Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Health Policy & Services
COVID-19 is an infectious disease caused by the SARS-CoV-2 virus, responsible for an increasing number of cases and deaths. Melatonin has anti-inflammatory, antioxidant, immunomodulatory, and Mpro and MMP9 protein-inhibitory activity. Melatonin prevents SARS-CoV-2 infection, although much remains to be clarified, at high doses, it seems to have a coadjuvant therapeutic effect in the treatment of SARS-CoV-2 infection and melatonin is effective against SARS-CoV-2 infection.
- SARS-CoV-2
- COVID-19
- Melatonin
1. Introduction
The COVID-19 coronavirus pandemic, responsible for the “severe acute respiratory syndrome” SARS-CoV-2, continues to rise around the world.
Approximately 40% to 45% of people infected with this coronavirus remain asymptomatic [5,6], and most of them (about 80%) can recover from the disease without treatment [7]. Therefore, the actual number of COVID-19-infected cases is assumed to be much higher than what has been reported [8,9]. However, the level of antibody seropositivity in the general population is still low [10,11], indicating that most of the world’s population remains susceptible.
Most patients have shown an adequate antibody response after infection [10], and proven reinfection has been rare [12]. Moreover, transfusion of convalescent plasma has been indicated as an effective therapy against COVID-19 infection [13]. This evidence, together with other evidence of various characteristics, recommended initiating the development of vaccines against COVID-19. The genome of this coronavirus contains four main structural proteins: the spike protein (S), membrane (M), envelope (E) and nucleocapsid (N). The main target of the antigenic epitopes of the COVID-19 vaccine are the S protein [14]; the S1 domain, which contains the receptor-binding domain (RBD) for the host cell receptor angiotensin-converting enzyme-2 (ACE2) [15]; the N-terminal domain (NTD), which has been demonstrated as another site with potent neutralizing activity [16,17,18]; the S2 domain, which contains the fusion peptide [19,20].
A total of 63 different vaccines have been registered in clinical studies at different stages, and 170 in pre-clinical studies. Of these, Pfizer-BioNTech’s vaccine is 95% effective, Moderna’s is 94% effective and AstraZeneca-Oxford’s is 59% effective, showing an adequate safety profile [21], without forgetting the reality of some adverse effects, such as thromboembolic phenomena, among others [22,23,24,25].
Nonetheless, vaccines to prevent COVID-19 infection are considered the most promising approach to curb the pandemic. In this regard, different strategies are being studied, including blocking SARS-CoV-2 from binding to human cell receptors, preventing the synthesis and replication of viral ribonucleic acid (RNA), restoring host innate immunity, modulating specific immunity, and suppressing excessive inflammatory responses [26,27,28,29,30,31].
Despite these achievements, the current circumstances arising from the irregular distribution of vaccines, transport and storage problems and the difficulties generated by the so-called “anti-vaccine” groups, mean that we are still far from achieving the desired global herd immunity.
This invites further research to find treatments that are effective, with few side effects and affordability for different economies, as Figure 1 depicts. While these difficulties are being resolved, it is necessary to reduce the morbidity and mortality of this pandemic by using alternative treatments such as melatonin [32]. Among its functions, as Figure 2 depicts, it modulates cell function by activating intracellular signaling pathways and the transcription factors involved in them, and is capable of dampening inflammatory activity, acting as a potent antioxidant, optimizing the functions of the mitochondria, boosting immunity, has the capacity to reduce circulating cytokine levels and inhibits the CD147 signaling pathway, thus preventing SARS-CoV-2 from entering cells [33,34,35,36]. In addition, melatonin is a hormone that is safe to administer even at high doses, with protective effects through peroxyl radical scavenging and glutathione activation [37,38,39,40,41].
