Coronavirus disease 2019 (COVID-19) outbreak was first reported in Wuhan, China in December 2019, and was found to be caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) which is a novel pleomorphic, positive-stranded RNA virus belonging to the Coronaviridae family. Quickly, it has become a global pandemic, infecting more than 176 million people and causing the death of more than 3.8 million individuals, that we are yet to recover from. Thus, an ongoing quest is being carried out for prophylaxis/therapy to prevent the transition from infection into serious forms of COVID-19.
- coronavirus disease 2019 (COVID-19)
- SARS-CoV-2
- vaccine
- coronaviruses
- reinfection
- epidemiology
- spike protein
- ACE2 receptor
- antigenicity
- immunity
1. Introduction
Coronavirus disease 2019 (COVID-19) outbreak was first reported in Wuhan, China in December 2019, and was found to be caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) which is a novel pleomorphic, positive-stranded RNA virus belonging to the Coronaviridae family. Quickly, it has become a global pandemic, infecting more than 176 million people and causing the death of more than 3.8 million individuals, that we are yet to recover from. Thus, an ongoing quest is being carried out for prophylaxis/therapy to prevent the transition from infection into serious forms of COVID-19 [1]. Though measures like physical distancing, use of masks, frequent sterilization, repurposing of existing drugs, etc. are being undertaken, the development of herd immunity through vaccination seems to be the most instrumental measure.
Many therapeutic strategies which can prove useful in the management of COVID-19 disease are underway, such as blocking the virus from binding cell receptors, preventing synthesis and replication of viral RNA, restoring innate immunity, modulating specific receptors/enzymes of the host, etc. [2][3][4][5]. However, amongst all such strategies to control the pandemic, the role of vaccines in preventing coronavirus (CoV) disease has been regarded as the most promising approach. The viral genome encodes several non-structural and structural proteins which include the spike (S), envelope (E), membrane (M), and nucleocapsid (N) proteins, which may play potentially instrumental roles to develop antigenic responses against the virus [6].
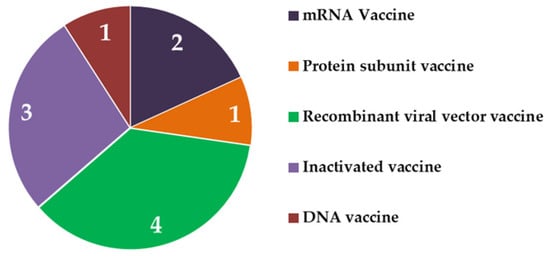
Scientists worldwide are in a race to develop safe and efficacious vaccine candidates against SARS-CoV-2 to curb the pandemic of COVID-19. Overwhelming attention has been paid to the S protein of the virus. The S protein makes up the studs outside the virus and is responsible for viral anchoring onto human cells through interaction with angiotensin-converting enzyme 2 (ACE2) receptors [1]. Hence, a vaccine expressing the S protein should induce a protective immune response without exposure to the whole virus in killed or attenuated form, i.e., the S protein itself is capable enough to act as the target antigen. Newer platforms use only the genetic material coding for S protein. Viral vectors with altered genetic payload (weakened viruses carrying sequences for the antigenic S protein) are also among the frontrunners in the race. Previously none of the adenovirus vectors, DNA vaccines, and mRNA vaccines had been approved by USFDA but the current pandemic has changed the trend. Other candidates in the race for vaccines include protein subunit vaccines and whole virus vaccines, some of which have displayed very promising results.
