Most cardiac studies focus on evaluating left ventricular (LV) systolic function. However, the assessment of diastolic cardiac function is becoming more appreciated, especially with the increasing prevalence of pathologies associated with diastolic dysfunction like heart failure with preserved ejection fraction (HFpEF). Diastolic dysfunction is an indication of abnormal mechanical properties of the myocardium, characterized by slow or delayed myocardial relaxation, abnormal LV distensibility, and/or impaired LV filling.
- heart
- diastolic cardiac function
- MRI
- HFpEF
1. Introduction
| Type of Disease | MRI Technique | n | Principal Findings |
|---|---|---|---|
| HCM [11] | GRE | 31 | Impairment of regional relaxation |
| HCM [12] | Spectroscopy | 8 | Decreased PCr/ATP in symptomatic patients |
| HCM [13] | Spectroscopy | 8 | Decreased PCr/ATP in asymptomatic patients |
| HCM [14] | Tagging | 17 | Smaller circumferential curvatures in hypertrophy |
| AS [15] | Tagging | 12 | Prolonged and delayed untwisting |
| AS [16] | Phase contrast | 9 | Volumetric mitral flow correlates with Doppler |
| LVH [17] | GRE | 9 | Early detection of filling abnormalities |
| AS [18] | Tagging | 13 | Prolonged and delayed untwisting |
| Hypertensive HD [19] | Spectroscopy | 11 | Decreased PCr/ATP correlates with impaired relaxation |
| Previous MI [20] | Phase contrast | 11 | Early diastolic filling velocities correlate with Doppler |
| Previous MI [21] | Tagging | 16 | Reduction of systolic strains in infarcted and remote area |
| Previous MI [22] | Tagging | 18 | Nonuniform, delayed, and prolonged untwisting |
| CAD/previous MI [20] | GRE | 10/15 | Reduced early diastolic long-axis velocity |
| Previous MI [23] | Tagging | 9 | Reduced systolic strains in asynergic segments |
| Fallot [24] | Phase contrast | 19 | Restrictive flow is associated with decreased exercise |
| Mustard/Senning [25] | Phase contrast | 12 | Restrictive tricuspid flow |
| Fallot [26] | GRE | 10 | Impaired ventricular filling correlates with exercise |
| RVPO [14] | Tagging | 9 | Heterogeneity in strain |
| Single ventricle [27] | Tagging | 10 | Regional decrease in systolic strains |
AS, Aortic stenosis; ATP, adenosine triphosphate; CAD, coronary artery disease; GRE, gradient echo; HCM, hypertrophic cardiomyopathy; HD, heart disease; LVH, left ventricular hypertrophy; MI, myocardial infarction; PCr, phosphocreatine; RVPO, right ventricular pressure overload; Spectroscopy, 31P-MR spectroscopy. Table reproduced with permission from [10]. Copyright 2002 Elsevier.