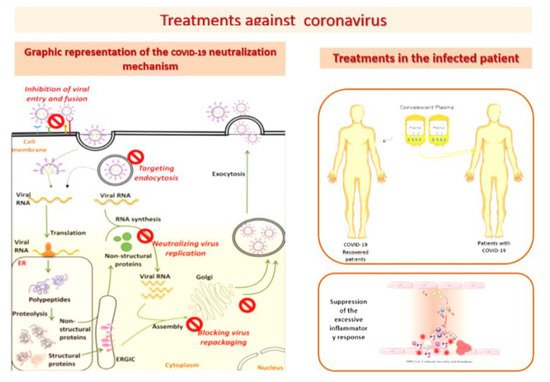
Figure 1. Treatment Against SARS-CoC-2.
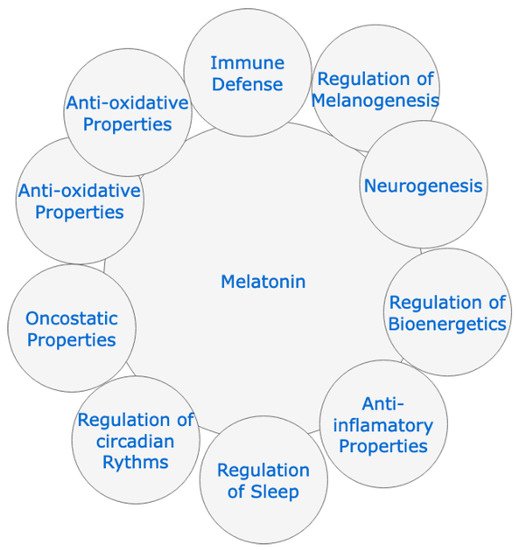
Figure 2. Physiological effects of melatonin.
Doses above 500 mg of melatonin have been shown to be useful in dampening the initial cytokine storm caused by SARS-CoV-2, and this dose is well tolerated in humans. Previously, its usefulness in mitigating the symptomatology and lethality associated with other viral infections, including influenzaviruses and SARS-CoV, and its prophylactic role, particularly in patients with preconditions of suppressed melatonin synthesis, have been noted [32].
Different authors [33,35,36,38,39,41,42,43,44,45] recommend the administration of melatonin for its anti-inflammatory, antioxidant and immunomodulatory capacity, mechanisms that could counteract or dampen the production of the responsible cytokines of the “inflammatory storm” and of the major complications that have been described in the disease caused by SARS-CoV-2.
2. Protective Effect of Melatonin Administration against SARS-CoV-2 Infection
The achievement of vaccines and their gradual administration to the population is transforming the global panorama of this pandemic; however, it is more than likely that, to achieve group immunity at the international level, a period will have to pass. Meanwhile, we will have to continue looking for treatments that help mitigate the damage that is occurring in non-immunized and especially sensitive patients (the elderly, immunosuppressed, sufferers of heart disease, cancer patients, diabetics, the obese, etc.).
As is known in the different protocols that have been applied in the Intensive Care Units to patients infected by SARS-CoV-2 with serious complications, among other therapeutic resources, antivirals and antibiotics from the group of macrolides have been included, as well as corticosteroids, biological therapies and even nonspecific intravenous immunoglobulins in severe cases (without clear evidence of their usefulness at doses of 1g/kg/day for 2 days or 400 mg/kg/day for 5 days), supporting that supportive treatments for basic vitality (ventilatory, cardiocirculatory, homeostatic and renal), together with specific measures (corticosteroids, tocilizumab, etc.), have demonstrated their usefulness and efficacy in numerous critical patients [52,53,54,55,56,57].
Thus, due to the lack of specific and effective active ingredients, there are numerous studies and recommendations that indicate the need for alternative treatments that cover the care and preventive needs of SAR-CoV-2 infection, such as those indicated by Anderson and Reiter [33], who recommend the administration of melatonin for its anti-inflammatory and antioxidant capacity, which leverages to buffer the cytokine storm, reducing the symptoms and lethality of the infection. It is also shown to be safe at high doses and to have a prophylactic effect.
