Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Virology
The three encephalitic alphaviruses, namely, the Venezuelan, eastern, and western equine encephalitis viruses (VEEV, EEEV, and WEEV), are classified by the Centers for Disease Control and Prevention (CDC) as biothreat agents.
- neutralizing antibodies (Nabs)
- anti-EEEV
- anti-WEEV
1. Introduction
The three encephalitic alphaviruses, namely, the Venezuelan, eastern, and western equine encephalitis viruses (VEEV, EEEV, and WEEV), belong to the Alphavirus genus of the family Togaviridae [1]. All three encephalitic alphaviruses share a number of sequence, structural, and functional similarities, including a positive-sense and single-stranded RNA genome with two polyprotein gene clusters, namely, nonstructural and structural [2]. The nonstructural proteins are translated directly from the 5′ two-thirds of the genomic RNA. A subgenomic positive-stranded RNA (the 26S RNA) is identical to the 3′ one-third of the genome and serves as the translational template for the structural proteins, capsid (C), E3, E2, 6K, and E1 [3]. Three of these proteins, C, E1, and E2 are found on all mature encephalitic alphavirus virions, while the E3 protein has only been positively identified in VEEV capsids to date [4]. The C encapsidates the viral genome and lies beneath the viral lipid bilayer. E1 and E2 project from the virus envelope as trimeric spikes of E1/E2 heterodimers. The E1 protein is responsible for membrane fusion, while E2, the receptor-binding protein, is believed to be the major protective antigen [5][6]. EEEV formerly encompassed North American and South American strains, with the North American strains being much more virulent than their South American counterparts. The South American strains are now classified as a separate species, namely, the Madariaga virus, which has an approximately 23% difference in nucleotide sequence from EEEV [7].
In nature, these viruses primarily circulate through animal populations and infect humans via bites from mosquito carriers that have fed on infected animals. Human infection typically results in an acute and highly incapacitating disease that is characterized by severe symptoms that are similar to influenza. However, severe or fatal encephalitis can result from these viruses crossing the cerebral vascular endothelium or the olfactory epithelium [8]. In 2019, the northern USA provinces experienced the worst outbreak of EEEV since monitoring of the disease began 15 years ago and a total of 38 cases, including 12 deaths, were reported [9].
Accidental laboratory infections [1] and experimental studies in animals [10] with these three alphaviruses have demonstrated that they are highly infectious via the aerosol route. Furthermore, alphavirus infections via the aerosol route develop much faster, displaying higher morbidity compared with the natural (mosquito bite) route, likely because the aerosol route allows for more of the virus to contact olfactory neurons, thus expediting viral invasion of the brain [11]. In addition, high titers of these alphaviruses are easily obtained in cell culture and are relatively stable (either liquid or dry) in the environment. As such, VEEV, EEEV, and WEEV are classified by the Centers for Disease Control and Prevention (CDC) as biothreat agents [12]. Indeed, VEEV was weaponized and aerosolized as an incapacitating agent by the pre-1992 Soviet Union and pre-1969 United States biological warfare programs [13]. Currently, no licensed vaccines or therapeutics are available for any of these three encephalitic alphaviruses for the protection or treatment of humans [14].
Antibodies, which are naturally produced in the body as part of the immune response to infectious agents, can also be used in the form of polyclonal serum/plasma preparations or recombinantly manufactured neutralizing antibodies (NAbs) to passively immunize patients to prevent or treat infectious diseases [15][16][17][18]. NAbs can confer immediate and consistent protection against infectious agents when administered, regardless of the recipient’s immune status. The use of NAbs in an infectious disease emergency has been demonstrated in the 2010 and 2012 outbreaks of Hendra virus in Australia [19], and in the unprecedented 2013–2016 outbreak of the Ebola virus in West Africa [20], highlighting that NAbs can play a critical role in the management of a deadly infectious disease crisis. NAbs that are licensed by regulatory agencies are available for prophylaxis of respiratory syncytial virus and therapeutically to treat anthrax [21][22], demonstrating their utility as effective medical countermeasures (MCMs) against infectious agents [23][24].
