Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Biotechnology & Applied Microbiology
CD146, also known as MUC18 or MCAM, is a 113KDa transmembrane glycoprotein that was first described by Johnson et al. as a melanoma progression antigen. It was found to be present in the vascular system, whatever the caliber of the vessel, in endothelial cells, smooth muscle cells and pericytes. In normal cells, CD146 is also expressed by placental trophoblasts and a subset of activated T-cell.
Triple Negative Breast Cancers (TNBC) are the most aggressive breast cancers and lead to poor prognoses.
- CD146
- triple negative breast cancer
- treatment
1. Introduction
CD146 has been shown to be expressed not only in melanoma but also in various cancers, such as pancreatic [1], breast [2], prostate [3], ovarian [4], hepato-carcinoma [5] and kidney [6] cancers. Its expression is generally associated with a poor prognosis for the patient. In breast cancer, CD146 induces the epithelial-to-mesenchymal transition (EMT), a crucial process in cancer metastasis [7], gaining stem cell-like properties [8] and generating cells known as Cancer Stem Cells (CSC).
Despite CD146 having been stated to be a tumor suppressor in breast cancer in certain studies, it is noteworthy that up-modulation of CD146 is frequently related to various high-grade tumors, ER-PR negative tumors and also triple negative breast cancers (TNBC) [9]. Subsequently, its down-regulation was frequently shown to induce a less aggressive phenotype tumor [10].
Of interest, CD146 appears to be highly expressed in TNBC [11] and could thus constitute a novel target in this type of breast cancer for which efficient therapeutic approaches are currently lacking. However, CD146 is also vital for vascular development and functions [12]. It thus appears difficult to target tumor CD146 without affecting vascular functions.
2. Soluble CD146 as a Potential Target for Preventing Triple Negative Breast Cancer MDA-MB-231 Cell Growth and Dissemination
Among breast cancers, Triple Negative Breast Cancer (TNBC) is one of the most aggressive [9] with few therapeutic options. This entry emphasized the role of CD146 and, in particular, its soluble form in TNBC development. Interestingly, the administration of M2J-1 mAb, which specifically targets the soluble form of CD146, led to a decrease in tumor size and metastatic dissemination and could represent a new therapeutic approach.
CD146 is considered as a major factor involved in tumor growth and dissemination. In-vivo studies have shown that its over expression leads to an increased metastatic ability of cancer cells [13]. Thus, it has been shown to increase the metastasis of lymphoma cells in a chicken model [14] and of mouse mammary carcinoma cells [15]. Wu et al. also showed that the over-expression of CD146 in prostate cancer [16] led to an increase in metastasis in-vivo [3]. CD146 has been reported to be responsible for advanced tumor stages and constitutes a poor prognosis factor for tumor relapse in ovarian cancer [17].
Likewise, CD146 expression is linked to a poor survival rate in pulmonary adenocarcinoma [18]. In non-small lung cancer (NSCLC) patients, CD146 expression was found to be gender specific, and its over expression leads to a poor survival rate [19]. In NSCLC, females had higher CD146 expression than males, proving it to be the poor prognostic factor for lung adenocarcinoma [20]. Finally, Peng Zeng et al. conducted a meta-analysis and showed a correlation between higher CD146 expression and poor survival rate of patients, thus, making it a valuable prognostic marker for many solid tumors [21].
In contrast to many other cancers, studies related to the correlation between CD146 and breast cancer are few and highly controversial. While some studies have shown that CD146 acts as a tumor suppressor in breast cancer because of its high expression on benign proliferative lesions and low expression on breast carcinoma [22], other studies have demonstrated a positive association between CD146 expression and breast cancer and a major role of the molecule in cell motility and invasion [10].
CD146 is highly expressed in TNBC [11] and is reported as a main activator of the Epithelial to Mesenchymal Transition (EMT), which constitutes an important process responsible for high metastatic features. Indeed, when over-expressed in epithelial breast cancer cells, CD146 down-regulates the epithelial markers while it up-regulates the mesenchymal markers, which significantly results in an increased cell migration and invasion ability along with an increase in Cancer Stem Cell (CSC) properties [9][10]. In addition, it has been proposed that CD146 may serve as a novel therapeutic target to overcome chemoresistance [23].