These affirmations are corroborated by the works carried out by Karamitri and Jockers [35], which confirm the antioxidant capacity of melatonin through eliminating peroxyl radicals and activating glutathione, and by Alghamdi [36], which corroborates the anti-inflammatory, immunity-enhancing and reducing activity of the concentration of circulating and inhibitory cytokines of the CD147 pathway. Furthermore, Zhang et al. [41] state that it is highly effective in the elderly and immunosuppressed with problems synthesizing melatonin, undergoing chemotherapy or transplants, or undergoing chronic treatment with corticosteroids.
Brusco L et al. [42] describe that deep sedation performed in the ICU in patients affected by SARS-CoV-2 increases long-term mortality. This indicates that the administration of melatonin reduces the use of sedation, pain, agitation, and anxiety, while it improves the quality of sleep. Furthermore, as a cytoprotective agent, melatonin restores the optimal circadian pattern of the sleep/wake cycle, which improves the clinical condition of the person with SARS-CoV-2 pneumonia. It is concluded in this work that the use of melatonin as adjunctive therapy in ICU patients is recommended, a statement that is supported by the reduction in the length of stay in the ICU. Added to this is its high margin of safety, the possibility of administration by different route—including oral, its stability without refrigeration and its low cost, which makes it accessible to geographic areas that lack specific infrastructures or to countries with limited resources. These are undoubtedly interesting considerations because it is a review of clinical trials, with a medium level of evidence. The mentioned study’s interest is mainly focused on the effects on sleep and a certain cytoprotective capacity, and a dose of 9 mg is proposed, clearly insufficient to achieve other effects in the evolutionary stages of the disease.
On the other hand, Cardinali D et al. [43] focus on the action of melatonin as a powerful chronobiotic with a slight hypnotic capacity, capable of synchronizing circadian rhythms, verifying that the prescription of melatonin two weeks before vaccination against SARS-CoV-2 improves the quality of sleep and guarantees that the vaccination is carried out in optimal conditions, keeping the patient’s mood and response capacity elevated and seroprotection. Added to this is its anxiolytic and antidepressant power, ultimately contributing to the effectiveness of the treatment. These are undoubtedly aspects of great interest, centered on its ability to regulate biological rhythms and, especially, the rhythm of sleep, which is altered in affected patients. In addition, it seems that its immunomodulatory and immune system enhancer role is being demonstrated again, an aspect that had already been previously referred to in the literature, precisely in seroconversion with a clear increase in the “booster” effect [53,54,55,56], as Figure 4 depicts.
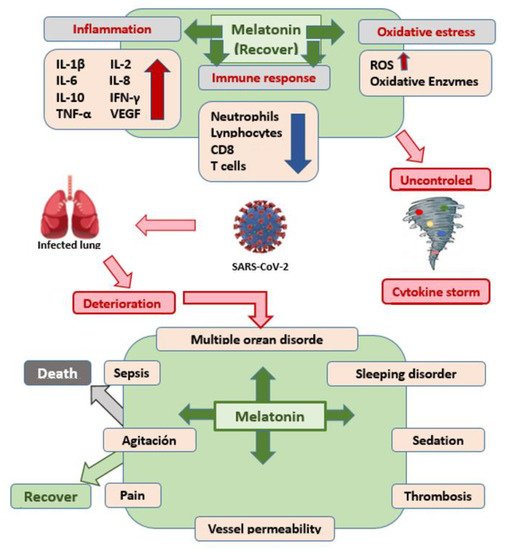
Figure 4. Mechanism of action of melatonin against SARS-CoV-2.
In another interesting contribution [42], the beneficial effects of melatonin as an adjuvant in the treatment of SARS-CoV-2 infection are emphasized, which are related to its anti-inflammatory, antioxidant, and regulatory capacity of the immune response, as it is documented in respiratory disorders, shown in Figure 4.
