Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Orthopedics
Coronal shear fractures are partial or complete articular fractures of the distal humerus without involvement of the columns, which can affect the capitellum, the trochlea, or both.
- shear fractures
- capitellum
- coronal fractures
- distal humerus fractures
- trochlea
- headless screws
- Dubberley
- elbow articular fractures
1. Classification
The Bryan–Morrey classification [1] is strictly focused on the capitellum. Type 1 (Hahn–Steinthal fracture) is a fracture that involves only the capitellum with attached subchondral bone. Type 2 (Kocher–Lorenz fracture) is an isolated fracture of the capitellum with the fragment consisting mainly on articular cartilage. Type 3 (Broberg–Morrey fracture) is an isolated capitellar fracture with comminution. A type 4 lesion (McKee fracture) [2] was further added and is a capitellar fracture that extends medially into the trochlea. Watts et al., reviewed 79 coronal shear fractures and observed that type 1 fracture was the most common one (47%) followed by type 4 (41%); type 2 occurred in 8% and type 3 in 4% [3].
Dubberley et al., published a more recent classification to better characterize capitellar fractures in order to drive the surgical management and to potentially predict the outcomes [4]. Type 1 is an isolated fracture of the capitellum extended to the most lateral portion of the trochlea (i.e., the equivalent to the Hahn–Steinthal fracture). Type 2 is a fracture of the capitellum and trochlea in a single fragment (i.e., the equivalent to the McKee fracture). Type 3 involves both the capitellum and the trochlea as separate fragments. These three types are further divided into subtype A—without posterior comminution or subtype B—with posterior comminution. Watson et al. proposed a rare “Type 4 fracture” which is a type 3 fracture with associated sagittal and axial plane fracture lines, creating multiple smaller fragments of the capitellum and trochlea [5]. This type of fracture is mainly seen in osteoporotic patients (Figure 1). One limitation of the Dubberley classification is that it does not include the associated injuries. There are no robust scientific data to draw conclusions on how these injuries influence both the treatment and the clinical outcomes.
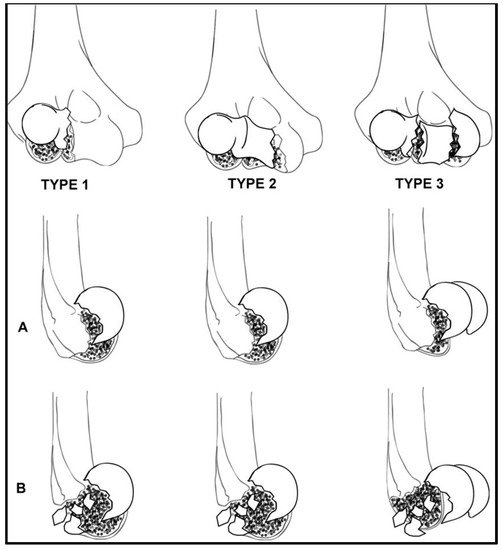
Figure 1. The Dubberley classification of capitellar and trochlear fractures. Subtype (A) fractures are not characterized by posterior comminution, while Subtype (B) show posterior comminution (From Dubberley J.H., Faber K.J. and Macdermid J.C. et al. Outcome after open reduction and internal fixation of capitellar and trochlear fractures. J Bone Joint Surg Am 2006; 88: 47 [4]; with permission).
The rare isolated fractures of the trochlea (T) can be included in the Dubberley classification as type 1T, differentiating it from fractures of the capitellum.
Ring and Jupiter proposed another descriptive classification [6]. Type 1 is a coronal shear fracture composed of a singular articular fragment that includes the capitellum and the lateral portion of the trochlea. Type 2 involves the lateral epicondyle. Type 3 is characterized by a further impaction of the metaphyseal bone behind the capitellum in the distal and posterior aspect of the lateral column. Type 4 is a fracture that includes the posterior aspect of the trochlea. Lastly, type 5 is a fracture that involves the medial epicondyle.
Finally, there is the AO-ASIF classification [7]. Coronal shear fractures are classified as type 13B3 (distal humerus, partial articular, frontal/coronal plane): 13B3.1 for capitellar fractures; 13B3.2 for trochlea fractures, and 13B3.3 for both capitellar and trochlea fractures.
