals with fibromyalgia. Pain 2019, 160, 2589–2602. [Google Scholar] [CrossRef]
- Timmins, H.C.; Mizrahi, D.; Li, T.; Kiernan, M.C.; Goldstein, D.; Park, S.B. Metabolic and lifestyle risk factors for chemotherapy-induced peripheral neuropathy in taxane and platinum-treated patients: A systematic review. J. Cancer Surviv. 2021, 1–15. [Google Scholar] [CrossRef]
- Forsythe, L.P.; Alfano, C.M.; George, S.M.; McTiernan, A.; Baumgartner, K.B.; Bernstein, L.; Ballard-Barbash, R. Pain in long-term breast cancer survivors: The role of body mass index, physical activity, and sedentary behavior. Breast Cancer Res. Treat. 2013, 137, 617–630. [Google Scholar] [CrossRef]
- Mosher, C.E.; Sloane, R.; Morey, M.C.; Snyder, D.C.; Cohen, H.J.; Miller, P.E.; Demark-Wahnefried, W. Associations between lifestyle factors and quality of life among older long-term breast, prostate, and colorectal cancer survivors. Cancer Interdiscip. Int. J. Am. Cancer Soc. 2009, 115, 4001–4009. [Google Scholar] [CrossRef]
- Leysen, L.; Beckwée, D.; Nijs, J.; Pas, R.; Bilterys, T.; Vermeir, S.; Adriaenssens, N. Risk factors of pain in breast cancer survivors: A systematic review and meta-analysis. Support. Care Cancer 2017, 25, 3607–3643. [Google Scholar] [CrossRef]
- Petrovchich, I.; Kober, K.M.; Wagner, L.; Paul, S.M.; Abrams, G.; Chesney, M.A.; Topp, K.; Smoot, B.; Schumacher, M.; Conley, Y.P. Deleterious effects of higher body mass index on subjective and objective measures of chemotherapy-induced peripheral neuropathy in cancer survivors. J. Pain Symptom Manag. 2019, 58, 252–263. [Google Scholar] [CrossRef] [PubMed]
- Sheng, J.Y.; Santa-Maria, C.A.; Blackford, A.L.; Lim, D.; Carpenter, A.; Smith, K.L.; Cohen, G.I.; Coughlin, J.; Appel, L.J.; Stearns, V. The impact of weight loss on physical function and symptoms in overweight or obese breast cancer survivors: Results from POWER-remote. J. Cancer Surviv. 2021. online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Cederholm, T.; Jensen, G.L. To create a consensus on malnutrition diagnostic criteria: A report from the Global Leadership Initiative on Malnutrition (GLIM) meeting at the ESPEN Congress 2016. J. Parenter. Enter. Nutr. 2017, 41, 311–314. [Google Scholar] [CrossRef] [PubMed]
- Prevost, V.; Joubert, C.; Heutte, N.; Babin, E. Assessment of nutritional status and quality of life in patients treated for head and neck cancer. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 2014, 131, 113–120. [Google Scholar] [CrossRef]
- Argiles, J.M. Cancer-associated malnutrition. Eur. J. Oncol. Nurs. 2005, 9 (Suppl. S2), S39–S50. [Google Scholar] [CrossRef]
- Field, R.; Pourkazemi, F.; Turton, J.; Rooney, K. Dietary Interventions Are Beneficial for Patients with Chronic Pain: A Systematic Review with Meta-Analysis. Pain Med. 2021, 22, 694–714. [Google Scholar] [CrossRef]
- Mohammadi, S.; Sulaiman, S.; Koon, P.B.; Amani, R.; Hosseini, S.M. Association of Nutritional Status with Quality of Life in Breast Cancer Survivors. Asian Pac. J. Cancer Prev. 2013, 14, 7749–7755. [Google Scholar] [CrossRef]
- Capra, S.; Ferguson, M.; Ried, K. Cancer: Impact of nutrition intervention outcome—Nutrition issues for patients. Nutrition 2001, 17, 769–772. [Google Scholar] [CrossRef]
- De Vries, Y.; Van Den Berg, M.; De Vries, J.; Boesveldt, S.; de Kruif, J.T.C.; Buist, N.; Haringhuizen, A.; Los, M.; Sommeijer, D.; Timmer-Bonte, J. Differences in dietary intake during chemotherapy in breast cancer patients compared to women without cancer. Supportive Care Cancer 2017, 25, 2581–2591. [Google Scholar] [CrossRef]