As of 28 October 2021, 49.10% of the global population has received at least one dose of COVID-19 vaccine, out of which 38.05% have been fully vaccinated [7]. Perturbations have been raised for the vaccines especially regarding their efficacy and the possibility of SARS-CoV-2 reinfection after being vaccinated. Mutation of an RNA virus is a matter of grave concern as it gives rise to newer strains, posing apprehensions that a vaccine developed for one strain might not be effective against a mutated strain. So far, several variants, such as B.1.1.7 (alpha, originated in the UK), B.1.351 (beta, originated in South Africa), P.1 (gamma, originated in Brazil), and B.1.617.2 (delta, originating from India) have been identified as major concerns [8][9]. These new mutants can spread faster, which raises the question of whether they may reduce the effectiveness of approved vaccines. World Health Organization (WHO) categorized variants C.37 (lambda, originated in Peru) and B.1.621 (mu, originated in Colombia) are of interest in this context [8]. Several other variants (B.1.466.2, B.1.525, B.1.526, B.1.617.1, B.1.619, B.1.620, B.1.630, B.1.1.318, C.36.3, R1, etc.) are still under monitoring [8]. In this review, we provided insights into the epidemiology, mechanism of action, and propensity for reinfection with CoV for the different vaccines administered worldwide.
2. Vaccines Approved for Public Use
2.1. Vaccines Approved by WHO for Global Application
| S. No. | Vaccines | Types | Carriers | Doses |
|---|---|---|---|---|
| 1 | Oxford-AstraZeneca (ChAdOx1nCoV-19, AZD1222) (University of Oxford, Oxford, UK) |
Viral vector, targeted towards S protein |
Modified Chimpanzee Adenovirus ChAdOx1 | 2 doses 8 to 12 weeks apart, i.m. |
| 2 | Pfizer-BioNTech (BNT162b2) | Nucleoside modified mRNA |
Lipid nanoparticles | 2 doses 21 to 28 days apart, i.m. |
| 3 | Johnson and Johnson (Ad26.COV2.S, Janssen) | S protein of SARS-CoV-2 WA1/2020 strain | Recombinant, replication incompetent adenovirus Ad26 | Single dose, i.m. |
| 4 | Moderna (mRNA-1273) | Nucleoside modified mRNA |
Lipid nanoparticles | 2 doses, 4 to 6 weeks apart, i.m. |
| 5 | Sinopharm (BBIBP-CorV) | Inactivated virus (2019-CoV) | Inactivated virus + adjuvant |
2 doses, 3–4 weeks apart, i.m. |
| 6 | CoronaVac (Sinovac) | Inactivated virus | Inactivated virus + adjuvant |
2 doses, 2–4 weeks apart, i.m. |
2.1.1. Pfizer-BioNTech (mRNA Vaccine)
2.1.2. Astrazeneca/University of Oxford (Viral Vector Vaccine)
2.1.3. Johnson and Johnson (Viral Vector Vaccine)
2.1.4. Moderna (mRNA Vaccine)
2.1.5. Sinopharm (Inactivated Virus Vaccine)
2.1.6. Sinovac Biotech (Inactivated Virus Vaccine)
2.2. Vaccines Approved Regionally
2.2.1. Sputnik V (Viral Vector Vaccine)
2.2.2. EpiVacCorona (Protein Subunit Vaccine)
2.2.3. Bharat Biotech (Inactivated Virus Vaccine)
2.2.4. Cansino Biologics (Viral Vector Vaccine)
2.2.5. Zydus Cadila (Plasmid-DNA Vaccine)
This entry is adapted from the peer-reviewed paper 10.3390/biomedicines9111740
References
- Kalra, R.S.; Tomar, D.; Meena, A.S.; Kandimalla, R. SARS-CoV-2, ACE2, and Hydroxychloroquine: Cardiovascular Complications, Therapeutics, and Clinical Readouts in the Current Settings. Pathogens 2020, 9, 546.
- Kandimalla, R.; Dewanjee, S.; Kalra, R.S.; Valupadas, C.; Vallamkondu, J.; Kolli, V.; Reddy, P.A.; Reddy, P.H. COVID-19 and Rheumatoid Arthritis Crosstalk: Emerging association, therapeutic options, and challenges. OSF Preprints 2021.