CD146 expression has been shown to be correlated with sCD146 secretion in many tumor cells [24], and sCD146 constitutes a major actor of tumor growth and dissemination [25]. This entry evidenced the effect of sCD146 on the expression of CSC markers, a phenomenon that has been frequently associated to their resistance to various treatment therapies like radiation, chemotherapy and hormonal therapy [26]. The breast cancer cell line MDA-MB-231 was used as a model in this study as it was found to have high CD146 expression.
The cells were found to have high CD44, low CD24, high EPcam and high CD133 expression, a characteristic of breast CSC. In addition, it was identified that two populations of CSC with different CD146 expression, namely CD146-high and CD146-low populations as already observed by Mostert et al. [27]. It were able to sort these two populations of cells for either studying their phenotype or re-culturing them to analyze whether they were able to maintain their phenotypical characteristics.
It was demonstrated that, immediately after sorting, CD146-high cells displayed a higher CD44/CD24 ratio and a higher expression of EPcam compared CD146-low cells, in favor of a more pronounced stemness phenotype. In addition, when re-cultured after sorting, CD146-high cells maintained their CD146-high expression while CD146-low cells differentiated into CD146-high and CD146-low cells. Added to the fact that CD146-high cells are the most important population in MDA-MB-231 cells, these results are in favor of the fact that high expression of CD146 constitutes an advantageous phenotype for cells to grow.
Along this line, the sorted cell populations of CD146-high and CD146-low cells showed that high CD146 expression was correlated with a higher proliferation, migration and invasion capacity. Of interest, soluble CD146 was able to reproduce these effects and it was able to increase many CSC and EMT markers expressed by the CD146-high cells.
These results will have to be confirmed in other TNBC cell lines expressing high levels of CD146, such as SUM159PT, SUM1315MO2 or SUM149PT cells [27]. In order to compare our results to the literature, it used public databases to estimate the influence of CD146 expression on properties of breast cancer cells and overall survival of patients. Figure 1A shows that CD146 expression is significantly higher in TNBC compared with in other breast cancers, such as HER2 or luminal breast cancers.
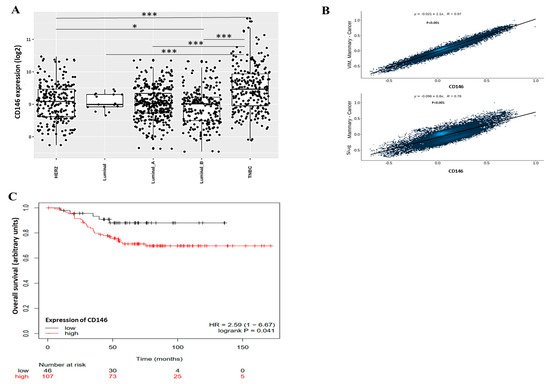
Figure 1. Expression of CD146, correlation with EMT markers and effect on overall survival in patients with breast cancer using public databases. (A) CD146 expression was determined in different subtypes of breast cancer, including HER2 cancer, luminal cancer and Triple Negative Breast Cancer (TNBC). Data were analyzed using gent2 in silico tool (http://gent2.appex.kr/gent2; 12 November 2021). (B) Expression of EMT markers (Vimentin and Slug) were correlated with CD146 expression in patients with breast cancer. Data were obtained from GitHub repository using correlation AnalyzeR (https://gccri.bishop-lab.uthscsa.edu/shiny/correlation-analyzer; 12 November 2021). (C) Overall survival of 153 patients with TNBC was given as a function of the low or high expression of CD146. Data were from the TCGA dataset and analyzed using Kaplan–Meier Plotter tool (https://kmplot.com/analysis/index.php?p=service; 12 November 2021). *, ***: p < 0.05, p < 0.001, comparison between breast cancer subtypes.
