Fetal acidosis is one of the main concerns during labor. Currently, fetal blood sampling (FBS) has become the most accurate measurement of acidosis detection. However, it is invasive and does not provide a real time measurement due to laboratory procedures.
1. Introduction
Fetal blood sampling (FBS) is a well-established technique for monitoring fetal acidosis with high precision. However, due to its invasive nature, bleeding and infection are the primary concerns [1,2]. Several non-invasive techniques such as a Doppler ultrasound, tocodynamometer, cardiotocogram, fetal pulse oximetry, and fetal electrocardiograph have been suggested to address these concerns. However, the low accuracy and precision of these methods result in faulty analysis, impairing decision-making, as evidenced by the rising number of unnecessary C-sections in recent years [3,4]. Current non-invasive techniques are insufficient and require significant design enhancements to meet standard requirements. Additionally, alternative methods for providing minimally invasive and more continuous monitoring devices should be explored to fulfill the clinical needs of intrapartum fetal monitoring [1].
2. Fetal Acidosis
Intrapartum or the transition period of labor is part of birth stress in which the fetus is compromised, receiving insufficient oxygen supply from placental circulation. It may create an extreme condition to the fetus either gradually or suddenly during the transition from maternal–fetal umbilical respiratory gas exchange to fetal lung activation [
5]. Fetal acidosis or intrauterine hypoxia refers to a condition of deprived short supply of oxygen below the physiologic level of normal blood, which is defined as pH ≤ 7.25 [
1,
6,
7].
Table 1. pH measurement for acidosis [
1].
| Measurands |
Interpretation |
| pH |
Lactate |
|
| ≥7.25 |
≤4.1 mmol/L |
Normal |
| 7.21–7.24 |
4.2–4.8 mmol/L |
Borderline |
| ≤7.20 |
≥4.9 mmol/L |
Abnormal |
Deviation in systemic acidity requires physiological adaptations in the redistribution of blood flow to vital organs, most notably the heart and brain [
5]. This can have a detrimental effect if fetal distress goes unmanaged, resulting in critical organ failure, particularly cerebral damage. Specifically, hypoxic–ischemic encephalopathy (HIE), cerebral palsy (loss of motor function; damage of white matter due to reduced blood or oxygen supply known as periventricular leukomalacia (PVL), which can be fatal when severe [
7,
11,
12]. According to a previous study, out of 56574 babies born at 35 gestation weeks or more, 506 of them have pH ≤ 7 which is 0.9%, with three deaths occurring within an hour of birth and a total of 24 deaths before the age of 2 years [
12].
Apart from pH, a few other parameters have been observed to change significantly during acidosis. In study [
10], it was noticed that pO2, pH and bicarbonate concentrations decreased, whereas lactate and potassium concentrations increased. However, pO2 was the parameter that most quickly reflected changes in the acid-base status, reaching its minimum value within 2.38 min. It was followed by pH, which indicates the severity of an acidosis. Other metabolites (bicarbonate, potassium and lactate) exhibit a gradual change in response to the cellular metabolism, which induced a decrease in oxygen levels in the blood. Thus, pO2 becomes the predominant parameter for the onset of acidosis where pO2 ≤ 80 mmHg or SpO2 ≤ 95%. In addition, pO2 was the only metabolite capable of reaching a similar level in the basal period.
2.2. Current Fetal Acidosis Detection Method
Fetal acidosis is the most undesirable condition during labor; thus, monitoring is necessary in order to examine the health of the fetus by either an invasive or non-invasive method.
2.2.1. Invasive Method
Electronic Fetal Monitoring (EFM), developed in the 1950s, introduced the cardiotocogram (CTG), which records the fetal heart rate and measures contraction frequency. The duration and strength of uterine contractions are related to the fetal heart rate (FHR) and its pattern. CTG consists of external devices (Doppler ultrasound and tocodynamometer), internal devices (intrauterine pressure catheters (IUPC) and fetal scalp electrodes (FSE)) [
13]. A Doppler ultrasound provides an audible simulation of the fetal heartbeats, and the real-time audio sound is shared with everyone present in the room. Since the tocodynamometer provides an unreliable measure of contraction strength, it was replaced by IUPC with the evolution of the catheter-tip sensor. Nonetheless, this method is invasive in nature, and requires membrane rupture, which is one of the IUPC’s drawbacks [
14]. CTG is very sensitive but not particularly specific, which means that a suspicious CTG signal can appear in the absence of any abnormality. As a result, it is necessary to increase the specificity, which is accomplished through pH.