- Kalra, R.S.; Kandimalla, R. Engaging the spikes: Heparan sulfate facilitates SARS-CoV-2 spike protein binding to ACE2 and potentiates viral infection. Signal Transduct. Target. Ther. 2021, 6, 39.
- Dhanjal, J.K.; Kumar, V.; Garg, S.; Subramani, C.; Agarwal, S.; Wang, J.; Zhang, H.; Kaul, A.; Kalra, R.S.; Kaul, S.C.; et al. Molecular mechanism of anti-SARS-CoV2 activity of Ashwagandha-derived withanolides. Int. J. Biol. Macromol. 2021, 184, 297–312.
- Kalra, R.S.; Kumar, V.; Dhanjal, J.K.; Garg, S.; Li, X.; Kaul, S.C.; Sundar, D.; Wadhwa, R. COVID19-inhibitory activity of withanolides involves targeting of the host cell surface receptor ACE2: Insights from computational and biochemical assays. J. Biomol. Struct. Dyn. 2021, 1–14.
- Asselah, T.; Durantel, D.; Pasmant, E.; Lau, G.; Schinazi, R.F. COVID-19: Discovery, diagnostics and drug development. J. Hepatol. 2020, 74, 168–184.
- Our World Data. Coronavirus (COVID-19) Vaccinations. Available online: https://ourworldindata.org/covid-vaccinations; (accessed on 29 October 2021).
- WHO. Tracking-SARS-CoV-2-Variants. Available online: https://www.who.int/en/activities/tracking-SARS-CoV-2-variants; (accessed on 25 October 2021).
- Matta, S.; Rajpal, S.; Chopra, K.; Arora, V. COVID-19 vaccines and new mutant strains impacting the pandemic. Indian J. Tuberc. 2021, 68, 171–173.
- WHO. The Pfizer BioNTech (BNT162b2) COVID-19 Vaccine: What You Need to Know. 2021. Available online: https://www.who.int/news-room/feature-stories/detail/who-can-take-the-pfizer-biontech-covid-19--vaccine (accessed on 9 September 2021).
- Lustig, Y.; Sapir, E.; Regev-Yochay, G.; Cohen, C.; Fluss, R.; Olmer, L.; Indenbaum, V.; Mandelboim, M.; Doolman, R.; Amit, S.; et al. BNT162b2 COVID-19 vaccine and correlates of humoral immune responses and dynamics: A prospective, single-centre, longitudinal cohort study in health-care workers. Lancet Respir. Med. 2021, 9, 999–1009.
- Salvagno, G.L.; Henry, B.M.; Pighi, L.; De Nitto, S.; Gianfilippi, G.L.; Lippi, G. Three-month analysis of total humoral response to Pfizer BNT162b2 mRNA COVID-19 vaccination in healthcare workers. J. Infect. 2021, 83, e4–e5.
- Pfizer and BioNTech Provide Update on Booster Program in Light of the Delta-Variant New York and Mainz, Germany. Available online: https://cdn.pfizer.com/pfizercom/2021-07/Delta_Variant_Study_Press_Statement_Final_7.8.21.pdf (accessed on 28 August 2021).
- Prendecki, M.; Clarke, C.; Brown, J.; Cox, A.; Gleeson, S.; Guckian, M.; Randell, P.; Pria, A.D.; Lightstone, L.; Xu, X.-N.; et al. Effect of previous SARS-CoV-2 infection on humoral and T-cell responses to single-dose BNT162b2 vaccine. Lancet 2021, 397, 1178–1181.
- Zimmermann, P.; Curtis, N. Factors That Influence the Immune Response to Vaccination. Clin. Microbiol. Rev. 2019, 32, e00084-18.
- Connors, M.; Graham, B.S.; Lane, H.C.; Fauci, A.S. SARS-CoV-2 Vaccines: Much Accomplished, Much to Learn. Ann. Intern. Med. 2021, 174, 687–690.