2. Treatment Options and Results
2.1. Planning
In order to best plan the treatment, careful evaluation of the fracture morphology and associated injuries with the CT scan should be done. Posterior comminution poses higher risk of avascular necrosis and biomechanical failure of fracture fixation [8][3][9]. Medial extension drives the decision regarding the choice of surgical approach between a lateral, extended lateral, combined lateral and medial, or olecranon osteotomy approaches [8][5][10]. Impacted fracture fragments can be difficult to detect intraoperatively; if not identified pre-operatively, anatomic fracture reduction may not be possible. The associated radial head and more rarely, coronoid fractures, are diagnosed with the CT scan. Data regarding treatment of radial head fractures in the setting of coronal shear fractures are lacking. Nevertheless, the radial head should be treated as a fracture-dislocation, and fixation versus replacement should be performed depending on the level of comminution.
Associated LUCL tears are more difficult to diagnose pre-operatively, and the diagnosis is typically intraoperative. We believe that LUCL tears are common. Additionally, during the extended lateral approach the LUCL often needs to be detached if it is not already torn. Thus, the LUCL is almost always repaired.
2.2. Nonoperative Treatment
Few studies have reported on closed treatment with marginal results [11][12][13][14][15][16][17]. Ochner et al. described a closed maneuver performed acutely after the injury in noncomminuted fractures [13]. After extension and supination, the elbow undergoes traction and varus stress followed by flexion and pronation. Then, the elbow is immobilized in a cast for around 3 weeks. More recently, Catbush et al. described seven adult patients fracture conservatively treated and no signs of fracture displacement, osteoarthritis, or avascular necrosis [17]. After an average follow-up of 41.6 months, patients showed 97% of their active elbow flexion, 83% of elbow extension, and full pronation–supination. However, the study only included Bryan–Morrey type 1 fractures, which represent only around 40% of all the shear fractures.
Although no robust scientific data exists that can help the surgeon decide, nonsurgical treatment is not usually recommended, as it is associated with a high risk of stiffness, pain, and post-traumatic arthritis [11][12][13]. Patients unfit to have surgery could have consideration of this option [10][18][19].
2.3. Fragment Excision
Excision is an option for small fracture fragments that are determined to be not fixable. The risk of intraarticular adhesions following the exposure of cancellous subchondral bone must be taken into consideration [20]. If the fracture involves the lateral trochlear ridge or further, excision is contraindicated, as it may destabilize the elbow [21]; however, there are no published data to support excision based on fracture classification [16]. Additionally, a medial collateral ligament tear contraindicates excision, due to the subsequent risk of chronic valgus instability [11][22] (Figure 2).

Figure 2. (A) Preoperative CT scan and (B) post-operative X-rays of a Bryan–Morrey Type II fracture treated with fragment excision and lateral collateral ligament repair using a suture anchor.
In the largest series describing excision, some including the trochlea, 29 patients were retrospectively reviewed (20 treated with excision and 9 with fixation), the results of excision were fair or poor with mean loss of ROM of 40° [11]. Fowles et al. tried an initial non-operative treatment and a delayed fragment excision if the elbow remained symptomatic. Their case series describing six patients reported worse outcomes in three patients treated after a mean of 5.7 months after trauma than the three treated within 24 h from trauma (91° vs. 141° of flexion, respectively—some residual pain in the group was later treated) [23].
In the rare cases of an isolated fracture of the trochlea, fragment excision is not a viable option because of the key role of this portion in elbow function [24].
2.4. Arthroscopic Treatment
Arthroscopy has been proposed both for fragment excision and fixation [25][26][27][28]. With theoretical benefits of minimal dissection, no dynamic stabilizers disrupted, and lower risk of infection, arthroscopy has the potential for a more precise articular fracture control, removal of loose bodies, and perhaps a better evaluation of the medial part of the joint [26][27][28][29]. However, it is highly technically demanding and neurovascular structures are at risk of iatrogenic injury.
Comminution can be a contraindication to arthroscopic fixation, especially if posterior, (i.e., Dubberley subtypes B) [30]. A relative contraindication is the Dubberley 3A fracture, as the capitellum and trochlea present as separate fragments [27][29].
Only few cases are reported in the literature and some lack intraoperative images. However, the early results appear promising. Van Nguyen, et al. [29], recently described their arthroscopic technique without clinical results. [29] First, varus stress is applied, followed by progressive elbow extension to reduce the fracture under arthroscopic visualization. Then, the reduction is refined using an arthroscopic periosteal elevator in 90° elbow flexion inserted through the anterolateral portal. A probe inserted through the posterolateral portal helps maintain the reduction, while the fragment is temporarily fixed with Kirschner wires. Definitive fixation is performed retrograde with percutaneous headless compression screws under the control of both fluoroscopy and arthroscopy.
2.5. Open Reduction and Internal Fixation (ORIF)
Most of the patients sustaining coronal shear fractures undergo ORIF. Due to the relatively uncommon nature of the pathology, the literature mostly consists of case series. Comparison studies regarding surgical approach and type of fixation are not reported. There are no data suggesting the optimal timing for surgery. However, earlier is likely best in order to reduce the amount of intra-articular scar tissue, subchondral bony resorption, and cartilaginous edema. Early surgery can potentially reduce the risk of bone avascular necrosis and accelerate the rehabilitation program.
2.6. Surgical Approaches
The ideal surgical approach depends on fracture characteristics, associated injuries, and surgeon preference.
Either a lateral, anterolateral, combined lateral and medial, or posterior superficial approach can be chosen, with the latter preferred when the fracture line extends far medially and posterior. Then, a deep lateral approach is usually sufficient. The Kocher interval is developed [31] and, if the lateral ulnar collateral ligament (LUCL) is intact, the capsule between the extensor carpi ulnaris and the anconeus should be incised as far anterior as possible, in order to preserve the LUCL integrity [32]. When the fracture line extends toward the trochlea, an extended Kocher approach might be preferred [33]— starting the incision at the supracondylar ridge and detaching the origins of the wrist extensors and brachioradialis from the lateral condyle. The origin of the LUCL sometimes needs to be detached as well to expose the posterior capitellum or mobilize impacted fragments in order to obtain an anatomic reduction and adequate fixation. Additionally, by raising the LUCL origin off the bone, the joint can be hinged open to allow for better exposure of the medial trochlea, while preserving the olecranon and medial soft tissues. In certain cases, the lateral epicondyle is fractured and the joint can be exposed by simple mobilization of the fragment, with the LUCL remaining attached to the bone [34]. Whenever the LUCL or the lateral epicondyle is detached, it needs a careful reinsertion, with either suture anchors or bone tunnel fixation, in order to avoid posterolateral rotatory instability.
An anterolateral approach has been described utilizing an “S” shaped incision: the brachioradialis and the radial nerve are retracted laterally and the biceps medially [35]. An anterior longitudinal incision through the brachialis and the capsule follows. This is a particularly good option for Dubberley type 2A and 3A fractures [36]. The disadvantages are that this approach is not extensile, it requires retraction of nerves, and it does not allow visualization of the posterior aspect of the capitellum.
When better visualization of the trochlea is needed, a separate medial “over the top” approach, described by Hotchkiss, that spares the anterior bundle of the medial collateral ligament, can be used [4][6][37].
In cases where severe medial and posterior comminution is observed, an olecranon osteotomy is an option. However, it is important to note, as this approach preserves both the medial and lateral ulnar collateral ligaments, the most anterior portion of the distal humerus is not clearly exposed even with extreme elbow flexion. A separate lateral window is necessary to do so, with detachment of the extensor carpi radialis longus, the brachialis, and the anterior capsule of the humerus. A triceps-sparing approach with subperiosteal elevation of collateral ligaments origin allows excellent visualization, but the drawback is the associated risk of iatrogenic instability. This approach is a good option to treat a severely comminuted fracture with an elbow replacement.
2.7. Fixation Techniques
2.7.1. Isolated Screw Fixation
Screw fixation is the most frequently used type of fixation. Several types, including cortical, cancellous small fragment, Herbert, and headless compression screws, have been proposed [16].
Isolated screws are sufficient in some cases, including those of Dubberley subtype A fractures. After reducing the fracture by applying a clamp to obtain compression, the provisional fixation is obtained with Kirschner wires. These are usually the guide wires for the cannulated screws. If not, provisional Kirschner wires should be placed along the fracture margins so as not to interfere with placement of headless screws. We suggest the use of at least two screws and a divergent pattern (Figure 3) [38][39].
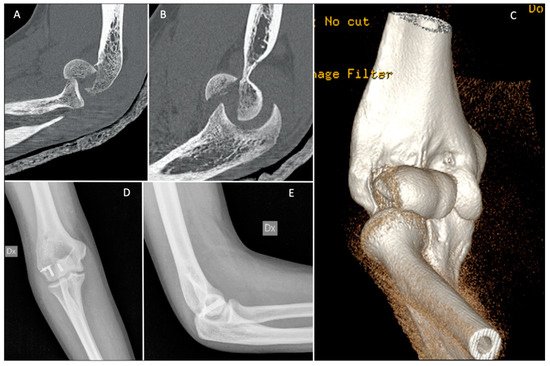
Figure 3. (A–C) Pre-operative CT scan; and (D,E) post-operative X-rays of a Dubberley 2A fracture fixed with independent antigrade headless screws.
Screws with heads need to be countersunk within the articular surface, but we prefer headless variable pitch screws. Matache et al., have recently demonstrated that the proximal third of the lateral trochlear ridge, on average around 5 mm in width, is a non-articulating region of the articular surface of the distal humerus. Thus, this area is a good point for screw insertion, especially when using an anterior-to-posterior lag screw; however, caution should be taken in small-statured patients that may have a smaller safe-zone [40].
In a biomechanical study, headless compression screws were demonstrated to provide a more stable fixation of capitellum fractures than four-millimeter partially threaded cancellous lag screws [41]. Both Herbert (Zimmer, Warsaw, Indiana) and Acutrak (Acumed Hillsboro Oregon) screws are options. However, after cyclic testing, which simulated physiologic loading, Acutrak screws inserted in the AP direction perpendicular to the articular surface proved to provide significantly more stable fixation than Herbert screws [42]. This might be due to the fully threaded, tapered shape, and variable pitch of the Acutrak screw. Nevertheless, several authors have reported good clinical outcomes using Herbert screws [43][44][45].
One limitation of the headless screws is the larger diameter due to the cannulation. Watson et al., have proposed the use of locking screws buried within the articular cartilage, as they have a low profile compared to a cortical screw, and very small diameter screws can be used [5].
The ideal orientation of the screws is still debated, and both options have limitations. Placing screws anterior-to-posterior causes damage to the joint surface. Alternatively, screws placed posterior-to-anterior pose a risk to the blood supply of the capitellum and trochlea. In a biomechanical study, the anterior-to-posterior direction provided a more stable fixation [41]. The posterior-to-anterior direction can potentially reduce the risk of collapse of the joint surface along with the subchondral bone, which at times is very thin. With collapse, the physiologic anterior offset of the capitellum is altered with subsequent risk of elbow instability due to the altered relationships between primary and secondary elbow stabilizers [46]. Lopiz et al., reported retrospectively on 18 patients, which were over the age of 65 and treated with either anterior-to-posterior (11 patients) or posterior-to-anterior (nine patients) cannulated screws. At a mean of 4.1 years of follow-up, elbow flexion, Mayo Elbow Performance Index and QuickDASH were slightly better in the posterior-to-anterior group, but the difference was not statistically significant [47]. When anterior-to-posterior orientation is preferred, biodegradable screws might be considered, as they have been shown to provide a similar biomechanical stability as metal screws [48]. However, the risk of reactive synovitis should be considered. Hirvensalo, et al. reported in a case series of eight patients, at a mean of 12 months of follow-up, one patient that developed synovitis that did not affect the final radiographic nor clinical outcomes [49].
This entry is adapted from the peer-reviewed paper 10.3390/jfmk7010007
References
- Morrey, B.F. The Elbow and Its Disorders, 2nd ed.; Saunders: Philadelphia, PA, USA, 1993.
- McKee, M.D.; Jupiter, J.B.; Bamberger, H.B. Coronal Shear Fractures of the Distal End of the Humerus. J. Bone Jt. Surg. Am. Vol. 1996, 78, 49–54.
- Watts, A.C.; Morris, A.; Robinson, C.M. Fractures of the Distal Humeral Articular Surface. J. Bone Jt. Surg. Br. Vol. 2007, 89, 510–515.
- Dubberley, J.H.; Faber, K.J.; Macdermid, J.C.; Patterson, S.D.; King, G.J.W. Outcome after Open Reduction and Internal Fixation of Capitellar and Trochlear Fractures. J. Bone Jt. Surg. Am. 2006, 88, 46–54.
- Watson, J.J.; Bellringer, S.; Phadnis, J. Coronal Shear Fractures of the Distal Humerus: Current Concepts and Surgical Techniques. Shoulder Elb. 2020, 12, 124–135.
- Ring, D.; Jupiter, J.B.; Gulotta, L. Articular Fractures of the Distal Part of the Humerus. J. Bone Jt. Surg. Am. Vol. 2003, 85, 232–238.
- Bandi, W.; Muller, M. Arbeitsgemeinschaft Fur Osteosynthesefragen. Manual of Internal Fixation: Techniques Recommended by the AO-Group; Springer: New York, NY, USA, 1979.
- Yamaguchi, K.; Sweet, F.A.; Bindra, R.; Morrey, B.F.; Gelberman, R.H. The Extraosseous and Intraosseous Arterial Anatomy of the Adult Elbow. J. Bone Jt. Surg. 1997, 79, 1653–1662.
- Sen, M.K.; Sama, N.; Helfet, D.L. Open Reduction and Internal Fixation of Coronal Fractures of the Capitellum. J. Hand Surg. 2007, 32, 1462–1465.
- Ruchelsman, D.E.; Tejwani, N.C.; Kwon, Y.W.; Egol, K.A. Open Reduction and Internal Fixation of Capitellar Fractures with Headless Screws. Surgical Technique. J. Bone Jt. Surg. Am. Vol. 2009, 91 Pt 1 (Suppl. 2), 38–49.
- Grantham, S.A.; Norris, T.R.; Bush, D.C. Isolated Fracture of the Humeral Capitellum. Clin. Orthop. Relat. Res. 1981, 161, 262–269.
- Alvarez, E.; Patel, M.R.; Nimberg, G.; Pearlman, H.S. Fracture of the Capitulum Humeri. J. Bone Jt. Surg. Am. Vol. 1975, 57, 1093–1096.
- Ochner, R.S.; Bloom, H.; Palumbo, R.C.; Coyle, M.P. Closed Reduction of Coronal Fractures of the Capitellum. J. Trauma 1996, 40, 199–203.
- Letts, M.; Rumball, K.; Bauermeister, S.; McIntyre, W.; D’Astous, J. Fractures of the Capitellum in Adolescents. J. Pediatric Orthop. 1997, 17, 315–320.
- Puloski, S.; Kemp, K.; Sheps, D.; Hildebrand, K.; Donaghy, J. Closed Reduction and Early Mobilization in Fractures of the Humeral Capitellum. J. Orthop. Trauma 2012, 26, 62–65.
- Trinh, T.Q.; Harris, J.D.; Kolovich, G.P.; Griesser, M.J.; Schickendantz, M.S.; Jones, G.L. Operative Management of Capitellar Fractures: A Systematic Review. J. Shoulder Elb. Surg. 2012, 21, 1613–1622.
- Cutbush, K.; Andrews, S.; Siddiqui, N.; Brown, L.M.; Ross, M. Capitellar Fractures-Is Open Reduction and Internal Fixation Necessary? J. Orthop. Trauma 2015, 29, 50–53.
- Nauth, A.; McKee, M.D.; Ristevski, B.; Hall, J.; Schemitsch, E.H. Distal Humeral Fractures in Adults. J. Bone Jt. Surg. Am. Vol. 2011, 93, 686–700.
- Lee, J.J.; Lawton, J.N. Coronal Shear Fractures of the Distal Humerus. J. Hand Surg. 2012, 37, 2412–2417.
- Mighell, M.; Virani, N.A.; Shannon, R.; Echols, E.L.; Badman, B.L.; Keating, C.J. Large Coronal Shear Fractures of the Capitellum and Trochlea Treated with Headless Compression Screws. J. Shoulder Elb. Surg. 2010, 19, 38–45.
- Suenghwan, J.; Morrey, B.F. Distal Humerus Fractures: Isolated Fracture of the Capitellum; Elsevier: Amsterdam, The Netherlands, 2017.
- Dushuttle, R.P.; Coyle, M.P.; Zawadsky, J.P.; Bloom, H. Fractures of the Capitellum. J. Trauma 1985, 25, 317–321.
- Fowles, J.V.; Kassab, M.T. Fracture of the Capitulum Humeri. Treatment by Excision. J. Bone Jt. Surg. Am. Vol. 1974, 56, 794–798.
- Dhurve, K.; Patil, V.S.; Chandanwale, A.S.; Puranik, R.G. Isolated Fracture of the Trochlea: Report of Two Cases with Review of the Literature on the Mechanism of Injury; Akshantala Enterprises Private Limited: Mysore, India, 2013.
- Feldman, M.D. Arthroscopic Excision of Type II Capitellar Fractures. Arthrosc. J. Arthrosc. Relat. Surg. 1997, 13, 743–748.
- Hardy, P.; Menguy, F.; Guillot, S. Arthroscopic Treatment of Capitellum Fracture of the Humerus. Arthrosc. J. Arthrosc. Relat. Surg. 2002, 18, 422–426.
- Kuriyama, K.; Kawanishi, Y.; Yamamoto, K. Arthroscopic-Assisted Reduction and Percutaneous Fixation for Coronal Shear Fractures of the Distal Humerus: Report of Two Cases. J. Hand Surg. 2010, 35, 1506–1509.
- Mitani, M.; Nabeshima, Y.; Ozaki, A.; Mori, H.; Issei, N.; Fujii, H.; Fujioka, H.; Doita, M. Arthroscopic Reduction and Percutaneous Cannulated Screw Fixation of a Capitellar Fracture of the Humerus: A Case Report. J. Shoulder Elb. Surg. 2009, 18, e6–e9.
- van Nguyen, T.; Kholinne, E.; AlSomali, K.; Cho, C.H.; Koh, K.H.; Jeon, I.H. Technique for Arthroscopic-Assisted Reduction and Cannulated Screw Fixation for Coronal Shear Fractures of the Distal Humerus. Arthrosc. Tech. 2021, 10, e949–e955.
- Holt, M.S.; Savoie, F.H.; Field, L.D.; Ramsey, J.R. Arthroscopic Management of Elbow Trauma. Hand Clin. 2004, 20, 485–495.
- Kocher, T. Textbook of Operative Surgery, 3rd ed.; Adam & Charles Black: London, UK, 1911.
- Bellato, E.; Castoldi, F.; Marmotti, A.; Greco, V.; Pautasso, A.; Blonna, D. Relationship Between the Lateral Collateral Ligament of the Elbow and the Kocher Approach: A Cadaver Study. J. Hand Surg. 2021, 46, 245.e1–245.e7.
- Ring, D. Open Reduction and Internal Fixation of an Apparent Capitellar Fracture Using an Extended Lateral Exposure. J. Hand Surg. 2009, 34, 739–744.
- Li, J.; Martin, V.T.; Su, Z.-W.; Li, D.-T.; Zhai, Q.-Y.; Yu, B. Lateral Epicondyle Osteotomy Approach for Coronal Shear Fractures of the Distal Humerus: Report of Three Cases and Review of the Literature. World J. Clin. Cases 2021, 9, 4318–4326.
- Imatani, J.; Morito, Y.; Hashizume, H.; Inoue, H. Internal Fixation for Coronal Shear Fracture of the Distal End of the Humerus by the Anterolateral Approach. J. Shoulder Elb. Surg. 2001, 10, 554–556.