2. The First Approach to Develop Anti-WEEV or Anti-EEEV NAbs
The rE2 antigens of EEEV V105-00210 and WEEV Fleming were shipped to a custom antibody service provider (Precision Antibody; PA; Columbia, MD, USA) for immunization of mice and generation of hybridoma clones that were reactive to the rE2 antigen of EEEV V105-00210 or WEEV Fleming.
A total of seven hybridoma clones that were reactive to the rE2 antigen of EEEV V105-00210 and 66 clones reactive to the rE2 antigen of WEEV Fleming were generated.
3. The Second Approach to Develop Anti-WEEV and Anti-EEEV NAbs
Female BALB/c mice (4–6 weeks old) were obtained from Charles River Canada (St Constant, QC, Canada). All mouse experiments were performed in strict accordance with the guidelines set out by the Canadian Council on Animal Care. The animal care protocol was reviewed and approved in 2013 by the Committee on the Ethics of Animal Experiments of DRDC SRC (protocol number: W1H-13-1-2-0). All efforts were made to minimize the suffering of the mice. The mice were intramuscularly (i.m.) immunized with immunogens in different formats from different strains to develop anti-EEEV or anti-WEEV Nabs, as shown in Figure 1 and Figure 2.
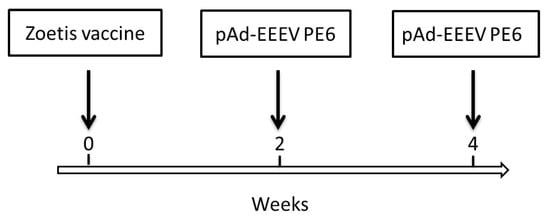
Figure 1. EEEV immunization scheme. Female BALB/c mice were i.m. primed with 100 µL/mouse of Zoetis vaccine at week zero and boosted with 100 µL/mouse of pAd-EEEV PE6 (100 µg) at weeks 2 and 4.
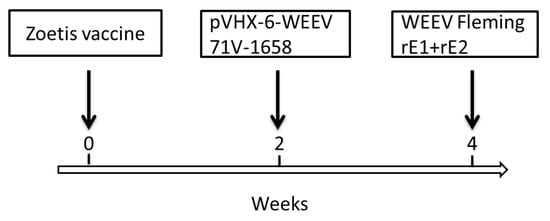
Figure 2. WEEV immunization scheme. Female BALB/c mice were i.m. primed with 100 µL/mouse of Zoetis vaccine at week zero and boosted with 100 µL/mouse of pVHX-6-WEEV 71V-1658 (100 µg) at week 2 and 100 µL/mouse of rE2 (100 µg) and rE1 (100 µg) of WEEV Fleming emulsified in 100 µL of TiterMax Gold adjuvant at week 4.
Three days after the last booster, five mice for each of EEEV and WEEV were sacrificed. Splenocytes were prepared and fused with myeloma cells in a standard hybridoma fusion protocol. Briefly, spleens were aseptically dissected from the immunized mice three days after the last booster, ground gently with autoclaved frosted-glass slides in DMEM, and filtered through a wire mesh screen to prepare splenocytes. Hybridomas were produced by fusing the splenocytes with Sp 2/0 myeloma cells using a Clonacell-HY Kit. After 2 weeks in a semisolid medium, five-thousand individual hybridoma clones for each virus were picked from semisolid medium and transferred to 96-well plates and cultured for 7 days in Clonacell Medium E, as previously described [25].
Hybridoma culture supernates were screened using an in vitro neutralization assay. Briefly, 20 pfu/well of EEEV PE6 or 125 pfu/well of WEEV 71V-1658 were incubated with a hybridoma culture supernate at 37 °C for 1 h. The mixtures were then added to Vero cells in 96-well plates (1 × 104 cells/well). Two or three days later, cells were observed under the microscope for cytopathic effects (CPE). Hybridoma clones that suppressed CPE were expanded. NAbs were purified from the cell culture supernate using a Melon Gel purification kit according to the manufacturer’s protocol. The supernate was dialyzed for two exchanges (1 h each) in Melon Gel IgG Purification Buffer pH 7.0 and then was added to a column containing the Melon Gel resin. After a 5 min incubation with end-over-end mixing, the purified IgG was collected in the flowthrough. All purified IgG samples were stored in aliquots at −70 °C.
