1. Social Isolation during COVID-19: Health Consequences
Quarantine is a viable tool for combating the spread of COVID-19
[1]; however, its sequela, social isolation, particularly when prolonged, increases the risk of infringing on many individuals’ needs for social interactions. Maslow’s Motivational Theory of Needs (1943) first outlined a hierarchy of human needs, which Matias et al. have adapted slightly and incorporated into the current landscape of quarantine
[2]. Using a physiological and psychological perspective, they outlined how each level of “need” is specifically impacted by quarantine, resulting in a disbalance of body equilibrium
[2]. The resulting behaviours are our innate drive to bring our body back into balance, and, as such, their outline will be discussed as a framework herein
[2]. In keeping with this view, when our body is in disbalance due to unmet needs, certain acute health consequences result, as listed in
Table 1.
Table 1. Physiological and psychological health issues associated with social isolation. It is important to note that many of the factors mentioned are often comorbid and associated with one another and that these consequences are health risks for “secondary” conditions (e.g., alcohol consumption is a risk factor for depression
[3]).
| Physiological Changes |
Psychological Changes |
| Body System |
Symptom/Change |
|
| Neuropsychology System |
- -
-
|
- -
-
General mental well-being deterioration [5]
|
- -
-
Psychomotor excitement [4]
|
- -
-
Increased alcohol consumption [5][2]
|
| Neuromuscular System |
- -
-
Loss of muscle mass (due to sedentarism) [6]
|
- -
-
|
- -
-
Muscle damage/denervation to neuromuscular joints [6]
|
- -
-
Generalized anxiety [5][2][4][7][8]
|
| Muscle Protein Metabolism |
- -
-
Increased risk of poor metabolic health, functional decline, and all-cause mortality [6]
|
- -
-
Depression [5][2][4][7][8]
|
- -
-
Suppression of muscle protein synthesis [6]
|
- -
-
|
| Glucose Homeostasis |
- -
-
Skeletal muscle has a pivotal role in inactivity-induced insulin resistance [6]
|
- -
-
|
- -
-
Specific reduction in muscle insulin sensitivity (without affecting that of the liver)
|
- -
-
|
- -
-
Insulin resistance (change in insulin sensitivity leads to muscle atrophy and change in body composition) [6]
|
- -
-
Symptoms of post-traumatic stress disorder (PTSD) [7]
|
| Cardiorespiratory System |
- -
-
Reduced cardiorespiratory fitness [6]
|
- -
-
|
- -
-
Various steps of the oxygen pathway are impaired (e.g., central and peripheral cardiovascular function to skeletal muscle oxidative metabolism) [6]
|
- -
-
|
- -
-
Lower/decrease in VO2max (associated with increased mortality) [6]
|
- -
-
|
| Digestive System/Energy Balance |
- -
-
Overfeeding/comfort eating leads to systemic inflammation, weight gain, obesity, eating disorders, and muscle loss [2][6]
|
- -
-
Psychological conflict [9]
|
- -
-
Bed rest/home isolation may be associated to decreased energy intake and rapid muscle wasting [6]
|
- -
-
|
The foundation level of this hierarchical structure is “Immediate Physiological Needs” (i.e., hunger, thirst, sex, elimination, sleep), which were the first to be affected by the COVID-19 pandemic
[2]. Stress and anxiety caused by the ‘lockdown’ responses have created psychological conflict in individuals, where they panic buy and stockpile supplies, incidentally affecting two foundational physiological needs—food and drink. While these behaviours are undertaken in order to provide comfort through food and drink, the consequences include weight gain, obesity, and eating disorders
[9][2]. Sleep is another basic foundational physiological need that is disturbed during conditions of isolation produced by the pandemic
[10]. As sleep is vital for healthy body maintenance and repair, the reduction in sleep quality and/or quantity places individuals at risk for physiological deterioration and attenuated immune function
[11]. Furthermore, along with its negative impact on sleep, the increased propensity toward a sedentary lifestyle has a number of physiological effects on cardiovascular, metabolic, and endocrine systems, creating further health implications (
Table 1)
[6].