2. Cardiac MRI Techniques
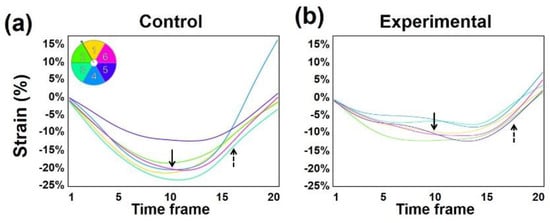
2.1. MRI Tagging
2.2. Complementary Spatial Modulation of Magnetization
2.3. MRI Feature-Tracking
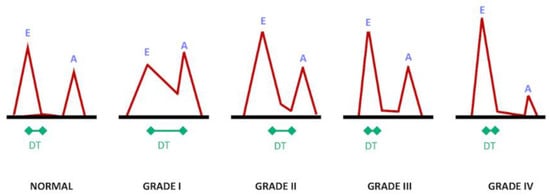
2.4. Phase-Contrast MRI
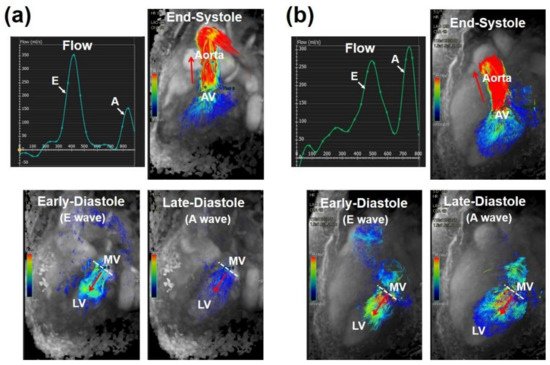
2.5. Four-Dimensional Flow Cardiac MRI (4D-Flow)
3. Cardiovascular Measures
3.1. Temporal Resolution
3.2. Late Diastole
3.3. Untwisting Motion
3.4. Vorticity
3.5. Left Atrium
3.6. Mitral Annulus
This entry is adapted from the peer-reviewed paper 10.3390/tomography7040075
References
- Cheng-Baron, J.; Chow, K.; Khoo, N.S.; Esch, B.T.; Scott, J.M.; Haykowsky, M.J.; Tyberg, J.V.; Thompson, R.B. Measurements of changes in left ventricular volume, strain, and twist during isovolumic relaxation using MRI. Am. J. Physiol. Heart Circ. Physiol. 2010, 298, H1908–H1918.
- Thompson, R.B.; Paterson, I.; Chow, K.; Cheng-Baron, J.; Scott, J.M.; Esch, B.T.; Ennis, D.B.; Haykowsky, M.J. Characterization of the relationship between systolic shear strain and early diastolic shear strain rates: Insights into torsional recoil. Am. J. Physiol. Heart Circ. Physiol. 2010, 299, H898–H907.
- Gaasch, W.H.; Zile, M.R. Left ventricular diastolic dysfunction and diastolic heart failure. Annu. Rev. Med. 2004, 55, 373–394.
- From, A.M.; Scott, C.G.; Chen, H.H. The development of heart failure in patients with diabetes mellitus and pre-clinical diastolic dysfunction a population-based study. J. Am. Coll. Cardiol. 2010, 55, 300–305.
- Dusch, M.N.; Thadani, S.R.; Dhillon, G.S.; Hope, M.D. Diastolic function assessed by cardiac MRI using longitudinal left ventricular fractional shortening. Clin. Imaging 2014, 38, 666–668.
- Steendijk, P. Heart failure with preserved ejection fraction. Diastolic dysfunction, subtle systolic dysfunction, systolic-ventricular and arterial stiffening, or misdiagnosis? Cardiovasc. Res. 2004, 64, 9–11.
- Kawaguchi, M.; Hay, I.; Fetics, B.; Kass, D.A. Combined ventricular systolic and arterial stiffening in patients with heart failure and preserved ejection fraction: Implications for systolic and diastolic reserve limitations. Circulation 2003, 107, 714–720.
- Kermer, J.; Traber, J.; Utz, W.; Hennig, P.; Menza, M.; Jung, B.; Greiser, A.; Barckow, P.; von Knobelsdorff-Brenkenhoff, F.; Topper, A.; et al. Assessment of diastolic dysfunction: Comparison of different cardiovascular magnetic resonance techniques. ESC Heart Fail. 2020, 7, 2637–2649.
- Wu, V.; Chyou, J.Y.; Chung, S.; Bhagavatula, S.; Axel, L. Evaluation of diastolic function by three-dimensional volume tracking of the mitral annulus with cardiovascular magnetic resonance: Comparison with tissue Doppler imaging. J. Cardiovasc. Magn. Reson. 2014, 16, 71.
- Paelinck, B.P.; Lamb, H.J.; Bax, J.J.; Van der Wall, E.E.; de Roos, A. Assessment of diastolic function by cardiovascular magnetic resonance. Am. Heart J. 2002, 144, 198–205.