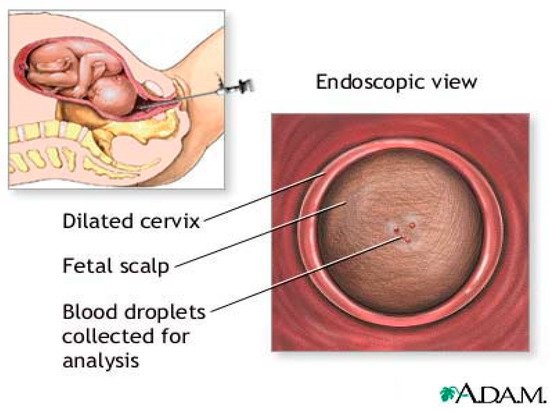
In 1961, Hon introduced Fetal Blood Sampling (FBS) [
3] as shown in
Figure 1. It has long been recognized as the most accurate test for measurement of pH,
pCO2and base access. FBS is considered after CTG is pathological and considers expediting the birth [
15]. FBS requires cervical dilation of 3–4 cm to accommodate a large amnioscope [
3]. It is followed by a small scalpel incision to a depth of 1.5–2 mm [
15] to obtain a blood sample using a thin heparinized capillary tube and transportation to the laboratory for analysis. Reduced blood pH serves as an early warning sign of acidosis, which is important for the obstetrician [
16]. If the blood sample results are borderline (pH 7.1–7.24), a follow-up sample should be taken 30 min later, while birth should be expedited in cases of pH ≤ 7.20 [
17].
Figure 1. Fetal blood sampling. “Adapted with permission from Ref. [
18], 2022, Jacobson, J.D.; Zieve, D.”.
The condition that ruptures fetal scalp membranes induces risk to mother and child in terms of tissue reactions, pain, bleeding, and infection. These risks are increased in fetuses with suspected hemophilia or thrombocytopenia [
15] and in mothers with HIV, hepatitis B, or C [
3]. In addition, the analysis requires a large amount of blood (30–50 uL) and is time consuming (median time taken is 18 min) [
19], resulting in diagnostic delay while pH drops at a rate 0.01–0.04 unit/min [
20,
21]. Prolonged collection time increases the risk of blood clotting and clogging the analyzer [
22]. Due to the liquid nature of the blood sample, it is easily contaminated by amniotic fluid, meconium, and other fluids that may enter the blood sample and affect the pH measurements [
23].
FBS is currently available in two forms of measurement, which are pH and lactate. Lactate measurements have an advantage in terms of analysis because they require a smaller amount of blood (5 μL) compared to pH analysis (30–50 μL) [
22]. FBS has shown to be capable of detecting fetal acidosis in up to 10% of cases where ST events were absent on ECG or CTG [
2]. FBS also revealed that only 11% of fetuses with suspicious FHR had acidosis, defined by Saling as a scalp pH < 7.20. These findings suggest that FBS could reduce the number of cesarean sections associated with the use of continuous CTG [
3].
2.2.2. Non-Invasive Method
There are a few non-invasive fetal monitoring techniques, which are discussed below.
The fetoscope, invented by David Hillis in 1917, was the first non-invasive method for monitoring fetal development. It is an intermittent auscultation (IA) technique used during labor to monitor the fetal heart rate (FHR). IA is the best way to monitor healthy women with healthy pregnancies at a low risk of complications [
24]. However, it was not a reliable indicator of fetal distress other than in an extreme situation of terminal bradycardia [
25].
