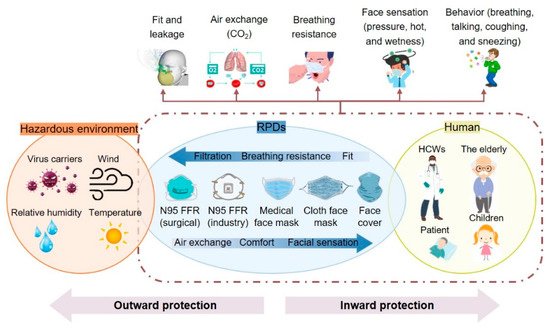
Respiratory protective devices (RPDs) play a crucial role in controlling infection, particularly for viruses like SARS-CoV-2 that have a high transmission rate, strong viability, multiple infection routes and mechanisms, and emerging new variants that could reduce the efficacy of existing vaccines.
- respiratory protective device
- decontamination
- Respiratory Protection
1. Introduction
Respiratory protective devices (RPDs) play a crucial role in controlling infection, particularly for viruses like SARS-CoV-2 that have a high transmission rate, strong viability, multiple infection routes and mechanisms, and emerging new variants that could reduce the efficacy of existing vaccines.
2. RPD Performance, Issues, and Challenges
3. Decontamination and Reuse of RPDs
This entry is adapted from the peer-reviewed paper 10.3390/polym13234165
References
- Racz, L.; Yamamoto, D.P.; Eninger, R.M. Handbook of Respiratory Protection: Safeguarding against Current and Emerging Hazards; CRC Press: Boca Raton, FL, USA, 2017.
- CDC. 42 CFR Part 84 Respiratory Protective Devices. 1997. Available online: https://www.cdc.gov/niosh/npptl/topics/respirators/pt84abs2.html (accessed on 10 October 2021).
- FDA. Face Masks, Including Surgical Masks, and Respirators for COVID-19. 2020. Available online: https://www.fda.gov/medical-devices/coronavirus-covid-19-and-medical-devices/face-masks-including-surgical-masks-and-respirators-covid-19 (accessed on 12 October 2021).
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Sciences Policy; Committee on the Use of Elastomeric Respirators in Health Care. Reusable Elastomeric Respirators in Health Care: Considerations for Routine and Surge Use; Liverman, C.T., Yost, O.C., Rogers, B.M.E., Clever, L.H., Eds.; National Academies Press (US): Washington, DC, USA, 2018.
- National Academies of Sciences, Engineering, and Medicine. Current Issues in the Assessment of Respiratory Protective Devices for Occupational and Non-Occupational Uses: Proceedings of a Workshop; The National Academies Press: Washington, DC, USA, 2021.
- Karim, N.; Afroj, S.; Lloyd, K.; Oaten, L.C.; Andreeva, D.V.; Carr, C.; Farmery, A.D.; Kim, I.-D.; Novoselov, K.S. Sustainable personal protective clothing for healthcare applications: A review. ACS Nano 2020, 14, 12313–12340.
- Chua, M.H.; Cheng, W.; Goh, S.S.; Kong, J.; Li, B.; Lim, J.Y.C.; Mao, L.; Wang, S.; Xue, K.; Yang, L.; et al. Face masks in the new COVID-19 normal: Materials, testing, and perspectives. Research 2020, 2020, 7286735.
- Blachere, F.M.; Lemons, A.R.; Coyle, J.P.; Derk, R.C.; Lindsley, W.G.; Beezhold, D.H.; Woodfork, K.; Duling, M.G.; Boutin, B.; Boots, T. Face mask fit modifications that improve source control performance. medRxiv 2021.
- Patel, R.B.; Skaria, S.D.; Mansour, M.M.; Smaldone, G.C. Respiratory source control using a surgical mask: An in vitro study. J. Occup. Environ. Hyg. 2016, 13, 569–576.
- O’Dowd, K.; Nair, K.M.; Forouzandeh, P.; Mathew, S.; Grant, J.; Moran, R.; Bartlett, J.; Bird, J.; Pillai, S.C. Face masks and respirators in the fight against the COVID-19 pandemic: A review of current materials, advances and future perspectives. Materials 2020, 13, 3363.
- AATCC. AATCC M14-2020 Guidance and Considerations for General Purpose Textile Face Coverings: Adult; AATCC: Research Triangle, NC, USA, 2020.
- ASTM. ASTM F3502-21 Standard Specification for Barrier Face Coverings; ASTM International: West Conshohocken, PA, USA, 2021.
- Furukawa, N.W.; Brooks, J.T.; Sobel, J. Evidence supporting transmission of severe acute respiratory syndrome coronavirus 2 while presymptomatic or asymptomatic. Emerg. Infect. Dis. 2020, 26, e201595.
- Gómez-Ochoa, S.A.; Franco, O.H.; Rojas, L.Z.; Raguindin, P.F.; Roa-Díaz, Z.M.; Wyssmann, B.M.; Guevara, S.L.R.; Echeverría, L.E.; Glisic, M.; Muka, T. COVID-19 in health-care workers: A living systematic review and meta-analysis of prevalence, risk factors, clinical characteristics, and outcomes. Am. J. Epidemiol. 2021, 190, 161–175.
- He, D.; Zhao, S.; Lin, Q.; Zhuang, Z.; Cao, P.; Wang, M.H.; Yang, L. The relative transmissibility of asymptomatic COVID-19 infections among close contacts. Int. J. Infect. Dis. 2020, 94, 145–147.