- Inglis, J.E.; Lin, P.-J.; Kerns, S.L.; Kleckner, I.R.; Kleckner, A.S.; Castillo, A.D.; Mustian, K.M.; Peppone, L.J. Nutritional Interventions for Treating Cancer-Related Fatigue: A Qualitative Review. Nutr. Cancer 2019, 71, 21–40. [Google Scholar] [CrossRef] [PubMed]
- Petzel, M.Q.B.; Hoffman, L. Nutrition Implications for Long-Term Survivors of Pancreatic Cancer Surgery. Nutr. Clin. Pract. 2017, 32, 588–598. [Google Scholar] [CrossRef]
- Hu, Y.; Kim, H.-I.; Hyung, W.J.; Song, K.J.; Lee, J.H.; Kim, Y.M.; Noh, S.H. Vitamin B12 deficiency after gastrectomy for gastric cancer: An analysis of clinical patterns and risk factors. Ann. Surg. 2013, 258, 970–975. [Google Scholar] [CrossRef] [PubMed]
- Philpot, U.; Johnson, M. Diet therapy in the management of chronic pain: Better diet less pain? Pain Manag. 2019, 9, 335–338. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.-H.; Kang, J.W.; Lee, T.H. Therapeutic options for aromatase inhibitor-associated arthralgia in breast cancer survivors: A systematic review of systematic reviews, evidence mapping, and network meta-analysis. Maturitas 2018, 118, 29–37. [Google Scholar] [CrossRef] [PubMed]
- Dragan, S.; Șerban, M.-C.; Damian, G.; Buleu, F.; Valcovici, M.; Christodorescu, R. Dietary Patterns and Interventions to Alleviate Chronic Pain. Nutrients 2020, 12, 2510. [Google Scholar] [CrossRef]
- Niravath, P.; Chen, B.; Chapman, J.-A.W.; Agarwal, S.K.; Welschhans, R.L.; Bongartz, T.; Kalari, K.R.; Shepherd, L.E.; Bartlett, J.; Pritchard, K. Vitamin D levels, vitamin D receptor polymorphisms, and inflammatory cytokines in aromatase inhibitor-induced Arthralgias: An analysis of CCTG MA. 27. Clin. Breast Cancer 2018, 18, 78–87. [Google Scholar] [CrossRef]
- Martin, K.R.; Reid, D.M. Is there a role for vitamin D in the treatment of chronic pain? Ther. Adv. Musculoskelet. Dis. 2017, 9, 131–135. [Google Scholar] [CrossRef]
- Carr, A.C.; McCall, C. The role of vitamin C in the treatment of pain: New insights. J. Transl. Med. 2017, 15, 77. [Google Scholar] [CrossRef]
- Carr, A.C.; Vissers, M.C.M.; Cook, J.S. The Effect of Intravenous Vitamin C on Cancer- and Chemotherapy-Related Fatigue and Quality of Life. Front. Oncol. 2014, 4, 283. [Google Scholar] [CrossRef]
- Chao, C.; Bhatia, S.; Xu, L.; Cannavale, K.L.; Wong, F.L.; Huang, P.S.; Cooper, R.; Armenian, S.H. Chronic Comorbidities Among Survivors of Adolescent and Young Adult Cancer. J. Clin. Oncol. 2020, 38, 3161. [Google Scholar] [CrossRef]
- Porciello, G.; Montagnese, C.; Crispo, A.; Grimaldi, M.; Libra, M.; Vitale, S.; Palumbo, E.; Pica, R.; Calabrese, I.; Cubisino, S. Mediterranean diet and quality of life in women treated for breast cancer: A baseline analysis of DEDiCa multicentre trial. PLoS ONE 2020, 15, e0239803. [Google Scholar] [CrossRef] [PubMed]
- Wayne, S.J.; Baumgartner, K.; Baumgartner, R.N.; Bernstein, L.; Bowen, D.J.; Ballard-Barbash, R. Diet quality is directly associated with quality of life in breast cancer survivors. Breast Cancer Res. Treat. 2006, 96, 227–232. [Google Scholar] [CrossRef] [PubMed]
- Koh, D.; Song, S.; Moon, S.-E.; Jung, S.-Y.; Lee, E.S.; Kim, Z.; Youn, H.J.; Cho, J.; Yoo, Y.B.; Lee, S.K. Adherence to the American Cancer Society guidelines for cancer survivors and health-related quality of life among breast cancer survivors. Nutrients 2019, 11, 2924. [Google Scholar] [CrossRef]