In addition, CD146 expression was significantly correlated with several EMT markers, such as vimentin or slug (Figure 8B). This is in accordance with our results showing that high CD146 MDA-MB-231 cells secrete high levels of sCD146 that, in turn, is able to increase vimentin and slug expression. Finally, clinical studies evidenced a significant decrease in overall survival rate in TNBC patients bearing high CD146 tumors as compared to tumors with weak CD146 expression (Figure 1C).
This confirms the fact that CD146/sCD146 are relevant markers in this pathology and could represent potential targets for therapy. This is also in accordance with the review of De Kruijff et al. showing that, in univariable analysis, CD146 expression was a prognostic factor for both metastasis-free survival and overall survival [11].
However, it is highly difficult to specifically target CD146 in cancer in general, and in TNBC in particular, essentially because of the high expression of the molecule on surrounding cells, such as the whole vascular system, and of its important physiological functions [28]. In addition, CD146 is able to act through its soluble form generated from the shedding of the membrane form. It was hypothesized that targeting sCD146 could constitute a relevant therapeutic approach.
This original approach was comforted by the sCD146 effects observed in CD146-high MDA-MB-231 cells. To this end, it thus took advantage of the recent generation of an antibody specifically targeting sCD146, namely the M2J-1 mAb [25]. In our study, this antibody was able to counteract the effects of sCD146 on proliferation, migration and invasion in vitro as well as on CSC and EMT markers both in vitro and in vivo. In addition, it was able to reduce the growth and dissemination of CD146-high MD-MBA-231 cells in two experimental animal models.
These reported effects of M2J-1 mAb are of major importance since, up to today, the therapeutic options to fight TNBC are very few. The recent development of sacituzumab govitecan that targets Trop2 has increased the survival of patients; however, many mechanisms of resistance to the molecule can appear, mainly through genetic mutations [29]. Immunotherapy has also been shown to be of interest, in particular by combining atezolizumab, an anti-PDL1 antibody, with chemotherapy [30]. It can thus speculate that, in TNBC expressing CD146, combining these therapies with our newly anti-sCD146 antibody M2J-1 could be of therapeutic benefit in order to prevent TNBC dissemination and to increase the overall survival of women attained with this pathology.
This entry is adapted from the peer-reviewed paper 10.3390/ijms23020974
References
- Zheng, B.; Ohuchida, K.; Chijiiwa, Y.; Zhao, M.; Mizuuchi, Y.L.; Horioka, K.; Ohtsuka, T.; Mizumoto, K.; Oda, Y.; Hashizume, M.; et al. CD146 Attenuation in Cancer-Associated Fibroblasts Promotes Pancreatic Cancer Progression. Mol. Carcinog. 2016, 55, 1560–1572.
- Li, W.; Yang, D.; Wang, S.; Guo, X.; Lang, R.; Fan, Y.; Gu, F.; Zhang, X.; Niu, Y.; Yan, X.; et al. Increased expression of CD146 and microvessel density (MVD) in invasive micropapillary carcinoma of the breast: Comparative study with invasive ductal carcinoma-not otherwise specified. Pathol. Res. Pract. 2011, 207, 739–746.
- Wu, G.J.; Peng, Q.; Fu, P.; Wang, S.W.; Chiang, C.F.; Dillehay, D.L.; Wu, M.W. Ectopical expression of human MUC18 increases metastasis of human prostate cancer cells. Gene 2004, 327, 201–213.
- Wu, Z.; Wu, Z.; Li, J.; Yang, X.; Wang, Y.; Yu, Y.; Ye, J.; Xu, C.; Qin, W.; Zhang, Z. MCAM is a novel metastasis marker and regulates spreading, apoptosis and invasion of ovarian cancer cells. Tumour Biol. 2012, 33, 1619–1628.
- Jiang, G.; Zhang, L.; Zhu, Q.; Bai, D.; Zhang, C.; Wang, X. CD146 promotes metastasis and predicts poor prognosis of hepatocellular carcinoma. J. Exp. Clin. Cancer Res. 2016, 35, 38.
