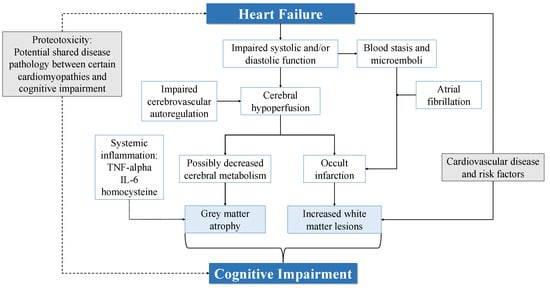
Several pathophysiological pathways have been proposed to contribute to the structural brain changes and CI among patients with HF. These are outlined in Figure 1.
2.1. Cerebral Hypoperfusion and Impaired Autoregulation
Reduced cerebral blood flow (CBF) is one of the proposed mechanisms of brain injury and CI in HF [
55,
58]. Several studies have demonstrated lower CBF velocities on transcranial Doppler (TCD) in those with HF [
59,
60,
61]. Furthermore, TCD measurements in patients with HF showed a decline over a 12-month period [
62]. Lower CBF in HF patients impacted global cognitive function, attention and executive function [
62,
63], while reduced regional hippocampal CBF was associated with poorer performance on measures of delayed memory [
64]. A low output state in HF may result in chronic cerebral hypoperfusion in patients with HF, making them more susceptible to watershed infarcts. Additionally, owing to the similar risk factors shared by patients with HF and cerebrovascular disease, patients with HF may also have a poorer collateral blood supply due to atheromatous stenosis of the cerebral arteries [
43]. Some studies compared CBF measurements against structural neuroimaging or neuropsychological testing and evaluated the relationship between CBF and CI in HF [
55,
59]. Alosco et al. found that reduced CBF in patients with HF was associated with increased WMLs, which were in turn related to poorer MMSE scores [
59]. Vogels et al. similarly described lower CBF in patients with HF, but did not find a correlation with brain changes on neuroimaging [
55].
In the general population, Jefferson et al. reported higher MRI-assessed cardiac index to be positively related to total brain volume and information processing speed [
58]. Similarly, a lower cardiac index was associated with increased dementia risk [
29]. In a study of 4366 individuals from the United Kingdom Biobank, van Hout et al. found that individuals with subclinical reduced left ventricular EF had reduced total brain volume and GM volume, and also increased WMLs [
65]. Interestingly, only WM and hippocampal volume loss were associated with CI, and both were not related to EF [
65]. Arterial stiffness, microvascular damage, atherosclerosis and inflammation in HF may possibly confound the reported relationship between EF and CI. These pathophysiological mechanisms are adversely associated with both cardiac function and cognition, making it difficult to ascertain the true association between EF and CI [
66,
67]. However, Park et al. found that total brain volume and hippocampal volume remained associated with poorer left ventricular systolic function even after adjustment for cardiometabolic disease [
37]. Left ventricular stroke volume and cardiac output have also been linked to CI [
68]. The potential mechanisms by which cardiac dysfunction may influence brain atrophy are not well understood but may be related to decreased cerebral metabolism. Patients with HF with extensive hibernating myocardium had reduced cerebral metabolism in frontal and hippocampal areas in a study utilising 18F-flurodeoxyglucose positron emission tomography/computed tomography (18F-FDG PET/CT) imaging [
69].
A reduced CBF is unlikely to be the sole explanation for cortical GM loss [
16,
54]. Brain areas such as the periventricular white matter, basal ganglia and hippocampus are susceptible to cerebral hypoperfusion due to their location at the junction of large-vessel arterial territories, or due to their irrigation by long-penetrating end arterioles. In contrast, the cortex has a rich dual blood supply and can better tolerate cerebral hypoperfusion [
43,
70]. The interplay of other cardiovascular risk factors may also contribute to cortical GM loss, since similar patterns of GM loss have been observed in HF and IHD patients [
16]. Leeuwis et al. further argued that CBF may not be the main reason for CI in HF in light of their findings that while CBF was lower in patients with HF, this did not correspond with reduced cognitive function [
71].
CBF has been shown to increase after heart transplantation [
72] and heart transplantation has been associated with improved cognitive function [
73,
74]. Cognitive improvement has also been reported after left ventricular assist device (LVAD) placement [
75,
76]. However, these improvements were marginal and MoCA scores increased by approximately 1.6 following LVAD placement [
76]. Schall et al., on the other hand, did not find a significant difference between pre- and post-operative cognitive scores after 7.7 months in their patients with dilated cardiomyopathy who underwent heart transplantation, despite greatly improved physical health [
77]. A possible explanation is the shorter follow-up duration compared to other studies [
73]. Several cognitive scores showed a non-statistically significant increase and a longer reassessment interval may have revealed further cognitive improvement [
77]. Another reason may be the use of an extensive neuropsychological battery by Schall et al. compared to less rigorous screening measures such as the MoCA in other studies [
74]. Patients with HF may also have diminished cerebrovascular autoregulation, with greater impairments in those with NYHA IV compared to NYHA II and III. Accordingly, cerebral oxygen saturations were found to be lower in patients with HF [
78,
79]. Previous studies have shown a blunted haemodynamic response and greater CBF reduction in patients with HF in response to upright posture [
80,
81]. More recently, Kharraziha et al. observed a more pronounced decrease in cerebral tissue oxygen saturations in response to head-up tilt in patients with HF [
82]. While it is unclear how HF may lead to impaired autoregulation, it could result in increased susceptibility to low cardiac output states due to an inability to maintain CBF via vasodilatory mechanisms.