Delirium is a set of neuropsychiatric symptoms, including qualitative disturbances of consciousness and attention, which may be accompanied by cognitive deficits and psychotic symptoms. The incidence of delirium varies from several percent in patients hospitalized in general wards up to 80% in patients with multi-organ failure treated in intensive care units. Delirium worsens the prognosis, extends hospitalization time, and may increase mortality.
- delirium
- Hypoactive delirium
- hyperactive delirium
1. Introduction
The incidence of delirium varies from several percent in patients hospitalized in general wards up to 80% in patients with multi-organ failure treated in intensive care units (ICU)[1][2]. Hypoactive delirium in the most frequent form, accounting for almost half of all delirium cases and may not be recognized even in 80% of patients, due to the coexistence of dementia or use of sedative drugs, which cannot always be discontinued in the ICU[3][4].
2. Diagnosis Criteria
Diagnosis of postoperative delirium (POD) should be based on updated criteria in the Diagnostic and Statistical Manual of Mental Disorders (DSM)[5]. Although it is a gold standard diagnostic tool, it can be difficult to use even by experienced non-psychiatrists[6]. Therefore, screening for delirium may be more effective when using validated diagnostic scales: Confusion Assessment Method for the Intensive Care Unit (CAM-ICU)[7][8], Intensive Care Delirium Screening Checklist (ICDSC)[9], Delirium Observation Screening (DOS)[10], Neelon and Champagne Confusion Scale (NEECHAM)[11], or others, which have found popularity in scientific research regarding delirium. These methods are summarized in Table 1.
Table 1. Criteria for the diagnosis of delirium in scientific research.
|
Method |
Diagnostic Criteria |
|
DSM-V *[5] |
· Disturbance of consciousness (i.e., reduced clarity of awareness of the environment) reduced ability to focus, sustain, or shift attention. · Change in cognition (e.g., memory deficit, disorientation, language disturbance, perceptual disturbance) that cannot be better accounted for by a preexisting, established, or evolving dementia. · The disturbance develops over a short period of time (usually hours to days) and tends to fluctuate during the course of the day. · Evidence from the history, physical examination, or laboratory findings indicates that the disturbance is caused by a direct physiologic consequence of a general medical condition, an intoxicating substance, medication use, or more than one cause. |
|
If features 1 and 2 and either 3 or 4 are present (CAM +/positive), a diagnosis of delirium is suggested: · Acute onset and fluctuating course (1) · Inattention (2) · Disorganized thinking (3) · Altered level of consciousness (4) |
|
|
ICDSC[9] |
· Altered level of consciousness · Inattention · Disorientation · Hallucinations or delusions · Psychomotor agitation or retardation · Inappropriate speech or mood · Sleep/wake cycle disturbance · Symptom fluctuation |
|
DOS[10] |
· Dozes off during conversation or activities · Is easily distracted by stimuli from the environment · Maintains attention to conversation or action · Does not finish question or answer · Gives answers that do not fit the question · Reacts slowly to instructions · Thinks they are somewhere else · Knows which part of the day it is · Remembers recent events · Is picking, disorderly, restless · Pulls intravenous tubing, feeding tubes, catheters, etc. · Is easily or suddenly emotional · Sees/hears things which are not there Responses are dichotomous (yes/no). Scores ≥ 3 were considered positive delirium screens |
|
DRS[12] |
· Temporal onset (three points) · Perceptual disturbances (three points) · Hallucinations (three points) · Delusions (three points) · Psychomotor (three points) · Cognition (four points) · Physical etiology (two points) · Sleep-wake cycle (four points) · Mood lability (three points) · Fluctuation (four points) Total scores of ≥ 12– diagnosis of delirium |
|
NEECHAM[11] |
· Level of responsiveness-information processing o Attention and alertness (0–4 points) o Verbal and motor response (0–5 points) o Memory and orientation (0–5 points) · Level of behavior o General behavior and posture (0–2 points) o Sensory motor performance (0–4 points) o Verbal responses (0–4 points) · Vital functions o Vital signs (0–2 points) o Oxygen saturation level (0–2 points) o Urinary continence (0–2 points) 0–19 points: moderate to severe confusion 20–24 points: mild or early development of delirium 25–30 points: not confused or normal function |
* Gold standard.