Reiter RJ et al. [57] once again describe that high mortality is caused by the uncontrolled innate immune response and the intense inflammatory response, and melatonin can be administered as a prophylactic by regulating the innate immune response’s exaggerated and excessive inflammation, promoting adaptive immune activity. These investigators propose the following therapeutic algorithm shown in Figure 5 for its use in patients affected by the pandemic, suggesting administering a dose of 100–400 mg/day as a supplement, especially if effective antiviral treatment is not available:
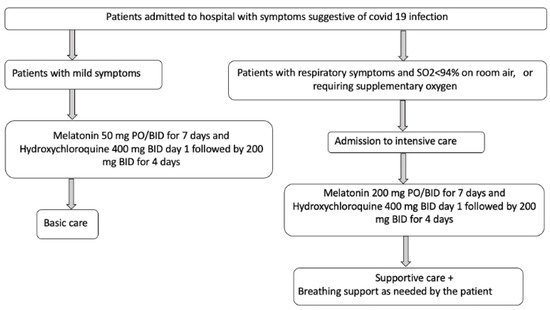
Figure 5. Melatonin administration algorithm against COVID-19. Inspired in Reiter RJ et al. [57].
This seems to be a very appropriate and promising proposal, with pathophysiological grounds. Perhaps the most novel are the regimen and the dose recommended by the authors. It has been published that, for melatonin to enter the mitochondria, minimum doses of 50 mg are necessary, and, in this case, it is more than enough.
Currently, there is no definitive treatment against COVID-19, which makes its development an urgent need due to its serious repercussions. Consequently, Acuña-Castroviejo D et al. [45] propose melatonin as a molecule of great interest in the treatment of COVID-19 for the following reasons: (1) antioxidant function, which reduces the effects of free radicals, restores mitochondrial metabolism, and prevents lung damage; (2) anti-inflammatory function, caused by SARS-CoV-2 infection; (3) inhibitory of p65, preventing the transcriptional capacity and the inflammatory response. In the EducraCT clinical trial: 2008-006782-83, the authors demonstrate that the intravenous administration of 60 mg/day of melatonin improves the condition of patients and reduces their mortality and their hospital stay by up to 40%. To determine the dose to be administered, these authors designed a protocol that was approved by the Spanish Agency for Medicines and Medical Devices in a single-center, double-blind, randomized and placebo-controlled phase II trial, the objective being to address the efficacy and safety of intravenous administration of melatonin in patients admitted to the ICU.
3. Conclusions
Once the contributions selected for this review were analyzed, we believe that the following considerations are relevant:
- (1)
-
Melatonin is a simple molecule, with well-documented pathophysiological functions, such as: the anti-inflammatory, antioxidant, and immunomodulatory action, as well as its inhibitory capacity of the Mpro protease and the MMP9 protein, which would make it a therapeutic alternative to consider against various infectious diseases.
- (2)
-
It has been known for years and it has been demonstrated once again with the administration of vaccines that the administration of melatonin can enhance the immune response, with a response in the rate of specific antibodies much higher than when the vaccine components are administered without melatonin.
- (3)
-
Before the onset of this pandemic, it had been shown in various viral infections that it could inhibit and/or mitigate the pathogenic action of these microbial agents in experimental animals.
- (4)
-
When melatonin is used in the laboratory (animal experimentation) and in the human clinic, a very wide safety margin has been demonstrated, well above most of the drugs used in ICUs against SARS-CoV-2 infection.
- (5)
-
There is a sufficient level of scientific evidence to authorize its use as a preventive drug against COVID-19 infection, due to its proven physiological actions, although it must be said that the exact dose to achieve this preventive effect has still not been determined.
- (6)
-
In infected patients with progressive disease, the scientific evidence is clear, and its administration is recommended for several reasons: (a) because it has been able to significantly reduce the consequences of the disease; (b) because there are no studies that say otherwise; (c) because its security profile is very broad.
- (7)
-
Although several administration guidelines have already been published in patients infected with SARS-CoV-2, it would be advisable to launch new clinical trials to define the best administration protocol, especially regarding dose and times when it should be administered, to respect its circadian rhythmicity.
This entry is adapted from the peer-reviewed paper 10.3390/cimb44010003
This entry is offline, you can click here to edit this entry!