- Kaur, S.P.; Gupta, V. COVID-19 Vaccine: A comprehensive status report. Virus Res. 2020, 288, 198114.
- Angeli, F.; Spanevello, A.; Reboldi, G.; Visca, D.; Verdecchia, P. SARS-CoV-2 vaccines: Lights and shadows. Eur. J. Intern. Med. 2021, 88, 1–8.
- Wise, J. COVID-19: New data on Oxford AstraZeneca vaccine backs 12 week dosing interval. BMJ 2021, 372, n326.
- Voysey, M.; Clemens, S.A.C.; Madhi, S.A.; Weckx, L.Y.; Folegatti, P.M.; Aley, P.K.; Angus, B.; Baillie, V.L.; Barnabas, S.L.; Bhorat, Q.E.; et al. Single-dose administration and the influence of the timing of the booster dose on immunogenicity and efficacy of ChAdOx1 nCoV-19 (AZD1222) vaccine: A pooled analysis of four randomised trials. Lancet 2021, 397, 881–891.
- Mahase, E. COVID-19: South Africa pauses use of Oxford vaccine after study casts doubt on efficacy against variant. BMJ 2021, 372, n372.
- Lumley, S.F.; Rodger, G.; Constantinides, B.; Sanderson, N.; Chau, K.K.; Street, T.L.; O’Donnell, D.; Howarth, A.; Hatch, S.B.; Marsden, B.D.; et al. An Observational Cohort Study on the Incidence of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection and B.1.1.7 Variant Infection in Healthcare Workers by Antibody and Vaccination Status. Clin. Infect. Dis. 2021, ciab608.
- WHO. The Janssen Ad26.COV2.S COVID-19 Vaccine: What You Need to Know. 2021. Available online: https://www.who.int/news-room/feature-stories/detail/the-j-j-covid-19-vaccine-what-you-need-to-know (accessed on 11 September 2021).
- Bos, R.; Rutten, L.; van der Lubbe, J.E.M.; Bakkers, M.J.G.; Hardenberg, G.; Wegmann, F.; Zuijdgeest, D.; de Wilde, A.H.; Koornneef, A.; Verwilligen, A.; et al. Ad26 vector-based COVID-19 vaccine encoding a prefusion-stabilized SARS-CoV-2 Spike immunogen induces potent humoral and cellular immune responses. NPJ Vaccines 2020, 5, 1–11.
- Mukhopadhyay, L.; Yadav, P.D.; Gupta, N.; Mohandas, S.; Patil, D.Y.; Shete-Aich, A.; Panda, S.; Bhargava, B. Comparison of the immunogenicity & protective efficacy of various SARS-CoV-2 vaccine candidates in non-human primates. Indian J. Med. Res. 2021, 153, 93–114.
- Mercado, N.B.; Zahn, R.; Wegmann, F.; Loos, C.; Chandrashekar, A.; Yu, J.; Liu, J.; Peter, L.; McMahan, K.; Tostanoski, L.H.; et al. Single-shot Ad26 vaccine protects against SARS-CoV-2 in rhesus macaques. Nat. Cell Biol. 2020, 586, 1–11.
- van der Lubbe, J.E.M.; Huber, S.K.R.; Vijayan, A.; Dekking, L.; van Huizen, E.; Vreugdenhil, J.; Choi, Y.; Baert, M.R.M.; Boer, K.F.-D.; Gil, A.I.; et al. Ad26.COV2.S protects Syrian hamsters against G614 spike variant SARS-CoV-2 and does not enhance respiratory disease. NPJ Vaccines 2021, 6, 39.
- He, X.; Chandrashekar, A.; Zahn, R.; Wegmann, F.; Yu, J.; Mercado, N.B.; McMahan, K.; Martinot, A.J.; Piedra-Mora, C.; Beecy, S.; et al. Low-dose Ad26.COV2.S protection against SARS-CoV-2 challenge in rhesus macaques. Cell 2021, 184, 3467–3473.e11.