- Yamanari, H.; Kakishita, M.; Fujimoto, Y.; Hashimoto, K.; Kiyooka, T.; Katayama, Y.; Otsuka, F.; Emori, T.; Uchida, S.; Ohe, T. Effect of regional myocardial perfusion abnormalities on regional myocardial early diastolic function in patients with hypertrophic cardiomyopathy. Heart Vessel. 1997, 12, 192–198.
- De Roos, A.; Doornbos, J.; Luyten, P.R.; Oosterwaal, L.J.; van der Wall, E.E.; den Hollander, J.A. Cardiac metabolism in patients with dilated and hypertrophic cardiomyopathy: Assessment with proton-decoupled P-31 MR spectroscopy. J. Magn. Reson. Imaging 1992, 2, 711–719.
- Jung, W.I.; Sieverding, L.; Breuer, J.; Hoess, T.; Widmaier, S.; Schmidt, O.; Bunse, M.; van Erckelens, F.; Apitz, J.; Lutz, O.; et al. 31P NMR spectroscopy detects metabolic abnormalities in asymptomatic patients with hypertrophic cardiomyopathy. Circulation 1998, 97, 2536–2542.
- Petrank, Y.F.; Dong, S.J.; Tyberg, J.; Sideman, S.; Beyar, R. Regional differences in shape and load in normal and diseased hearts studied by three dimensional tagged magnetic resonance imaging. Int. J. Card. Imaging 1999, 15, 309–321.
- Stuber, M.; Scheidegger, M.B.; Fischer, S.E.; Nagel, E.; Steinemann, F.; Hess, O.M.; Boesiger, P. Alterations in the local myocardial motion pattern in patients suffering from pressure overload due to aortic stenosis. Circulation 1999, 100, 361–368.
- Hartiala, J.J.; Foster, E.; Fujita, N.; Mostbeck, G.H.; Caputo, G.R.; Fazio, G.P.; Winslow, T.; Higgins, C.B. Evaluation of left atrial contribution to left ventricular filling in aortic stenosis by velocity-encoded cine MRI. Am. Heart J. 1994, 127, 593–600.
- Kudelka, A.M.; Turner, D.A.; Liebson, P.R.; Macioch, J.E.; Wang, J.Z.; Barron, J.T. Comparison of cine magnetic resonance imaging and Doppler echocardiography for evaluation of left ventricular diastolic function. Am. J. Cardiol. 1997, 80, 384–386.
- Nagel, E.; Stuber, M.; Burkhard, B.; Fischer, S.E.; Scheidegger, M.B.; Boesiger, P.; Hess, O.M. Cardiac rotation and relaxation in patients with aortic valve stenosis. Eur. Heart J. 2000, 21, 582–589.
- Lamb, H.J.; Beyerbacht, H.P.; van der Laarse, A.; Stoel, B.C.; Doornbos, J.; van der Wall, E.E.; de Roos, A. Diastolic dysfunction in hypertensive heart disease is associated with altered myocardial metabolism. Circulation 1999, 99, 2261–2267.
- Karwatowski, S.P.; Brecker, S.J.; Yang, G.Z.; Firmin, D.N.; St John Sutton, M.; Underwood, S.R. A comparison of left ventricular myocardial velocity in diastole measured by magnetic resonance and left ventricular filling measured by Doppler echocardiography. Eur. Heart J. 1996, 17, 795–802.
- Bogaert, J.; Bosmans, H.; Maes, A.; Suetens, P.; Marchal, G.; Rademakers, F.E. Remote myocardial dysfunction after acute anterior myocardial infarction: Impact of left ventricular shape on regional function: A magnetic resonance myocardial tagging study. J. Am. Coll. Cardiol. 2000, 35, 1525–1534.
- Nagel, E.; Stuber, M.; Lakatos, M.; Scheidegger, M.B.; Boesiger, P.; Hess, O.M. Cardiac rotation and relaxation after anterolateral myocardial infarction. Coron. Artery Dis. 2000, 11, 261–267.