- Lei, Y.-Y.; Ho, S.C.; Cheng, A.; Kwok, C.; Lee, C.-K.I.; Cheung, K.L.; Lee, R.; Loong, H.H.; He, Y.-Q.; Yeo, W. Adherence to the World Cancer Research Fund/American Institute for Cancer Research Guideline is associated with better health-related quality of life among Chinese patients with breast cancer. J. Natl. Compr. Cancer Netw. 2018, 16, 275–285. [Google Scholar] [CrossRef]
- Brown, M.; Farquhar-Smith, P. Pain in cancer survivors; filling in the gaps. Br. J. Anaesth. 2017, 119, 723–736. [Google Scholar] [CrossRef] [PubMed]
- Christensen, M.A.; Smoak, P.; Lisano, J.K.; Hayward, R.; Coronado, C.; Kage, K.; Shackelford, D.; Stewart, L.K. Cardiorespiratory fitness, visceral fat, and body fat, but not dietary inflammatory index, are related to C-reactive protein in cancer survivors. Nutr. Health 2019, 25, 195–202. [Google Scholar] [CrossRef]
- Alfano, C.M.; Imayama, I.; Neuhouser, M.L.; Kiecolt-Glaser, J.K.; Smith, A.W.; Meeske, K.; McTiernan, A.; Bernstein, L.; Baumgartner, K.B.; Ulrich, C.M. Fatigue, inflammation, and ω-3 and ω-6 fatty acid intake among breast cancer survivors. J. Clin. Oncol. 2012, 30, 1280. [Google Scholar] [CrossRef]
- Kurtys, E.; Eisel, U.; Verkuyl, J.; Broersen, L.; Dierckx, R.; de Vries, E. The combination of vitamins and omega-3 fatty acids has an enhanced anti-inflammatory effect on microglia. Neurochem. Int. 2016, 99, 206–214. [Google Scholar] [CrossRef]
- Guest, D.D.; Evans, E.M.; Rogers, L.Q. Diet components associated with perceived fatigue in breast cancer survivors. Eur. J. Cancer Care 2013, 22, 51–59. [Google Scholar] [CrossRef]
- Lowry, E.; Marley, J.; McVeigh, J.G.; McSorley, E.; Allsopp, P.; Kerr, D. Dietary Interventions in the Management of Fibromyalgia: A Systematic Review and Best-Evidence Synthesis. Nutrients 2020, 12, 2664. [Google Scholar] [CrossRef]
- Zuniga, K.E.; Parma, D.L.; Muñoz, E.; Spaniol, M.; Wargovich, M.; Ramirez, A.G. Dietary intervention among breast cancer survivors increased adherence to a Mediterranean-style, anti-inflammatory dietary pattern: The Rx for Better Breast Health Randomized Controlled Trial. Breast Cancer Res. Treat. 2019, 173, 145–154. [Google Scholar] [CrossRef] [PubMed]
- Esposito, K.; Marfella, R.; Ciotola, M.; Di Palo, C.; Giugliano, F.; Giugliano, G.; D’Armiento, M.; D’Andrea, F.; Giugliano, D. Effect of a Mediterranean-style diet on endothelial dysfunction and markers of vascular inflammation in the metabolic syndrome: A randomized trial. JAMA 2004, 292, 1440–1446. [Google Scholar] [CrossRef] [PubMed]
- George, S.M.; Neuhouser, M.L.; Mayne, S.T.; Irwin, M.L.; Albanes, D.; Gail, M.H.; Alfano, C.M.; Bernstein, L.; McTiernan, A.; Reedy, J. Postdiagnosis diet quality is inversely related to a biomarker of inflammation among breast cancer survivors. Cancer Epidemiol. Prev. Biomark. 2010, 19, 2220–2228. [Google Scholar] [CrossRef] [PubMed]
- Orchard, T.S.; Andridge, R.R.; Yee, L.D.; Lustberg, M.B. Diet quality, inflammation, and quality of life in breast cancer survivors: A cross-sectional analysis of pilot study data. J. Acad. Nutr. Diet. 2018, 118, 578–588.e1. [Google Scholar] [CrossRef]
- Nashed, M.G.; Balenko, M.D.; Singh, G. Cancer-induced oxidative stress and pain. Current Pain Headache Reports 2014, 18, 384. [Google Scholar] [CrossRef]
- Shim, H.S.; Bae, C.; Wang, J.; Lee, K.-H.; Hankerd, K.M.; Kim, H.K.; Chung, J.M.; La, J.-H. Peripheral and central oxidative stress in chemotherapy-induced neuropathic pain. Mol. Pain 2019, 15, 1744806919840098. [Google Scholar] [CrossRef]
- Luo, Y.; Ma, J.; Lu, W. The Significance of Mitochondrial Dysfunction in Cancer. Int. J. Mol. Sci. 2020, 21, 5598. [Google Scholar] [CrossRef]
- Doyle, T.M.; Salvemini, D. Mini-Review: Mitochondrial dysfunction and chemotherapy-induced neuropathic pain. Neurosci. Lett. 2021, 760, 136087. [Google Scholar] [CrossRef]
- Totsch, S.K.; Waite, M.E.; Sorge, R.E. Dietary influence on pain via the immune system. Prog. Mol. Biol. Transl. Sci. 2015, 131, 435–469. [Google Scholar]
- Skouroliakou, M.; Grosomanidis, D.; Massara, P.; Kostara, C.; Papandreou, P.; Ntountaniotis, D.; Xepapadakis, G. Serum antioxidant capacity, biochemical profile and body composition of breast cancer survivors in a randomized Mediterranean dietary intervention study. Eur. J. Nutr. 2018, 57, 2133–2145. [Google Scholar] [CrossRef] [PubMed]
- Butalla, A.C.; Crane, T.E.; Patil, B.; Wertheim, B.C.; Thompson, P.; Thomson, C.A. Effects of a Carrot Juice Intervention on Plasma Carotenoids, Oxidative Stress, and Inflammation in Overweight Breast Cancer Survivors. Nutr. Cancer 2012, 64, 331–341. [Google Scholar] [CrossRef] [PubMed]
- Schatz, A.A.; Oliver, T.K.; Swarm, R.A.; Paice, J.A.; Darbari, D.S.; Dowell, D.; Meghani, S.H.; Winckworth-Prejsnar, K.; Bruera, E.; Plovnick, R.M.; et al. Bridging the Gap Among Clinical Practice Guidelines for Pain Management in Cancer and Sickle Cell Disease. J. Natl. Compr. Cancer Netw. 2020, 18, 392–399. [Google Scholar] [CrossRef]
- Hartung, J.E.; Eskew, O.; Wong, T.; Tchivileva, I.E.; Oladosu, F.A.; O’Buckley, S.C.; Nackley, A.G. Nuclear factor-kappa B regulates pain and COMT expression in a rodent model of inflammation. Brain Behav. Immun. 2015, 50, 196–202. [Google Scholar] [CrossRef] [PubMed]
- Kolberg, M.; Pedersen, S.; Bastani, N.E.; Carlsen, H.; Blomhoff, R.; Paur, I. Tomato paste alters NF-κB and cancer-related mRNA expression in prostate cancer cells, xenografts, and xenograft microenvironment. Nutr. Cancer 2015, 67, 305–315. [Google Scholar] [CrossRef] [PubMed]
- Pellegrini, M.; Ippolito, M.; Monge, T.; Violi, R.; Cappello, P.; Ferrocino, I.; Cocolin, L.S.; De Francesco, A.; Bo, S.; Finocchiaro, C. Gut microbiota composition after diet and probiotics in overweight breast cancer survivors: A randomized open-label pilot intervention trial. Nutrition 2020, 74, 110749.
- Croisier, E.; Brown, T.; Bauer, J. The Efficacy of Dietary Fiber in Managing Gastrointestinal Toxicity Symptoms in Patients with Gynecologic Cancers undergoing Pelvic Radiotherapy: A Systematic Review. J. Acad. Nutr. Diet. 2021, 121, 261–277.e2.
- Lynch, S.V.; Pedersen, O. The Human Intestinal Microbiome in Health and Disease. N. Engl. J. Med. 2016, 375, 2369–2379.
- Guida, F.; Boccella, S.; Belardo, C.; Iannotta, M.; Piscitelli, F.; De Filippis, F.; Paino, S.; Ricciardi, F.; Siniscalco, D.; Marabese, I. Altered gut microbiota and endocannabinoid system tone in vitamin D deficiency-mediated chronic pain. Brain Behav. Immun. 2020, 85, 128–141.
- Dalile, B.; Van Oudenhove, L.; Vervliet, B.; Verbeke, K. The role of short-chain fatty acids in microbiota–gut–brain communication. Nat. Rev. Gastroenterol. Hepatol. 2019, 16, 461–478.
- Guo, R.; Chen, L.-H.; Xing, C.; Liu, T. Pain regulation by gut microbiota: Molecular mechanisms and therapeutic potential. Br. J. Anaesth. 2019, 123, 637–654.