- Oliver, S.E.; Gargano, J.W.; Marin, M.; Wallace, M.; Curran, K.G.; Chamberland, M.; McClung, N.; Campos-Outcalt, D.; Morgan, R.L.; Mbaeyi, S.; et al. The Advisory Committee on Immunization Practices’ Interim Recommendation for Use of Moderna COVID-19 Vaccine—United States, December 2020. MMWR. Morb. Mortal. Wkly. Rep. 2021, 69, 1653–1656.
- Sharma, O.; Sultan, A.A.; Ding, H.; Triggle, C.R. A Review of the Progress and Challenges of Developing a Vaccine for COVID-19. Front. Immunol. 2020, 11, 585354.
- Baden, L.R.; El Sahly, H.M.; Essink, B.; Kotloff, K.; Frey, S.; Novak, R.; Diemert, D.; Spector, S.A.; Rouphael, N.; Creech, C.B.; et al. Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine. N. Engl. J. Med. 2021, 384, 403–416.
- Mahase, E. COVID-19: Moderna vaccine is nearly 95% effective, trial involving high risk and elderly people shows. BMJ 2020, 371, m4471.
- Corbett, K.S.; Flynn, B.; Foulds, K.E.; Francica, J.R.; Boyoglu-Barnum, S.; Werner, A.P.; Flach, B.; O’Connell, S.; Bock, K.W.; Minai, M.; et al. Evaluation of the mRNA-1273 Vaccine against SARS-CoV-2 in Nonhuman Primates. N. Engl. J. Med. 2020, 383, 1544–1555.
- Corbett, K.S.; Edwards, D.K.; Leist, S.R.; Abiona, O.M.; Boyoglu-Barnum, S.; Gillespie, R.A.; Himansu, S.; Schäfer, A.; Ziwawo, C.T.; DiPiazza, A.T.; et al. SARS-CoV-2 mRNA vaccine design enabled by prototype pathogen preparedness. Nature 2020, 586, 567–571.
- WHO. The Sinovac-CoronaVac COVID-19 Vaccine: What You Need to Know. 2021. Available online: https://www.who.int/news-room/feature-stories/detail/the-sinovac-covid-19-vaccine-what-you-need-to-know (accessed on 9 September 2021).
- U.S. National Institutes of Health. ClinicalTrials.gov Efficacy, Immunogenicity and Safety of BBIBP-CorV Vaccine against Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection. (ECOVA-01). Official Title: A Phase 3, Ran-domized, Observer-blind, Controlled Trial to Assess the Efficacy, Immunogenicity and Safety of BBIBP-CorV Vaccine Against Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection. Identifier: NCT04984408. Available online: https://clinicaltrials.gov/ct2/show/NCT04984408 (accessed on 30 August 2021).
- BBIBP-CorV, Sinopharm COVID-19 Vaccine. New Drug Approvals. 2021. Available online: https://newdrugapprovals.org/2021/03/23/bbibp-corv-sinopharm-covid-19-vaccine/ (accessed on 1 September 2021).
- Wang, H.; Zhang, Y.; Huang, B.; Deng, W.; Quan, Y.; Wang, W.; Xu, W.; Zhao, Y.; Li, N.; Zhang, J.; et al. Development of an Inactivated Vaccine Candidate, BBIBP-CorV, with Potent Protection against SARS-CoV-2. Cell 2020, 182, 713–721.e9.
- Palacios, R.; Batista, A.P.; Albuquerque, C.S.N.; Patiño, E.G.; Santos, J.D.P. Efficacy and Safety of a COVID-19 Inactivated Vaccine in Healthcare Professionals in Brazil: The PROFISCOV Study. SSRN 2021, 66.