- Gandhi, M.; Yokoe, D.S.; Havlir, D.V. Asymptomatic Transmission, the Achilles’ Heel of Current Strategies to Control COVID-19. In The COVID-19 Reader; Routledge: London, UK, 2020; pp. 36–39.
- Gao, Z.; Xu, Y.; Sun, C.; Wang, X.; Guo, Y.; Qiu, S.; Ma, K. A systematic review of asymptomatic infections with COVID-19. J. Microbiol. Immunol. Infect. 2021, 54, 12–16.
- Feng, Y.; Marchal, T.; Sperry, T.; Yi, H. Influence of wind and relative humidity on the social distancing effectiveness to prevent COVID-19 airborne transmission: A numerical study. J. Aerosol Sci. 2020, 147, 105585.
- Dbouk, T.; Drikakis, D. On respiratory droplets and face masks. Phys. Fluids 2020, 32, 063303.
- Setti, L.; Passarini, F.; De Gennaro, G.; Barbieri, P.; Perrone, M.G.; Borelli, M.; Palmisani, J.; Di Gilio, A.; Piscitelli, P.; Miani, A. Airborne transmission route of COVID-19: Why 2 meters/6 feet of inter-personal distance could not be enough. Int. J. Environ. Res. Public Health 2020, 17, 2932.
- WHO. Transmission of SARS-CoV-2: Implications for Infection Prevention Precautions. 2020. Available online: https://www.who.int/news-room/commentaries/detail/transmission-of-sars-cov-2-implications-for-infection-prevention-precautions (accessed on 15 October 2021).
- CDC. CDC Calls on Americans to Wear Masks to Prevent COVID-19 Spread. 2020. Available online: https://www.cdc.gov/media/releases/2020/p0714-americans-to-wear-masks.html (accessed on 2 October 2021).
- Howard, J.; Huang, A.; Li, Z.; Tufekci, Z.; Zdimal, V.; van der Westhuizen, H.-M.; von Delft, A.; Price, A.; Fridman, L.; Tang, L.-H.; et al. An evidence review of face masks against COVID-19. Proc. Natl. Acad. Sci. USA 2021, 118, e2014564118.
- Liang, M.; Gao, L.; Cheng, C.; Zhou, Q.; Uy, J.P.; Heiner, K.; Sun, C. Efficacy of face mask in preventing respiratory virus transmission: A systematic review and meta-analysis. Travel Med. Infect. Dis. 2020, 36, 101751.
- Cheng, Y.; Ma, N.; Witt, C.; Rapp, S.; Wild, P.S.; Andreae, M.O.; Pöschl, U.; Su, H. Face masks effectively limit the probability of SARS-CoV-2 transmission. Science 2021, eabg6296.
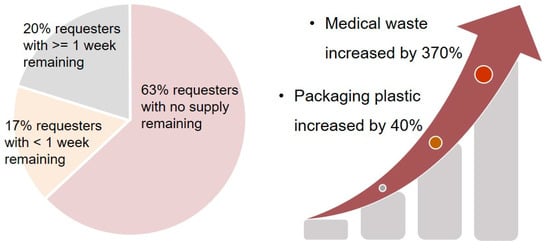
- O’Reilly, K.B. Amid PPE Shortage, AMA Collaboration Offers Supplier for Doctors. 2020. Available online: https://www.ama-assn.org/delivering-care/public-health/amid-ppe-shortage-ama-collaboration-offers-supplier-doctors (accessed on 10 October 2021).
- GUP. PPE Data on the Personal Protective Equipment Shortage across the U.S. 2021. Available online: https://getusppe.org/data/ (accessed on 19 November 2021).
- Dean, R. PPE: Polluting Planet Earth. Br. Dent. J. 2020, 229, 267.
- Vanapalli, K.R.; Sharma, H.B.; Ranjan, V.P.; Samal, B.; Bhattacharya, J.; Dubey, B.K.; Goel, S. Challenges and strategies for effective plastic waste management during and post COVID-19 pandemic. Sci. Total Environ. 2021, 750, 141514.
- Gorrasi, G.; Sorrentino, A.; Lichtfouse, E. Back to plastic pollution in COVID times. Environ. Chem. Lett. 2021, 19, 1–4.
- Prata, J.C.; Silva, A.L.; Walker, T.R.; Duarte, A.C.; Rocha-Santos, T. COVID-19 pandemic repercussions on the use and management of plastics. Environ. Sci. Technol. 2020, 54, 7760–7765.
- Silva, A.L.P.; Prata, J.C.; Walker, T.R.; Duarte, A.C.; Ouyang, W.; Barcelò, D.; Rocha-Santos, T. Increased plastic pollution due to COVID-19 pandemic: Challenges and recommendations. Chem. Eng. J. 2020, 405, 126683.
- Singh, N.; Tang, Y.; Zhang, Z.; Zheng, C. COVID-19 waste management: Effective and successful measures in Wuhan, China. Resour. Conserv. Recycl. 2020, 163, 105071.
- Harhay, M.O.; Halpern, S.D.; Harhay, J.S.; Olliaro, P.L. Health care waste management: A neglected and growing public health problem worldwide. Trop. Med. Int. Health 2009, 14, 1414–1417.
- WHO. Health-Care Waste. 2018. Available online: https://www.who.int/news-room/fact-sheets/detail/health-care-waste (accessed on 10 October 2021).
