Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Others
Cornelia de Lange syndrome (CDLS) is caused by pathogenic variants in genes which are structural or regulatory components of the cohesin complex. The classical Cornelia de Lange (CDLS) phenotype is characterized by distinctive facial features, growth retardation, upper limb reduction defects, hirsutism, and developmental delay. Non-classical phenotypes make this condition heterogeneous.
- Cornelia de Lange
- genetic syndrome
- fetal syndrome
- fetal ultrasound
1. Prenatal Presentation of a Classical CDLS Case
We report a case of prenatal diagnosis of CDLS at 29 weeks’ gestation in a 30-year-old woman who had previously delivered a normal baby. The patient was referred to our fetal medicine unit because of fetal growth restriction, diagnosed at 24 weeks’ gestation. As no Doppler flow anomalies were detected, a genetic anomaly (lethal trisomy) rather than placental insufficiency was suspected by the referring doctors. Ultrasound examination in our unit demonstrated symmetrical fetal growth restriction with normal Doppler studies. The amniotic fluid was increased with a deepest vertical pool of 9.2 cm. Examination of the fetal face showed abnormal profile, synophrys, depressed nasal bridge, long downturned upper lip, and micrognathia (Figure 1A,B). Cardiac examination demonstrated abnormal flow through the atrio-ventricular, aortic, and pulmonary valves. The third finger of the right fetal hand was missing, and the fingers of the left hand were overlapping.
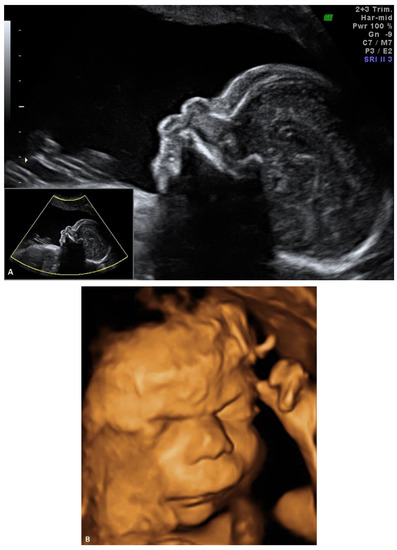

Figure 1. Ultrasound examination of the fetal face in a CDLS case with classical phenotype: (A) 2D image of the fetal profile at 29 w of gestation, showing mild micrognathia/retrognathia; abnormal philtrum; depressed nasal bridge; (B) Volume reconstruction of the fetal face at 29 w of gestation; (C) Volume reconstruction of the fetal face at 34 w of gestation.
The suspected diagnosis was Cornelia de Lange syndrome, CDLS. We discussed the findings with the patient, and we presented the parents with the choice of a late amniocentesis. We explained that lethal conditions such as trisomy 18 or 13 can be ruled out only by direct genetic testing. We described the genetic tests that can be performed for CDLS and we discussed the limitations of such tests, given the circumstances. A geneticist was involved in the counselling. The parents refused any prenatal genetic testing, as they were committed to the pregnancy.
The initial ultrasound findings persisted in the third trimester (Figure 1C). As pregnancy progressed the polyhidramnios worsened but did not become tense and did not require amniodrainage. Fetal skin edema was seen in late pregnancy.
A male infant weighing 2030 g was delivered by cesarean section at 38 weeks of gestation. An experienced neonatologist was present at birth. CDLS was confirmed by clinical examination demonstrating synophrys, long eyelashes, short upturned nose, thin downturned lips, long philtrum, excessive body hair, mild aortic valve stenosis and moderate aortic arch hypoplasia, missing fingers, and severe gastroesophageal reflux. A multidisciplinary team, including a geneticist, was involved in the care of the baby. Genetic testing was offered after birth, but it was declined by the parents of the baby.
This entry is adapted from the peer-reviewed paper 10.3390/diagnostics11010142
This entry is offline, you can click here to edit this entry!