- Zhang, Y.; Zeng, G.; Pan, H.; Li, C.; Hu, Y.; Chu, K.; Han, W.; Chen, Z.; Tang, R.; Yin, W.; et al. Safety, tolerability, and immunogenicity of an inactivated SARS-CoV-2 vaccine in healthy adults aged 18–59 years: A randomised, double-blind, placebo-controlled, phase 1/2 clinical trial. Lancet Infect. Dis. 2020, 21, 181–192.
- Logunov, D.Y.; Dolzhikova, I.V.; Shcheblyakov, D.V.; Tukhvatulin, A.I.; Zubkova, O.V.; Dzharullaeva, A.S.; Kovyrshina, A.V.; Lubenets, N.L.; Grousova, D.M.; Erokhova, A.S.; et al. Safety and efficacy of an rAd26 and rAd5 vector-based heterologous prime-boost COVID-19 vaccine: An interim analysis of a randomised controlled phase 3 trial in Russia. Lancet 2021, 397, 671–681.
- Barouch, D.H.; Kik, S.V.; Weverling, G.J.; Dilan, R.; King, S.L.; Maxfield, L.F.; Clark, S.; Ng’Ang’A, D.; Brandariz, K.L.; Abbink, P.; et al. International seroepidemiology of adenovirus serotypes 5, 26, 35, and 48 in pediatric and adult populations. Vaccine 2011, 29, 5203–5209.
- Jones, I.; Roy, P. Sputnik V COVID-19 vaccine candidate appears safe and effective. Lancet 2021, 397, 642–643.
- Lawton, G. Sputnik V vaccine goes global. New Sci. 2021, 250, 10–11.
- Balakrishnan, V.S. The arrival of Sputnik V. Lancet Infect. Dis. 2020, 20, 1128.
- Burki, T.K. The Russian vaccine for COVID-19. Lancet Respir. Med. 2020, 8, e85–e86.
- Logunov, D.Y.; Dolzhikova, I.V.; Zubkova, O.V.; Tukhvatullin, A.I.; Shcheblyakov, D.V.; Dzharullaeva, A.S.; Grousova, D.M.; Erokhova, A.S.; Kovyrshina, A.V.; Botikov, A.G.; et al. Safety and immunogenicity of an rAd26 and rAd5 vector-based heterologous prime-boost COVID-19 vaccine in two formulations: Two open, non-randomised phase 1/2 studies from Russia. Lancet 2020, 396, 887–897.
- Günl, F.; Mecate-Zambrano, A.; Rehländer, S.; Hinse, S.; Ludwig, S.; Brunotte, L. Shooting at a Moving Target—Effectiveness and Emerging Challenges for SARS-CoV-2 Vaccine Development. Vaccines 2021, 9, 1052.
- Ryzhikov, A.B.; Ryzhikov, E.A.; Bogryantseva, M.P.; Danilenko, E.D.; Imatdinov, I.R.; Nechaeva, E.A.; Pyankov, O.V.; Pyankova, O.G.; Susloparov, I.M.; Taranov, O.S.; et al. Immunogenicity and protectivity of the peptide vaccine against SARS-CoV-2. Ann. Russ. Acad. Med Sci. 2021, 76, 5–19.
- U.S. National Institutes of Health. ClinicalTrials.gov Study of the Tolerability, Safety, Immunogenicity and Preventive Efficacy of the EpiVacCorona Vaccine for the Prevention of COVID-19. Official Title: Multicenter Double-blind Place-bo-controlled Comparative Randomized Study of the Tolerability, Safety, Immunogenicity and Prophylactic Efficacy of the EpiVacCorona Peptide Antigen-Based Vaccine for the Prevention of COVID-19, with the Participation of 3000 Volunteers Aged 18 Years and above (Phase III-IV). Identifier: NCT04780035. Available online: https://clinicaltrials.gov/ct2/show/NCT04780035 (accessed on 30 August 2021).
