Bone cancer including primary bone cancer and metastatic bone cancer, remains a challenge claiming millions of lives and affecting the life quality of survivors. Conventional treatments of bone cancer include wide surgical resection, radiotherapy, and chemotherapy. However, some bone cancer cells may remain or recur in the local area after resection, some are highly resistant to chemotherapy, and some are insensitive to radiotherapy. Photodynamic therapy (PDT) is a clinically approved, minimally invasive, and highly selective treatment, and has been widely reported for cancer therapy. Under the irradiation of light of a specific wavelength, the photosensitizer (PS) in PDT can cause the increase of intracellular ROS leading to the tumoricidal effects. In this review, the progress of PDT applications in the treatment of bone cancer has been outlined and summarized, and some envisioned challenges and future perspectives have been mentioned. This review provides the current state of the art regarding PDT in bone cancer and inspiration for future studies on PDT.
- photodynamic therapy
- bone cancer
- nanoparticles
- Oncology
1. Introduction
2. PDT
3. Application of PDT in Bone Cancer
3.1. Preliminary Studies on the Therapeutic Effect of PDT on Bone Cancer
3.2. PDT Using New Generations of PSs for Bone Cancer
3.2.1. Dextran-Benzoporphyrin Derivatives (BPD)
3.2.2. Acridine Orange (AO)
3.2.3. Aminolevulinic Acid (ALA)
3.2.4. 5,10,15,20-Tetrakis(meta-hydroxyphenyl)chlorine (mTHPC)
3.2.5. Indocyanine Green (ICG)
3.2.6. Methylene Blue (MB)
3.2.7. Chlorin e6 (Ce6)
3.2.8. Chlorophyll Derivatives
3.2.9. Benzochloroporphyrin Derivatives (BCPDs)
3.2.10. Other Porphyrin Derivatives
3.2.11. Photodynamic Molecular Beacons (PMBs)
3.2.12. Other New PSs
3.3. Combination of PDT and Other Therapies for Bone Cancer
3.3.1. PDT Combined with Chemotherapy
3.3.2. PDT Combined with Immunotherapy
3.3.3. PDT Combined with Hyperthermia
3.3.4. PDT Combined with Radiotherapy
3.3.5. Other Applications of PDT for Clinical Bone Cancer
4. Conclusions and outlooks
As some bone cancer cells may remain or recur in the local area after tumor resection, some are highly resistant to chemotherapy, and some are insensitive to radiotherapy, there are multiple undesirable results following bone cancer therapy, such as motor dysfunction, neurological symptoms, reduced quality of life, and mental and economic burdens. PDT has the advantages of minimally invasive, highly efficient and selective, and easy to combine with other treatments. Therefore, PDT is recognized as a new generation of effective treatment for bone cancer. The most used light source in PDT is the light with absorbance in the NIR region, which possesses sufficient tissue penetration and minor side effects, and can induce the generation of intracellular ROS to ablate tumor cells. Studies on PDT for bone cancer are mainly focused on the development and optimization of PSs, in order to improve the safety and efficiency of the second- or third-generation PSs. Nanoformulation is the main trend in the development of PSs which can endow PSs with bone- or tumor-targeting capacity, the ability of loading chemotherapeutic or immunotherapeutic drugs, and enhanced biocompatibility and residence time. In addition, nanocarriers based on metal nanoparticles or organic NIR dyes exhibit both PDT and PTT effects, and the resulting synergistic phototherapy has stronger tumoricidal effects while the side effects are not improved. Moreover, some researchers are focusing on the specific mechanisms of PDT effects on tumor therapy and they want to further improve the effects via altering the expression of involved molecules in corresponding signaling pathways [183]. Recently, computerized medical imaging has also been employed for the diagnosis, planning, and real-time monitoring during PDT [184].
However, there are also some crucial challenges or opportunities for further clinical applications of PDT. Firstly, the PDT efficiency and side effects depend on the time, intensity, and interval of light irradiation, as well as the amount of PSs. Therefore, guidelines for the clinical use of PDT are necessary. When PDT combined with minimally invasive techniques such as endoscopy is used for deep bone cancer, the clinical protocol can be customized according to existing ones for other superficial tumors. Secondly, the long-term metabolism and biocompatibility of the nanoscale PSs, and the tumor-targeting capacity and specificity of PSs for various cancers, are required further studies. Thirdly, pre-clinical and clinical experiments of real-time monitoring for local immune response and situations of surrounding normal tissues are also needed. Finally, although the combined applications of PDT and other conventional treatments are the most interesting area among studies, the necessity, economic benefits, safety, and efficacy of these combined therapies require detailed discussion depending on each individual. In summary, PDT for bone cancer has developed rapidly in recent years, and we strongly believe that PDT has great prospects in tumor therapy. We hope this review can provide valuable information and insights for future studies on PDT.
This entry is adapted from the peer-reviewed paper 10.3390/ijms222111354
References
- Rainusso, N.; Wang, L.L.; Yustein, J.T. The adolescent and young adult with cancer: State of the art—Bone tumors. Curr. Oncol. Rep. 2013, 15, 296–307.
- Gorlick, R.; Janeway, K.; Lessnick, S.; Randall, R.L.; Marina, N.; Committee, C.O.G.B.T. Children’s Oncology Group’s 2013 blueprint for research: Bone tumors. Pediatr. Blood Cancer 2013, 60, 1009–1015.
- Siclari, V.A.; Qin, L. Targeting the osteosarcoma cancer stem cell. J. Orthop. Surg. Res. 2010, 5, 78.
- Chen, D.; Zhao, Z.; Huang, Z.; Chen, D.C.; Zhu, X.X.; Wang, Y.Z.; Yan, Y.W.; Tang, S.; Madhavan, S.; Ni, W.; et al. Super enhancer inhibitors suppress MYC driven transcriptional amplification and tumor progression in osteosarcoma. Bone Res. 2018, 6, 11.
- Isakoff, M.S.; Bielack, S.S.; Meltzer, P.; Gorlick, R. Osteosarcoma: Current Treatment and a Collaborative Pathway to Success. J. Clin. Oncol. 2015, 33, 3029–3035.
- Italiano, A.; Mir, O.; Cioffi, A.; Palmerini, E.; Piperno-Neumann, S.; Perrin, C.; Chaigneau, L.; Penel, N.; Duffaud, F.; Kurtz, J.E.; et al. Advanced chondrosarcomas: Role of chemotherapy and survival. Ann. Oncol. 2013, 24, 2916–2922.
- Gaspar, N.; Hawkins, D.S.; Dirksen, U.; Lewis, I.J.; Ferrari, S.; Le Deley, M.C.; Kovar, H.; Grimer, R.; Whelan, J.; Claude, L.; et al. Ewing Sarcoma: Current Management and Future Approaches Through Collaboration. J. Clin. Oncol. 2015, 33, 3036–3046.
- Mundy, G.R. Metastasis to bone: Causes, consequences and therapeutic opportunities. Nat. Rev. Cancer 2002, 2, 584–593.
- Schroeder, A.; Heller, D.A.; Winslow, M.M.; Dahlman, J.E.; Pratt, G.W.; Langer, R.; Jacks, T.; Anderson, D.G. Treating metastatic cancer with nanotechnology. Nat. Rev. Cancer 2011, 12, 39–50.
- Yuasa, T.; Urakami, S. Kidney cancer: Decreased incidence of skeletal-related events in mRCC. Nat. Rev. Urol. 2014, 11, 193–194.
- Fukutomia, M.; Yokotaa, M.; Chumanb, H.; Haradab, H.; