COVID-19 is an inflammatory disease caused by SARS-CoV-2 and can manifest as various symptoms ranging from mild symptoms or asymptomatic cases to severe pneumonia that can progress to acute respiratory distress syndrome (ARDS) and death. The entry describes a study assessed the utility of various inflammatory markers in predicting mortality among hospitalized patients with COVID-19.
- COVID-19
- mortality
- prediction
1. Introduction
COVID-19 has a three-phase progression: initial disease caused by active infection, a second pulmonary phase, and, when severe, a third phase described by hyper-inflammation, cytokine storm, elevated biomarker levels of cardiac injury, and significant morbidity and mortality [10]. Serum biochemical analysis and blood count analysis are commonly used blood tests, which could be faster, easier to use, and low-cost techniques that can facilitate the diagnosis and prognosis of this disease [11]. From these routine tests, inflammatory markers have been used for predicting the severity of COVID-19 such as neutrophil to lymphocyte ratio (NLR), derivate neutrophil to lymphocyte ratio (dNLR), monocyte to lymphocyte ratio (MLR), and platelet to lymphocyte ratio (PLR) [11,12]. NLR and PLR are biomarkers reflecting systemic inflammation, neutrophil and platelet activation, and are associated with increased mortality in cardiovascular disease and poor prognosis in various cancers or in polycythemia vera [13,14,15]. In addition, a higher NLR, and decreased PLR were predictive of poor survival in patients with myelofibrosis [16]. Derived neutrophil-to-lymphocyte ratio (dNLR) is a potential new biomarker for systemic inflammation, defined as the absolute neutrophil count (ANC)/white cell count (WBC)—absolute neutrophil count (ANC), and has prognostic value in patients with several types of cancer [17,18,19]. Unlike NLR, dNLR includes monocytes and other granulocytes by using the difference between WBC and neutrophils in the denominator. Poorly differentiated and immature neutrophils can be released into a pro-inflammatory environment, which rapidly increases neutrophil generation, thus dNLR is likely to reflect this negative inflammation more comprehensively [17,19]. The systemic inflammatory response index (SIRI) may also reflect the host’s immune and inflammatory balance [20]. In addition, systemic immune-inflammation index (SII), defined as platelet count × NLR, is effective in reflecting inflammatory status, being a basic biomarker for predicting the prognosis [12]. The current study assesses the utility of various inflammatory markers in predicting mortality among hospitalized patients with COVID-19.
2. Participants Characteristics
| Total | Survivors 91 (84.3%) |
Deaths 17 (15.7%) |
p Value | |
|---|---|---|---|---|
| Age (Mean ± SD) |
63.31 ± 14.83 | 62.02 ± 14.73 | 70.18 ± 13.83 | 0.03 |
| Comorbidities No. (%) |
||||
| Diabetes | 50 (46.3%) | 40 (44.0%) | 10 (58.8%) | 0.29 |
| Hypertension | 76 (70.4%) | 62 (68.1%) | 14 (82.4%) | 0.38 |
| Heart diseases | 51 (47.2%) | 38 (41.8%) | 13 (76.5%) | 0.01 |
| Chronic lung diseases | 23 (21.3%) | 17 (18.7%) | 6 (35.3%) | 0.19 |
| Complete blood count (Mean ± SD) |
||||
| White blood cell (×1012/L) | 8.71 ± 5.74 | 8.71 ± 5.76 | 8.73 ± 5.81 | 0.98 |
| Neutrophil count (×109/L) | 6.96 ± 4.36 | 6.75 ± 4.18 | 8.06 ± 5.19 | 0.25 |
| Lymphocyte count (×109/L) | 0.98 ± 0.78 | 1.03 ± 0.82 | 0.73 ± 0.44 | 0.03 |
| Monocyte count (×109/L) | 0.47 ± 0.32 | 0.47 ± 0.32 | 0.51 ± 0.33 | 0.64 |
| Hemoglobin (g/dL) |
13.15 ± 1.78 | 13.27 ± 1.64 | 12.50 ± 2.36 | 0.10 |
| Platelet count (×109/L) |
242 ± 109 | 252 ± 112 | 192 ± 79 | 0.03 |
| Inflammatory markers | ||||
| NLR | 9.18 ± 6.7 | 8.31 ± 5.74 | 13.83 ± 9.23 | 0.001 |
| MLR | 0.58 ±0.44 | 0.53 ± 0.39 | 0.83 ± 0.59 | 0.01 |
| PLR | 327 ± 72 | 324 ± 219 | 345 ± 235 | 0.71 |
| dNLR | 5.16 ± 3.76 | 4.77 ± 3.45 | 7.07 ± 4.64 | 0.01 |
| SII | 2280 ± 1950 | 2183 ± 1847 | 2798.± 2429 | 0.23 |
| SIRI | 4.57 ± 5.12 | 4.11 ± 4.67 | 7.02 ± 6.72 | 0.03 |
| O2 Saturation * | 91.96 ± 6.16 | 92.26 ± 5.96 | 90.35 ± 7.13 | 0.24 |
| Hospitalization length | 11.89 (6.56) | 12.96 | 6.18 | <0.001 |
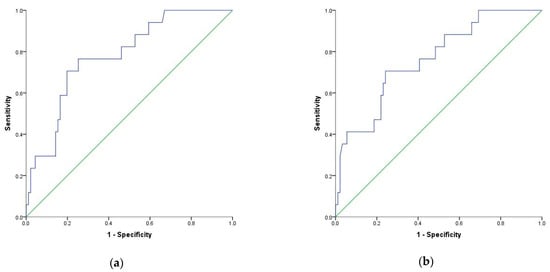
3. Using Optimal Cut-Off Values of Inflammatory Markers to Predict Mortality in Patients with COVID-19
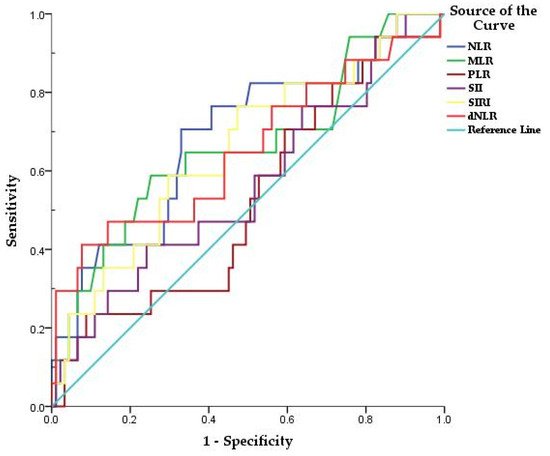
| Variables | Area | Std. Error | Asymptotic Sig. | 95% Confidence Interval |
Sensitivity | Sensibility | Cut-Off | |
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
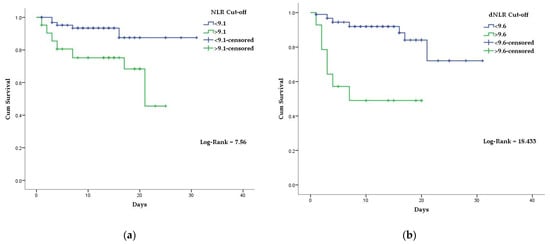
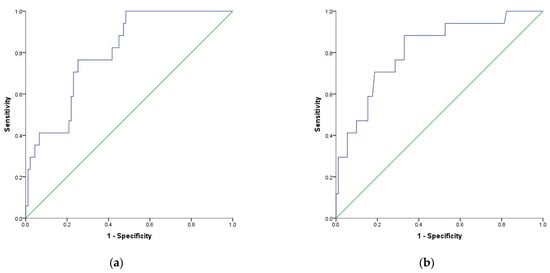
| NLR | 0.689 | 0.074 | 0.014 | 0.544 | 0.833 | 70% | 67% | 9.1 |
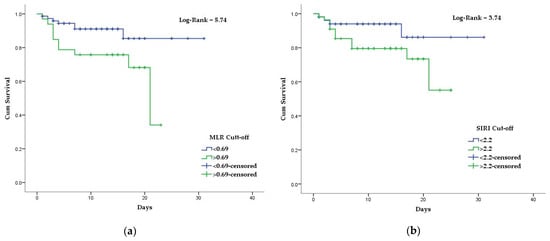
| MLR | 0.661 | 0.078 | 0.036 | 0.508 | 0.813 | 58% | 74% | 0.69 |
| SIRI | 0.655 | 0.074 | 0.042 | 0.511 | 0.800 | 76% | 52% | 2.2 |
| dNLR | 0.652 | 0.082 | 0.047 | 0.491 | 0.813 | 41% | 92% | 9.6 |
4. Association of Inflammatory Biomarkers Results with The COVID-19 Mortality
| Variables | HR (95%CI) | p Value |
|---|---|---|
| NLR | 3.85 (1.35–10.95) | 0.01 |
| dNLR | 6.4 (2.40–17.18) | <0.001 |
| MLR | 3.05 (1.16–8.05) | 0.02 |
| Variables | Adjusted OR * | p Value |
|---|---|---|
| NLR | 4.14 | 0.002 |
| dNLR | 14.09 | 0.001 |
| MLR | 3.29 | 0.04 |
| SIRI | 3.06 | 0.08 |
This entry is adapted from the peer-reviewed paper 10.3390/diagnostics12010122