- Garot, J.; Bluemke, D.A.; Osman, N.F.; Rochitte, C.E.; McVeigh, E.R.; Zerhouni, E.A.; Prince, J.L.; Lima, J.A. Fast determination of regional myocardial strain fields from tagged cardiac images using harmonic phase MRI. Circulation 2000, 101, 981–988.
- Helbing, W.A.; Niezen, R.A.; Le Cessie, S.; van der Geest, R.J.; Ottenkamp, J.; de Roos, A. Right ventricular diastolic function in children with pulmonary regurgitation after repair of tetralogy of Fallot: Volumetric evaluation by magnetic resonance velocity mapping. J. Am. Coll. Cardiol. 1996, 28, 1827–1835.
- Rebergen, S.A.; Helbing, W.A.; van der Wall, E.E.; Maliepaard, C.; Chin, J.G.; de Roos, A. MR velocity mapping of tricuspid flow in healthy children and in patients who have undergone Mustard or Senning repair. Radiology 1995, 194, 505–512.
- Singh, G.K.; Greenberg, S.B.; Yap, Y.S.; Delany, D.P.; Keeton, B.R.; Monro, J.L. Right ventricular function and exercise performance late after primary repair of tetralogy of Fallot with the transannular patch in infancy. Am. J. Cardiol. 1998, 81, 1378–1382.
- Fogel, M.A.; Weinberg, P.M.; Gupta, K.B.; Rychik, J.; Hubbard, A.; Hoffman, E.A.; Haselgrove, J. Mechanics of the single left ventricle: A study in ventricular-ventricular interaction II. Circulation 1998, 98, 330–338.
- Young, A.A.; Cowan, B.R.; Thrupp, S.F.; Hedley, W.J.; Dell’Italia, L.J. Left ventricular mass and volume: Fast calculation with guide-point modeling on MR images. Radiology 2000, 216, 597–602.
- Nacif, M.S.; Almeida, A.L.C.; Young, A.A.; Cowan, B.R.; Armstrong, A.C.; Yang, E.; Sibley, C.T.; Hundley, W.G.; Liu, S.; Lima, J.A.; et al. Three-Dimensional Volumetric Assessment of Diastolic Function by Cardiac Magnetic Resonance Imaging: The Multi-Ethnic Study of Atherosclerosis (MESA). Arq. Bras. Cardiol. 2017, 108, 552–563.
- Ibrahim, E.S.H. Heart Mechanics: Magnetic Resonance Imaging; CRC Press: Boca Raton, FL, USA, 2017.
- Edvardsen, T.; Rosen, B.D.; Pan, L.; Jerosch-Herold, M.; Lai, S.; Hundley, W.G.; Sinha, S.; Kronmal, R.A.; Bluemke, D.A.; Lima, J.A. Regional diastolic dysfunction in individuals with left ventricular hypertrophy measured by tagged magnetic resonance imaging—the Multi-Ethnic Study of Atherosclerosis (MESA). Am. Heart J. 2006, 151, 109–114.
- Ambale-Venkatesh, B.; Armstrong, A.C.; Liu, C.Y.; Donekal, S.; Yoneyama, K.; Wu, C.O.; Gomes, A.S.; Hundley, G.W.; Bluemke, D.A.; Lima, J.A. Diastolic function assessed from tagged MRI predicts heart failure and atrial fibrillation over an 8-year follow-up period: The multi-ethnic study of atherosclerosis. Eur. Heart J. Cardiovasc. Imaging 2014, 15, 442–449.
- Fischer, S.E.; McKinnon, G.C.; Maier, S.E.; Boesiger, P. Improved myocardial tagging contrast. Magn. Reson. Med. 1993, 30, 191–200.
- Swoboda, P.P.; Larghat, A.; Zaman, A.; Fairbairn, T.A.; Motwani, M.; Greenwood, J.P.; Plein, S. Reproducibility of myocardial strain and left ventricular twist measured using complementary spatial modulation of magnetization. J. Magn. Reson. Imaging 2014, 39, 887–894.