Fetal Pulse Oximetry (PO) is a technique for determining the saturation level of fetal blood oxygen (SpO2
) based on the relative absorbance of multiple light wavelengths by oxyhemoglobin and deoxyhemoglobin, which produces a periodic time domain signal called a photoplethysmogram (PPG). PPG pulse depth at two wavelengths is used to estimate the relative concentration of
HbO2
in pulsating arterial tissue. Conventional invasive PO is performed using a probe placed on the fetus’ head while it is in the uterus and vaginal canal during labor [
26,
27]. However, transabdominal PO available today have apply near-infrared light transmitted to the maternal abdomen and fetus in order to measure the oxygen saturation in the fetal blood non-invasively [
27].
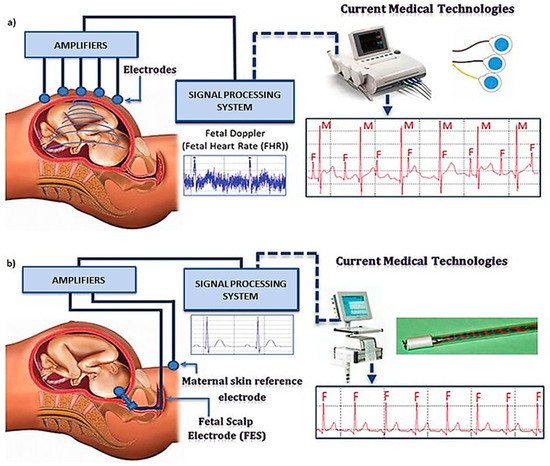
The fetal electrocardiograph (fECG) is a graphic record of the electrical activity of myocardial cells that reflects the oxygenation level of the myocardium, as shown in Figure 2.
Figure 2. fECG placement and the working principle (
a) external electrode (
b) internal electrode. “Adapted with permission from Ref. [
28], 2012, Martinek, R.; Žídek, J.”.
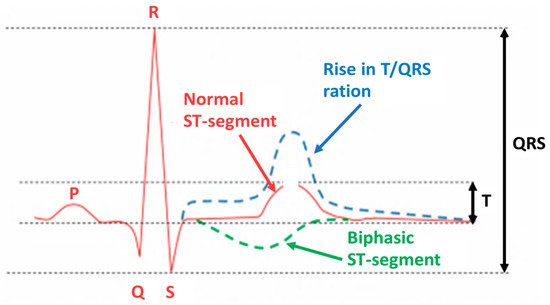
The fECG classification system incorporates a ST analysis (STAN) algorithm for interpretation. It evaluates changes in the fECG complex (
Figure 3), most notably the ST segment and T wave [
29,
30]. Additionally, the T/QRS ratio is analyzed, which indicates the duration of the hypoxic insult in the cells [
29] and correlates to the severity of myocardial damage. ECG bradycardia develops immediately as a result of hypoxia and the resulting acidosis. Bradycardia is a critical time marker for delivery, as any delay in delivery greater than 18 min from uterine rupture results in significant morbidity. The ECG should be used in conjunction with other evaluation tools, such as echocardiography and biochemical markers [
5].
Figure 3. Fetal ECG in acidosis occurrence. “Adapted with permission from Ref. [
28], 2012, Martinek, R.; Žídek, J.”.
Electro myometrial imaging (EMMI) evaluates three-dimensional (3D) uterine electrical activation in detail and visualizes uterine contractions in 3D with high spatial and temporal resolution. EMMI originates from magnetic resonance images of body surface electrical recording combined with body–uterus geometry. EMMI is a technique that utilizes electrodes placed on the abdomen to reconstruct the uterine electrical activation patterns and thus generates CTG. These patterns correspond to those obtained when electrodes are placed directly on the uterine surface [
31].
The development of non-invasive methods is an excellent alternative for fetal monitoring, since invasive methods suffer limitations such as bleeding, tissue biocompatibility, and trauma to the fetus and mother. Non-invasive methods could eliminate those adverse effects before irreversible damage to the fetus occurs, thereby lowering mortality and morbidity rates. However, accurate reading is the main constraint. This motivates researchers from several disciplines to develop high precision fetal monitoring devices that employ a variety of techniques.
This entry is adapted from the peer-reviewed paper 10.3390/s22041334