- U.S. National Institutes of Health. ClinicalTrials.gov Study of the Safety, Reactogenicity and Immunogenicity of “EpiVac-Corona” Vaccine for the Prevention of COVID-19 (EpiVacCorona). Official Title: Simple, Blind, Placebo-controlled, Ran-domized Study of the Safety, Reactogenicity and Immunogenicity of Vaccine Based on Peptide Antigens for the Prevention of COVID-19 (EpiVacCorona), in Volunteers Aged 18-60 Years (I–II Phase). Identifier: NCT04527575. Available online: https://clinicaltrials.gov/ct2/show/NCT04527575 (accessed on 10 September 2021).
- Thiagarajan, K. What do we know about India’s Covaxin vaccine? BMJ 2021, 373, n997.
- Ganneru, B.; Jogdand, H.; Dharam, V.K.; Molugu, N.R.; Prasad, S.D.; Vellimudu, S.; Ella, K.M.; Ravikrishnan, R.; Awasthi, A.; Jose, J.; et al. Evaluation of Safety and Immunogenicity of an Adjuvanted, TH-1 Skewed, Whole Virion Inactivat-edSARS-CoV-2 Vaccine—BBV152. bioRxiv 2020.
- Peshimam, G.N.; Farooq, U. CanSinoBIO’s COVID-19 Vaccine 65.7% Effective in Global Trials, Pakistan Official Says; Reuters Healthcare & Pharma, 8 February 2021. Available online: https://www.google.com.hk/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&ved=2ahUKEwjs7qb1o4r0AhUEr1YBHe2SDfwQFnoECAUQAQ&url=https%3A%2F%2Fwww.reuters.com%2Fworld%2Fchina%2Fcansinobios-covid-19-vaccine-657-effective-global-trials-pakistan-official-says-2021-02-08%2F&usg=AOvVaw2AqQ6u2XzqSkUjADK166Te (accessed on 10 September 2021).
- Wu, S.; Zhong, G.; Zhang, J.; Shuai, L.; Zhang, Z.; Wen, Z.; Wang, B.; Zhao, Z.; Song, X.; Chen, Y.; et al. A single dose of an adenovirus-vectored vaccine provides protection against SARS-CoV-2 challenge. Nat. Commun. 2020, 11, 4081.
- Kumar, V.M.; Pandi-Perumal, S.R.; Trakht, I.; Thyagarajan, S.P. Strategy for COVID-19 vaccination in India: The country with the second highest population and number of cases. NPJ Vaccines 2021, 6, 60.
- ZyCoV-D Continues India’s Habit of Approving COVID Vaccines with Invisible Data. Available online: https://science.thewire.in/health/zydus-cadila-zycov-d-dna-plasmid-covid-vaccine-missing-data-dcgi-approval/ (accessed on 12 August 2021).
- Dey, A.; Rajanathan, T.C.; Chandra, H.; Pericherla, H.P.; Kumar, S.; Choonia, H.S.; Bajpai, M.; Singh, A.K.; Sinha, A.; Saini, G.; et al. Immunogenic potential of DNA vaccine candidate, ZyCoV-D against SARS-CoV-2 in animal models. Vaccine 2021, 39, 4108–4116.
- Yadav, P.; Kumar, S.; Agarwal, K.; Jain, M.; Patil, D.; Maithal, K.; Mathapati, B.; Giri, S.; Mohandas, S.; Shete, A. Assessment of immunogenicity and protective efficacy of ZyCoV-D DNA vaccine candidates in Rhesus macaques against SARS-CoV-2 in-fection. BioRxiv 2021.
- Momin, T.; Kansagra, K.; Patel, H.; Sharma, S.; Sharma, B.; Patel, J.; Mittal, R.; Sanmukhani, J.; Maithal, K.; Dey, A.; et al. Safety and Immunogenicity of a DNA SARS-CoV-2 vaccine (ZyCoV-D): Results of an open-label, non-randomized phase I part of phase I/II clinical study by intradermal route in healthy subjects in India. EClinicalMedicine 2021, 38, 101020.