- Ibrahim, E.S.H. Cardiovascular Magnetic Resonance Tagging for Assessment of Left Ventricular Diastolic Function. In Cardiovascular Magnetic Resonance: A Companion to Braunwald’s Heart Disease, 3rd ed.; Manning, W.J., Pennell, D.J., Eds.; Elsevier: Philadelphia, PA, USA, 2019; pp. 282–290.
- Feinstein, J.A.; Epstein, F.H.; Arai, A.E.; Foo, T.K.; Hartley, M.R.; Balaban, R.S.; Wolff, S.D. Using cardiac phase to order reconstruction (CAPTOR): A method to improve diastolic images. J. Magn. Reson. Imaging 1997, 7, 794–798.
- Ennis, D.B.; Epstein, F.H.; Kellman, P.; Fananapazir, L.; McVeigh, E.R.; Arai, A.E. Assessment of regional systolic and diastolic dysfunction in familial hypertrophic cardiomyopathy using MR tagging. Magn. Reson. Med. 2003, 50, 638–642.
- Uddin, A.; Fairbairn, T.; Swoboda, P.; Kidambi, A.; Motwani, M.; Ripley, D.; Al Musa, T.; McDiarmid, A.; Plein, S.; Greenwood, J. 119 Cardiovascular Magnetic Resonance Evaluation of Change in Myocardial Strain following Transcatheter Aortic Valve Implantation (TAVI) and Surgical Aortic Valve Replacement (SAVR). Heart 2014, 100, A68.
- Ng, M.Y.; Tong, X.; He, J.; Lin, Q.; Luo, L.; Chen, Y.; Shen, X.P.; Wan, E.Y.F.; Yan, A.T.; Yiu, K.H. Feature tracking for assessment of diastolic function by cardiovascular magnetic resonance imaging. Clin. Radiol. 2020, 75, 321.e1–321.e11.
- Buss, S.J.; Krautz, B.; Schnackenburg, B.; Abdel-Aty, H.; Santos, M.F.; Andre, F.; Maertens, M.J.; Mereles, D.; Korosoglou, G.; Giannitsis, E.; et al. Classification of diastolic function with phase-contrast cardiac magnetic resonance imaging: Validation with echocardiography and age-related reference values. Clin. Res. Cardiol. 2014, 103, 441–450.
- Paelinck, B.P.; de Roos, A.; Bax, J.J.; Bosmans, J.M.; van Der Geest, R.J.; Dhondt, D.; Parizel, P.M.; Vrints, C.J.; Lamb, H.J. Feasibility of tissue magnetic resonance imaging: A pilot study in comparison with tissue Doppler imaging and invasive measurement. J. Am. Coll. Cardiol. 2005, 45, 1109–1116.
- Ashrafpoor, G.; Bollache, E.; Redheuil, A.; De Cesare, A.; Giron, A.; Defrance, C.; Azarine, A.; Perdrix, L.; Ladouceur, M.; Diebold, B.; et al. Age-specific changes in left ventricular diastolic function: A velocity-encoded magnetic resonance imaging study. Eur. Radiol. 2015, 25, 1077–1086.
- Eriksson, J.; Bolger, A.F.; Ebbers, T.; Carlhall, C.J. Four-dimensional blood flow-specific markers of LV dysfunction in dilated cardiomyopathy. Eur. Heart J. Cardiovasc. Imaging 2013, 14, 417–424.
- Svalbring, E.; Fredriksson, A.; Eriksson, J.; Dyverfeldt, P.; Ebbers, T.; Bolger, A.F.; Engvall, J.; Carlhall, C.J. Altered Diastolic Flow Patterns and Kinetic Energy in Subtle Left Ventricular Remodeling and Dysfunction Detected by 4D Flow MRI. PLoS ONE 2016, 11, e0161391.
- Zhang, J.; Chen, J.; Cheong, B.; Pednekar, A.; Muthupillai, R. High frame rate cardiac cine MRI for the evaluation of diastolic function and its direct correlation with echocardiography. J. Magn. Reson. Imaging 2019, 50, 1571–1582.