The “Need for Self-Protection” is the next level of basic human needs affected by the stay-at-home government policies
[2]. The fear of infection and death along with unmet self protection needs among result in deep-rooted feelings in individuals in lockdown of not being able to protect themselves or their family
[2]. The resulting frustration contributes to adverse health outcomes and behaviours when the need for self-protection is unmet in isolated conditions (
Table 1). Recent data have demonstrated various health consequences in vulnerable individuals during COVID-19 lockdowns—conditions such as an increase in alcohol consumption (hazardous drinking increased to 29.1%, harmful drinking to 9.5%), deterioration of mental well-being (32.1% reported), various forms of anxiety (29% reported), different forms of depression (37.1% reported), and increased risk of suicide
[5][12][13]. Furthermore, these factors are found to result in insomnia, irritability, and aggression (e.g., physical violence)
[5][2], which is evinced by the increase in homicides and suicides during the current pandemic
[2][14]. While these factors refer to individual consequences, lockdown policies result in groups of individuals spending prolonged periods of time together (e.g., roommates, families), creating unique and abnormal periods of interaction. This highlights that there are not only health implications at the individual level but at a family-dynamic level as well.
The next affected need is the “Need for Affiliation”
[2]. Connecting with others is a natural need that helps an individual deal with controlling emotions, coping with stress and remaining resilient; however, quarantine policies limit this much-needed face-to-face contact. While virtual options exist, they are missing nonverbal cues, lack warmth and provide less engagement, resulting in a reduced quality of connection
[15]. As a result, social isolation and loneliness increase any existing stress, which can have harmful effects on immune and cardiovascular health
[2][6]. These effects include deterioration in various body functions, ranging from the neuromuscular system to energy balance and inflammation, as depicted in
Table 1. Importantly, individuals who feel unfulfilled in their need for affiliation are at greater risk of failing to meet the next level of need.
The last need affected by isolation is the “Need for Status/Self-Esteem”. The pandemic has caused increased unemployment and poverty, which are related to decreased self-esteem in affected individuals
[2]. This outcome leads to an increased vulnerability to depressive symptoms and an increase in alcohol consumption
[2]. The previously mentioned data by Ahmed et al. suggests that 37.1% of participants affected by the pandemic-lockdown experience depressive symptomatology, and hazardous drinking has increased to 29.1%, with 32.1% of participants experiencing a decline in mental health
[5].
The foregoing health concerns associated with social isolation provide an important emphasis on the inciting factors that place individuals at risk of these outcomes. Numerous stressors have been found to be associated with these social isolation outcomes, including, but not limited to, longer quarantine duration, fear of being infected, frustration, boredom, inadequate supplies, inadequate information, financial loss, and stigma associated with the illness
[7]. Addressing these stressors will directly help reduce any possible health outcomes associated with social isolation and indirectly treat any behaviour/consequence related to those outcomes (e.g., alcoholism, depression, loneliness, anxiety).
As these social isolation health risks are becoming more apparent, recent studies have identified a number of vulnerable subgroups in the general population. The elderly have been identified as being more likely to suffer psychologically; however, it is suggested that this is due to the high mortality rate in this clinical population amidst the pandemic (i.e., the perception of an active threat and particular vulnerability incites mental stress)
[16][9]. Furthermore, elders were found to have depressive symptomatology due to a lack of informational technology (I.T.) skills (i.e., inability to connect with others)
[8]. Interestingly, elders were found to be less likely to socially isolate even thought they were at the greatest risk, which the authors concluded was due to the psychological conflict of wanting to maintain a normal lifestyle
[16][9]. Nonetheless, elders are still vulnerable to social isolation risk as they are forced to adhere to quarantine guidelines (i.e., those that adhere to isolation guidelines are therefore at risk, and those that choose not to adhere to quarantine guidelines are limited in their social interactions due to the current quarantine policies). Online questionnaires found that the younger age group (ages 21–40 years) and women were more vulnerable to mental health issues, as their stress increase was associated with social media usage (i.e., more access to the oversaturation of COVID-19 related news)
[16][17][18]. Social isolation is generally associated with physical inactivity, and as such, younger people are vulnerable to loneliness due to the association of physical inactivity with loneliness (e.g., adolescents being physically inactive were more likely to feel lonely)
[19]. It is important to understand these physical/mental health consequences, the stressors, and groups vulnerable to the effects of social isolation, as it informs us as to how anxiety is associated with the current COVID-19 solution.