- Halt, K.; Parssinen, H.; Junttila, S.; Sim-Lucas, S.; Koivunen, P.; Myllyharju, J.; Quaggin, S.; Skovorodkin, I.; Vainio, S. CD146 cells are essential for kidney vasculature development. Kidney Int. 2016, 90, 311–324.
- Imbert, A.M.; Garulli, C.; Choquet, E.; Koubi, M.; Aurrand-Lions, M.; Chabannon, C. CD146 expression in human breast cancer cell lines induces phenotypic and functional changes observed in epithelial to mesenchymal transition. PLoS ONE 2012, 7, e43752.
- Mani, S.A.; Guo, W.; Liao, M.J.; Eaton, E.N.; Ayyanan, A.; Zhou, A.Y.; Brooks, M.; Reinhard, F.; Zhang, C.C.; Shipitsin, M.; et al. The epithelial-mesenchymal transition generates cells with properties of stem cells. Cell 2008, 133, 704–715.
- Zeng, Q.; Li, W.; Lu, D.; Wu, Z.; Duan, H.; Luo, Y.; Feng, J.; Yang, D.; Fu, L.; Yan, X. CD146, an epithelial mesenchymal transition inducer, is associated with triple-negative breast cancer. Proc. Natl. Acad. Sci. USA 2012, 109, 1127–1132.
- Zabouo, G.; Imbert, A.M.; Jacquemier, J.; Finetti, P.; Moreau, T.; Esterni, B.; Birnbaum, D.; Bertucci, F.; Chabannon, C. CD146 expression is associated with a poor prognosis in human breast tumors and with enhanced motility in breast cancer cell lines. Breast Cancer Res. 2009, 11, R1.
- De Kruijff, I.; Timmermans, A.; den Bakker, M.; Trapman-Jansen, A.; Foekens, R.; Meijer-Van Gelder, M.; Oomen-de Hoop, E.; Smid, M.; Hollestelle, A.; van Deurzen, C.; et al. The Prevalence of CD146 Expression in Breast Cancer Subtypes and Its Relation to Outcome. Cancers 2018, 10, 134.
- So, J.H.; Hong, S.K.; Kim, H.T.; Jung, S.H.; Lee, M.S.; Choi, J.H.; Bae, Y.K.; Kudoh, T.; Kim, J.H.; Kim, C.H. Gicerin/CD146 is involved in zebrafish cardiovascular development and tumor angiogenesis. Genes Cells 2010, 15, 1099–1110.
- Schlagbauer-Wadl, H.; Jansen, B.; Muller, M.; Polterauer, P.; Wolff, K.; Eichler, H.G.; Pehamberger, H.; Konak, E.; Johnson, J.P. Influence of MUC18/MCAM/CD146 expression on human melanoma growth and metastasis in SCID mice. Int. J. Cancer 1999, 81, 951–955.
- Tsuchiya, S.; Tsukamoto, Y.; Furuya, M.; Hiroi, S.; Miki, N.; Sasaki, F.; Taira, E. Gicerin, a cell adhesion molecule, promotes the metastasis of lymphoma cells of the chicken. Cell Tissue Res. 2003, 314, 389–397.
- Tsukamoto, Y.; Sakaiuchi, T.; Hiroi, S.; Furuya, M.; Tsuchiya, S.; Sasaki, F.; Miki, N.; Taira, E. Expression of gicerin enhances the invasive and metastatic activities of a mouse mammary carcinoma cell line. Int. J. Oncol. 2003, 23, 1671–1677.
- Wu, G.J.; Fu, P.; Chiang, C.F.; Huss, W.J.; Greenberg, N.M.; Wu, M.W. Increased expression of MUC18 correlates with the metastatic progression of mouse prostate adenocarcinoma in the TRAMP model. J. Urol. 2005, 173, 1778–1783.