4. Titration of NAbs against Various Strains of EEEV or WEEV
As shown in Figure 3, the alphavirus neutralization test (ANT) was carried out in 96-well plates. Three-fold serial dilutions of each NAb were screened, starting with a maximum concentration of 100 µg/mL. The volume of each well was 50 µL. Subsequently, 100× the 50% tissue culture infective dose (TCID50) of the virus in 50 µL was added to each well and then pre-incubated at 37 °C for 1 h to allow for neutralization of the virus. Thereafter, 1 × 104 cells/well (Vero) were added in a volume of 50 µL. Plates were then incubated at 37 °C under 5% CO2. After 3 days, the plates were examined microscopically. The NAb titer was identified as the highest dilution that resulted in 50% inhibition of CPE.
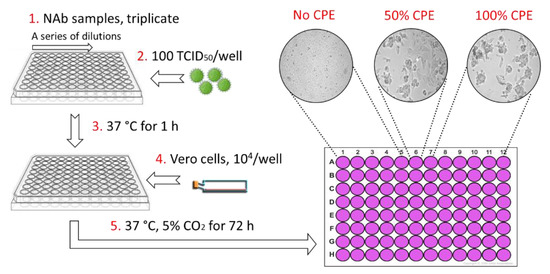
Figure 3. Anti-alphavirus neutralization titration assay. Serial 3-fold dilutions were made for each purified antibody in 50 µL. The virus (50 µL) was added to each well and then pre-incubated at 37 °C for 1 h. Thereafter, 1 × 104 Vero cells per well were added in a volume of 50 µL. Plates were then incubated for 3 days at 37 °C with 5% CO2 and then examined under a microscope. The NAb titer was identified as the highest dilution that resulted in 50% inhibition of CPE caused by 100 TCID50.
This entry is adapted from the peer-reviewed paper 10.3390/v13112231
References
- Zacks, M.A.; Paessler, S. Encephalitic alphaviruses. Vet. Microbiol. 2010, 140, 281–286.
- Johnston, R.E.; Peters, C.J. Alphavirus. In Fields Virology, 3rd ed.; Fields, B.N., Knipe, D.M., Howley, P.M., Eds.; Raven Publishers: Philadelphia, PA, USA, 1996; pp. 843–898.
- Strauss, J.H.; Strauss, E.G. The alphaviruses: Gene expression, replication, and evolution. Microbiol. Rev. 1994, 58, 491–562.
- Zhang, R.; Hryc, C.F.; Cong, Y.; Liu, X.; Jakana, J.; Gorchakov, R.; Baker, M.L.; Weaver, S.C.; Chiu, W. 4.4 A cryo-EM structure of an enveloped alphavirus Venezuelan equine encephalitis virus. EMBO J. 2011, 30, 3854–3863.
- France, J.K.; Wyrick, B.C.; Trent, D.W. Biochemical and antigenic comparison of the envelope glycoproteins of Venezuelan equine encephalomyelitis virus strains. J. Gen. Virol. 1979, 44, 725–740.
- Roehrig, J.T.; Day, J.W.; Kinney, R.M. Antigenic analysis of the surface glycoproteins of a Venezuelan equine encephalomyelitis virus (TC-83) using monoclonal antibodies. Virology 1982, 118, 269–278.
- Arrigo, N.C.; Adams, A.P.; Weaver, S.C. Evolutionary patterns of eastern equine encephalitis virus in North versus South America suggest ecological differences and taxonomic revision. J. Virol. 2010, 84, 1014–1025.
- Schafer, A.; Brooke, C.B.; Whitmore, A.C.; Johnston, R.E. The role of the blood-brain barrier during Venezuelan equine encephalitis virus infection. J. Virol. 2011, 85, 10682–10690.