- Ravishankar, M.R.; Kumar, M.N.; Raut, R. Choice of Surgical Approach for Capitellar Fractures Based on Pathoanatomy of Fractures: Outcomes of Surgical Management. Eur. J. Orthop. Surg. Traumatol. Orthop. Traumatol. 2017, 27, 233–242.
- Hotchkiss, R.; Kasparyan, G. The Medial “Over the Top” Approach to the Elbow. Tech. Orthop. 2000, 15, 105–112.
- Mighell, M.A.; Harkins, D.; Klein, D.; Schneider, S.; Frankle, M. Technique for Internal Fixation of Capitellum and Lateral Trochlea Fractures. J. Orthop. Trauma 2006, 20, 699–704.
- Wolfson, T.S.; Lowe, D.; Egol, K.A. Capitellum Fracture Open Reduction and Internal Fixation with Headless Screws. J. Orthop. Trauma 2019, 33 (Suppl. 1), S5–S6.
- Matache, B.A.; Culliton, K.; Chang, Y.; Cron, G.O.; Louati, H.; Pollock, J.W. Lateral Trochlear Ridge: A Non-Articulating Zone for Anterior-to-Posterior Screw Placement in Fractures Involving the Capitellum and Trochlea. J. Bone Jt. Surg. Am. Vol. 2019, 101, e75.
- Elkowitz, S.J.; Polatsch, D.B.; Egol, K.A.; Kummer, F.J.; Koval, K.J. Capitellum Fractures: A Biomechanical Evaluation of Three Fixation Methods. J. Orthop. Trauma 2002, 16, 503–506.
- Elkowitz, S.J.; Kubiak, E.N.; Polatsch, D.; Cooper, J.; Kummer, F.J.; Koval, K.J. Comparison of Two Headless Screw Designs for Fixation of Capitellum Fractures. Bul. NYU Hosp. Jt. Dis. 2003, 61, 123.
- Singh, A.P.; Singh, A.P.; Vaishya, R.; Jain, A.; Gulati, D. Fractures of Capitellum: A Review of 14 Cases Treated by Open Reduction and Internal Fixation with Herbert Screws. Int. Orthop. 2010, 34, 897–901.
- Mahirogullari, M.; Kiral, A.; Solakoglu, C.; Pehlivan, O.; Akmaz, I.; Rodop, O. Treatment of Fractures of the Humeral Capitellum Using Herbert Screws. J. Hand Surg. 2006, 31, 320–325.
- Yu, T.; Tao, H.; Xu, F.; Hu, Y.; Zhang, C.; Zhou, G. Management of Isolated Coronal Shear Fractures of the Humeral Capitellum with Herbert Screw Fixation through Anterolateral Approach. BMC Musculoskelet. Disord. 2018, 19, 108.
- Tarallo, L.; Novi, M.; Porcellini, G.; Giorgini, A.; Micheloni, G.; Catani, F. Surgical Tips and Tricks for Coronal Shear Fractures of the Elbow. Arch. Orthop. Trauma Surg. 2021, 141, 261–270.
- Lopiz, Y.; Rodríguez-González, A.; García-Fernández, C.; Marco, F. Open Reduction and Internal Fixation of Coronal Fractures of the Capitellum in Patients Older than 65 Years. J. Shoulder Elb. Surg. 2016, 25, 369–375.
- Wagner, F.C.; Post, A.; Yilmaz, T.; Maier, D.; Neubauer, J.; Feucht, M.J.; Südkamp, N.P.; Reising, K. Biomechanical Comparison of Biodegradable Magnesium Screws and Titanium Screws for Operative Stabilization of Displaced Capitellar Fractures. J. Shoulder Elb. Surg. 2020, 29, 1912–1919.
- Hirvensalo, E.; Böstman, O.; Partio, E.; Törmälä, P.; Rokkanen, P. Fracture of the Humeral Capitellum Fixed with Absorbable Polyglycolide Pins: 1-Year Follow-up of 8 Adults. Acta Orthop. 1993, 64, 85–86.
This entry is offline, you can click here to edit this entry!