- Aldovini, D.; Demichelis, F.; Doglioni, C.; Di Vizio, D.; Galligioni, E.; Brugnara, S.; Zeni, B.; Griso, C.; Pegoraro, C.; Zannoni, M.; et al. M-CAM expression as marker of poor prognosis in epithelial ovarian cancer. Int. J. Cancer 2006, 119, 1920–1926.
- Kristiansen, G.; Yu, Y.; Schluns, K.; Sers, C.; Dietel, M.; Petersen, I. Expression of the cell adhesion molecule CD146/MCAM in non-small cell lung cancer. Anal. Cell Pathol. 2003, 25, 77–81.
- Oka, S.; Uramoto, H.; Chikaishi, Y.; Tanaka, F. The Expression of CD146 Predicts a Poor Overall Survival in Patients with Adenocarcinoma of the Lung. Anticancer Res. 2012, 32, 861–864.
- Ouellette, D.; Desbiens, G.; Emond, C.; Beauchamp, G. Lung cancer in women compared with men: Stage, treatment, and survival. Ann. Thorac. Surg. 1998, 66, 1140–1143.
- Zeng, P.; Li, H.; Lu, P.; Zhou, L.; Tang, M.; Liu, C.; Chen, M. Prognostic value of CD146 in solid tumor: A Systematic Review and Meta-analysis. Sci. Rep. 2017, 7, 4223.
- Shih, L.M.; Hsu, M.Y.; Palazzo, J.P.; Herlyn, M. The cell–cell adhesion receptor Mel-CAM acts as a tumor suppressor in breast carcinoma. Am. J. Pathol. 1997, 151, 745–751.
- Tripathi, S.C. MCAM mediates chemoresistance in small cell lung cancer via the PI3K/AKT/SOX2 signaling pathway. Cancer Res. 2017, 77, 4414–4425.
- Stalin, J.; Nollet, M.; Garigue, P.; Fernandez, S.; Vivancos, L.; Essaadi, A.; Muller, A.; Bachelier, R.; Foucault-Bertaud, A.; Fugazza, L.; et al. Targeting soluble CD146 with a neutralizing antibody inhibits vascularization, growth and survival of CD146-positive tumors. Oncogene 2016, 35, 5489–5500.
- Stalin, J.; Traboulsi, W.; Vivancos-Stalin, L.; Nollet, M.; Joshkon, A.; Bachelier, R.; Guillet, B.; Lacroix, R.; Foucault-Bertaud, A.; Leroyer, A.; et al. Therapeutic targeting of soluble CD146/MCAM with the M2J-1 monoclonal antibody prevents metastasis development and procoagulant activity in CD146-positive invasive tumors. Int. J. Cancer 2020, 147, 1666–1679.
- Reinhold Arnold, C.; Mangesius, J.; Skvortsova, I.-I.; Ganswindt, U. The role of cancer stem cell in radiation resistance. Front. Oncol. 2020, 10, 164.
- Mostert, B.; Kraan, J.; Bolt-de Vries, J.; van der Spoel, P.; Sieuwerts, A.M.; Schutte, M.; Timmermans, A.M.; Foekens, R.; Martens, J.W.M.; Gratama, J.-W.; et al. Detection of circulating tumor cells in breast cancer may improve through enrichment with anti-CD146. Breast Cancer Res. Treat. 2010, 127, 33–41.
- Leroyer, A.S.; Blin, M.G.; Bachelier, R.; Bardin, N.; Blot-Chabaud, M.; Dignat-George, F. CD146 (Cluster of Differentiation 146). Arterioscler. Thromb. Vasc. Biol. 2019, 39, 1026–1033.
- Zaman, S.; Jadid, H.; Denson, A.; Gray, J. Targeting Trop-2 in solid tumors: Future prospects. OncoTargets Ther. 2019, 12, 1781–1790.
- Van Wambeke, S.; Gyawali, B. Atezolizumab in Metastatic Triple-Negative Breast Cancer—No Contradiction in the Eyes of a Dispassionate Observer. JAMA Oncol. 2021, 7, 1285–1286.
This entry is offline, you can click here to edit this entry!