- Breaking Down the 2019 Eastern Equine Encephalitis Outbreak in the US. Available online: https://www.contagionlive.com/news/breaking-down-the-2019-eastern-equine-encephalitis-outbreak-in-the-us (accessed on 20 January 2020).
- Steele, K.E.; Twenhafel, N.A. Review paper: Pathology of animal models of alphavirus encephalitis. Vet. Pathol. 2010, 47, 790–805.
- Hanson, R.P.; Sulkin, S.E.; Beuscher, E.L.; Hammon, W.M.; McKinney, R.W.; Work, T.H. Arbovirus infections of laboratory workers. Extent of problem emphasizes the need for more effective measures to reduce hazards. Science 1967, 158, 1283–1286.
- Moran, G.J. Threats in bioterrorism. II: CDC category B and C agents. Emerg. Med. Clin. N. Am. 2002, 20, 311–330.
- Sidwell, R.W.; Smee, D.F. Viruses of the Bunya-and Togaviridae families: Potential as bioterrorism agents and means of control. Antivir. Res. 2003, 57, 101–111.
- Nagata, L.P.; Wong, J.P.; Hu, W.G.; Wu, J.Q. Vaccines and therapeutics for the encephalitic alphaviruses. Future Virol. 2013, 8, 661–674.
- Casadevall, A. Antibody-based therapies for emerging infectious diseases. Emerg. Infect. Dis. 1996, 2, 200–208.
- Casadevall, A.; Scharff, M.D. Return to the past: The case for antibody-based therapies in infectious diseases. Clin. Infect. Dis. 1995, 21, 150–161.
- Zeitlin, L.; Cone, R.A.; Moench, T.R.; Whaley, K.J. Preventing infectious disease with passive immunization. Microbes Infect. 2000, 2, 701–708.
- Zeitlin, L.; Cone, R.A.; Whaley, K.J. Using monoclonal antibodies to prevent mucosal transmission of epidemic infectious diseases. Emerg. Infect. Dis. 1999, 5, 54–64.
- Pollard, E. Mother, Daughter Taking Experimental Hendra virus Drugs. ABC News. 28 May 2010. Available online: http://www.abc.net.au/news/2010-05-27/mother-daughter-taking-experimental-hendravirus/844358 (accessed on 14 August 2012).
- The PREVAIL II Writing Group; for the Multi-National PREVAIL II Study Team; Davey, R.T., Jr.; Dodd, L.; Proschan, M.A.; Neaton, J.; Neuhaus Nordwall, J.; Koopmeiners, J.S.; Beigel, J.; Tierney, J.; et al. A Randomized, Controlled Trial of ZMapp for Ebola Virus Infection. N. Engl. J. Med. 2016, 375, 1448–1456.
- Tsai, C.W.; Morris, S. Approval of Raxibacumab for the Treatment of Inhalation Anthrax under the US Food and Drug Administration “Animal Rule”. Front. Microbiol. 2015, 6, 1320.
- IMpact-RSV Study Group. Palivizumab, a humanized respiratory syncytial virus monoclonal antibody, reduces hospitalization from respiratory syncytial virus infection in high-risk infants. Pediatrics 1998, 102 Pt 1, 531–537.
- Hu, W.G.; Nagata, L.P. Opportunities and Challenges of Therapeutic Monoclonal Antibodies as Medical Countermeasures for Biodefense. J. Bioterrorism Biodefense 2016, 7, 1000149.
- Hu, W.G.; Nagata, L.P.; Vallerand, A. Novel Technology Platform of Therapeutic Antibody Development against Biothreat Agents: Cutting Edge Innovation for National Defence and Public Security. DRDC Scientific Letter 2015, DRDC-RDDC-2015-L189.
- Hu, W.G.; Yin, J.; Jager, S.; Wong, C.; Fulton, C.; Rayner, G.A.; Aw, C.; Fisher, G.R.; Dai, X.; Nagata, L.P. A novel approach to development of monoclonal antibodies using native antigen for immunization and recombinant antigen for screening. Hybridoma 2008, 27, 307–311.
This entry is offline, you can click here to edit this entry!