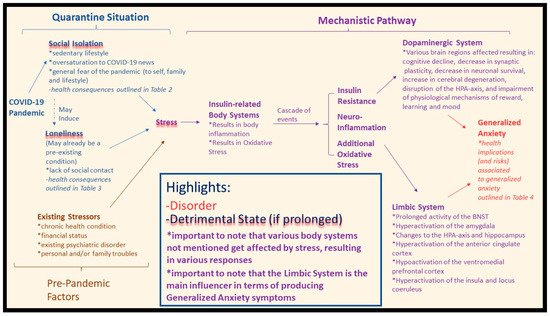
Figure 1 depicts a construct in which straining conditions, such as social isolation, are associated with symptoms of anxiety during the COVID-19 pandemic.
Figure 1. General proposed pathway influenced by various factors. Physiological concepts are applied to formulate the pathway. The proposed mechanism where the COVID-19 pandemic has caused quarantine response: social isolation conditions have a number of health issues associated with stress (highlighted in blue). Loneliness may be induced by social isolation, or make an existing loneliness condition worse, and is also associated with stress (highlighted in blue). Pre-pandemic factors also play a role (highlighted in brown). The resulting stress is associated with a cascade of events (highlighted in purple), ending with a link to generalized anxiety.
2. Loneliness during COVID-19: Health Concerns
It is proposed that the increase in physiological stress response (e.g., increased levels of cortisol) due to the COVID-19 pandemic results in an overall abnormal stress response that negatively affects health outcomes
[20]. For example, social isolation has been linked to the subjective experience of loneliness, which has been reported to have a significant impact on mental and physical health, resulting in adverse overall health outcomes, as outlined in
Table 2 [21][20][22].
Table 2. Physiological and psychological health issues associated with loneliness. It is important to note that many of the issues mentioned are comorbid and associated with “secondary” conditions.
| Physical Health Consequences/Risks |
Mental Health Consequences/Risks |
- -
-
Increased systolic blood pressure [20]
|
- -
-
Reduced time in bed spent asleep (7% less) (and overall sleep quality) [20][23][24]
|
- -
-
Increased risk of heart disease [20][22][25]
|
- -
-
Increased wake time after sleep onset [20][23]
|
- -
-
Increased risk of stroke [22][25]
|
- -
-
Increase in depressive symptomology [24][26]
|
- -
-
|
- -
-
Poor self-related health [26]
|
- -
-
Reduced quality of life (applies to both physical and mental aspects) [27]
|
- -
-
Impaired functional status/cognition [20][24][26]
|
- -
-
Disability (applies to both physical and mental aspects) [24][28][29]
|
- -
-
Perceived negative change in the quality of one’s life [24][26]
|
- -
-
|
- -
-
Suicide attempts/completed suicides (among older adults) [30]
|
- -
-
Increased mortality [24][31][32]
|
- -
-
|
- -
-
Increased use of healthcare services [24][36][37][38]
|
- -
-
Institutionalization [39]
|
As discussed in a recent manuscript by Wilkialis et al.
[40], loneliness is concerning as it is associated with a number of adverse health outcomes, including, but not limited to, GAD, major depressive disorder, suicide, and increased mortality
[21][41][42]. Furthermore, loneliness was highly prevalent before the COVID-19 pandemic
[21][35]. We theorize that the current COVID-19 pandemic and the implementation of quarantine as a public health strategy to prevent its spread is increasing the rate of loneliness. Notably, the elderly are identified as a population more vulnerable to loneliness due to their increased susceptibility to the virus and subsequent need to quarantine to minimize the spread of COVID-19
[43][22][44]. Taking this into consideration, the relationship between the COVID-19 pandemic alongside the rate and severity of loneliness is increasing, especially in people previously or currently infected, with elders being disproportionately affected
[45][46]. We therefore conclude that with the implementation of social isolation (i.e., quarantine) the rate of subjective experiences of loneliness are also increasing.