3. Risk factors
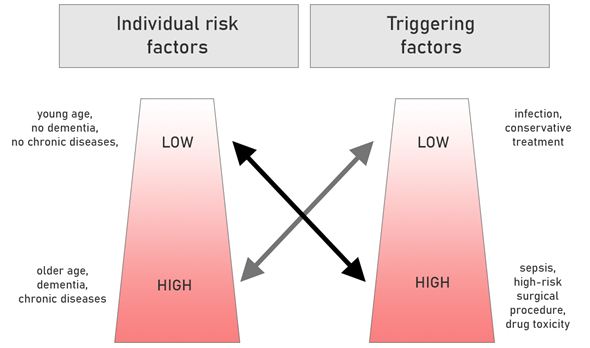
Risk factors for delirium can be divided into predisposing (mainly demographic variables and conditions related to the burden of additional diseases and the degree of their control) and precipitating (triggering) (these are primarily fluctuations in the current clinical state, associated with current hospitalization or therapy). The greater the burden of predisposing factors, the lower the exposure to triggers is likely to cause delirium, and vice versa. Figure 1 illustrates these connotations.
Figure 1. The role of predisposing and triggering factors in the occurrence of delirium. Based on[13][14] (with modification).
This entry is adapted from the peer-reviewed paper 10.3390/ijerph17176069
References
- Leotsakos, I.; Katafigiotis, I.; Gofrit, O.N.; Duvdevani, M.; Mitropoulos, D. Postoperative Delirium after Urological Surgery: A Literature Review. Curr. Urol. 2019, 13, 133–140.
- Brummel, N.E.; Jackson, J.C.; Pandharipande, P.P.; Thompson, J.L.; Shintani, A.K.; Dittus, R.S.; Gill, T.M.; Bernard, G.R.; Ely, E.W.; Girard, T.D. Delirium in the ICU and subsequent long-term disability among survivors of mechanical ventilation. Crit. Care Med. 2014, 42, 369–377.
- Gosch, M.; Nicholas, J.A. Pharmacologic prevention of postoperative delirium. Z. Gerontol. Geriatr. 2014, 47, 105–109.
- Girard, T.D. Sedation, Delirium, and Cognitive Function after Critical Illness. Crit. Care Clin. 2018, 34, 585–598.
- European Delirium Association; American Delirium Society; The DSM-5 criteria, level of arousal and delirium diagnosis: inclusiveness is safer.. BMC Medicine 2014, 12, 141, 10.1186/s12916-014-0141-2.
- Esteban Sepúlveda; José G. Franco; Paula T. Trzepacz; Ana M. Gaviria; David J. Meagher; José Palma; Eva Viñuelas; Imma Grau; Elisabet Vilella; Joan De Pablo; et al. Delirium diagnosis defined by cluster analysis of symptoms versus diagnosis by DSM and ICD criteria: diagnostic accuracy study.. BMC Psychiatry 2016, 16, 167, 10.1186/s12888-016-0878-6.
- Inouye, S.K.; van Dyck, C.H.; Alessi, C.A.; Balkin, S.; Siegal, A.P.; Horwitz, R.I. Clarifying confusion: The confusion assessment method. A new method for detection of delirium. Ann. Intern. Med. 1990, 113, 941–948.
- Ely, E.W.; Margolin, R.; Francis, J.; May, L.; Truman, B.; Dittus, R.; Speroff, T.; Gautam, S.; Bernard, G.R.; Inouye, S.K. Evaluation of delirium in critically ill patients: Validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Crit. Care Med. 2001, 29, 1370–1379.
- Finn M. Radtke; Martin Franck; Stefan Oppermann; Alawi Luetz; Matthes Seeling; Anja Heymann; Robin Kleinwächter; Felix Kork; Yoanna Skrobik; Claudia Spies; et al. Die Intensive Care Delirium Screening Checklist (ICDSC) – Richtlinienkonforme Übersetzung und Validierung einer intensivmedizinischen Delirium–Checkliste. AINS - Anästhesiologie · Intensivmedizin · Notfallmedizin · Schmerztherapie 2009, 44, 80-86, 10.1055/s-0029-1202647.
- Katherine Gavinski; Ryan M. Carnahan; Michelle T. Weckmann; Validation of the delirium observation screening scale in a hospitalized older population.. Journal of Hospital Medicine 2016, 11, 494-497, 10.1002/jhm.2580.
- Liesbeth A Gemert Van; Marieke J Schuurmans; The Neecham Confusion Scale and the Delirium Observation Screening Scale: Capacity to discriminate and ease of use in clinical practice. BMC Nursing 2007, 6, 3-3, 10.1186/1472-6955-6-3.
- P.T. Trzepacz; M.A. Dew; Further analyses of the Delirium Rating Scale. General Hospital Psychiatry 1995, 17, 75-79, 10.1016/0163-8343(94)00095-u.
- Inouye, S.K.; Charpentier, P.A. Precipitating factors for delirium in hospitalized elderly persons. Predictive model and interrelationship with baseline vulnerability. JAMA 1996, 275, 852–857.
- Han, J.H.; Wilber, S.T. Altered mental status in older patients in the emergency department. Clin. Geriatr. Med. 2013, 29, 101–136.