- Ibrahim, E.H. Editorial for Cardiac MRI Reveals Late Diastolic Changes in Left Ventricular Relaxation Patterns During Healthy Aging. J. Magn. Reson. Imaging 2021, 53, 775–776.
- Kuijer, J.P.; Marcus, J.T.; Gotte, M.J.; van Rossum, A.C.; Heethaar, R.M. Three-dimensional myocardial strains at end-systole and during diastole in the left ventricle of normal humans. J. Cardiovasc. Magn. Reson. 2002, 4, 341–351.
- Wang, J.; Khoury, D.S.; Thohan, V.; Torre-Amione, G.; Nagueh, S.F. Global diastolic strain rate for the assessment of left ventricular relaxation and filling pressures. Circulation 2007, 115, 1376–1383.
- Kowallick, J.T.; Lamata, P.; Hussain, S.T.; Kutty, S.; Steinmetz, M.; Sohns, J.M.; Fasshauer, M.; Staab, W.; Unterberg-Buchwald, C.; Bigalke, B.; et al. Quantification of left ventricular torsion and diastolic recoil using cardiovascular magnetic resonance myocardial feature tracking. PLoS ONE 2014, 9, e109164.
- Dorfman, T.A.; Rosen, B.D.; Perhonen, M.A.; Tillery, T.; McColl, R.; Peshock, R.M.; Levine, B.D. Diastolic suction is impaired by bed rest: MRI tagging studies of diastolic untwisting. J. Appl. Physiol. 2008, 104, 1037–1044.
- Matter, C.; Mandinov, L.; Kaufmann, P.; Nagel, E.; Boesiger, P.; Hess, O.M. Function of the residual myocardium after infarct and prognostic significance. Z. Kardiol. 1997, 86, 684–690.
- Schafer, M.; Humphries, S.; Stenmark, K.R.; Kheyfets, V.O.; Buckner, J.K.; Hunter, K.S.; Fenster, B.E. 4D-flow cardiac magnetic resonance-derived vorticity is sensitive marker of left ventricular diastolic dysfunction in patients with mild-to-moderate chronic obstructive pulmonary disease. Eur. Heart J. Cardiovasc. Imaging 2018, 19, 415–424.
- Martinez-Legazpi, P.; Bermejo, J.; Benito, Y.; Yotti, R.; Perez Del Villar, C.; Gonzalez-Mansilla, A.; Barrio, A.; Villacorta, E.; Sanchez, P.L.; Fernandez-Aviles, F.; et al. Contribution of the diastolic vortex ring to left ventricular filling. J. Am. Coll. Cardiol. 2014, 64, 1711–1721.
- Abe, H.; Caracciolo, G.; Kheradvar, A.; Pedrizzetti, G.; Khandheria, B.K.; Narula, J.; Sengupta, P.P. Contrast echocardiography for assessing left ventricular vortex strength in heart failure: A prospective cohort study. Eur. Heart J. Cardiovasc. Imaging 2013, 14, 1049–1060.
- Seemann, F.; Baldassarre, L.A.; Llanos-Chea, F.; Gonzales, R.A.; Grunseich, K.; Hu, C.; Sugeng, L.; Meadows, J.; Heiberg, E.; Peters, D.C. Assessment of diastolic function and atrial remodeling by MRI-validation and correlation with echocardiography and filling pressure. Physiol. Rep. 2018, 6, e13828.
- Aquaro, G.D.; Pizzino, F.; Terrizzi, A.; Carerj, S.; Khandheria, B.K.; Di Bella, G. Diastolic dysfunction evaluated by cardiac magnetic resonance: The value of the combined assessment of atrial and ventricular function. Eur. Radiol. 2019, 29, 1555–1564.
- Morris, D.A.; Gailani, M.; Vaz Perez, A.; Blaschke, F.; Dietz, R.; Haverkamp, W.; Ozcelik, C. Left atrial systolic and diastolic dysfunction in heart failure with normal left ventricular ejection fraction. J. Am. Soc. Echocardiogr. 2011, 24, 651–662.