Loneliness is associated with various health impacts, and it is important to highlight possible variables that place individuals at increased risk to adverse health outcomes. In addition to social isolation, there are a number of risk factors for loneliness. For example, living in a rural area, poor functional status (especially cognitive impairment), widowhood, being female, subjective causes (illness, death, etc.), depression, feeling misunderstood by others, and living alone (quarantine/social isolation for our purposes)
[24]. Indeed, a recent study reported similar risk factors associated with high rates of loneliness during the COVID-19 pandemic: being female, being younger, having fewer family resources (less contact with relatives), having fewer personal resources, and having a negative self-perception of aging
[47]. The main concern is that because of the current COVID-19 pandemic, loneliness is becoming an increasing and/or worsening problem
[20]; this will have many acute and long term effects on individuals and may lead to other illnesses that have already been associated with loneliness (e.g., GAD)
[21][48].
3. Social Isolation, Loneliness, and Generalized Anxiety during COVID-19
Taken together, the implication of both social isolation and loneliness allows us to highlight their differences and distinct negative outcomes on both physical and mental health. Nonetheless, it is important to acknowledge that both conditions have been intertwined, with their various health implications being comorbid
[33][49][50]. The foregoing observations, along with research suggesting that social isolation, because of the pandemic, has led to increased loneliness
[45][46], provide the impetus to analyze their combined effects on both physical and mental health. These combined effects consist of a wide array of risk factors that have both a direct and indirect association to GAD, as outlined in
Table 3. Recent online studies show evidence supporting this association by confirming the increase in self-reported symptoms of anxiety and psychological distress during the COVID-19 pandemic lockdown
[5][51][52][53][54].
Table 3. Social isolation and loneliness health implications (and risk factors) associated with generalized anxiety during the COVID-19 quarantine.
| Direct |
Indirect |
- -
-
|
- -
-
Alcohol consumption [5][2]
|
- -
-
|
- -
-
|
- -
-
|
- -
-
|
- -
-
|
- -
-
|
- -
-
|
- -
-
COVID-19/mortality fear [47][16][2][8][55]
|
- -
-
Higher all-cause mortality (both independent risk factors) [20]
|
- -
-
Running out of life-sustaining medical supplies/care/access [51][16][8][20]
|
- -
-
|
- -
-
Oversaturation to COVID-19 news (via radio, TV, social media) [47][16][8]
|
- -
-
Low self-perceived health condition [51]
|
- -
-
Increased risk of coronary artery disease-associated death (even with no prior history) [20]
|
- -
-
Unemployment/economic loss [51][22][56]
|
- -
-
Cardiovascular disease [22]
|
- -
-
Previous psychiatric history (recurrent or induced) [53][20]
|
- -
-
Chronic health illnesses [53]
|
The independent health implications of social isolation and loneliness (
Table 1 and
Table 2) also play a role in the increased rate of anxiety, which is discussed herein. In terms of gender, the literature suggests that males are more prone to alcohol consumption during quarantine
[5] and women are more prone to stress and higher levels of generalized anxiety pertaining to their overall health
[53][16]. Elderly populations are especially vulnerable to the pandemic due to the loneliness and social isolation conditions, in which exposure to the radio, TV, and media can increase fear, generalized anxiety, and depression
[16][8]. Those already suffering from loneliness and social isolation are even more affected
[20]. Additional important findings to note are that people with higher education (more self aware of their health)
[16], people with previous or current psychiatric illness
[53][57], existing chronic illness
[53], current COVID-19 patients
[58] and those living in urban areas
[53] are also found to be more vulnerable to the associated mental health consequences of the pandemic. We therefore theorize that these foregoing factors and their resulting effects are directly and indirectly associated with GAD. Understanding these effects, particularly in vulnerable groups, will further help elucidate the association of social isolation and loneliness with GAD during the COVID-19 pandemic.
Mounting data suggests that individuals are more prone to symptoms of generalized anxiety during the COVID-19 quarantine; increasing rates during quarantine conditions are expected, as well as more cases post pandemic. Furthermore, symptoms of generalized anxiety are associated with a number of health morbidities due to its comorbid nature, including, but not limited to, depressive disorders, substance abuse disorders, mood disorders, somatic symptom disorder, heart disease, chronic respiratory disorder and gastrointestinal conditions
[59][60]. When taking these into account with the implications of GAD, social isolation, and loneliness, there is a mixture of health hazards for affected individuals. These hazards will result in acute and chronic morbidities, leading to possible premature death. To acknowledge and address this, it was noteworthy to begin by outlining the independent and combined health consequences of social isolation and loneliness and their possible association with GAD.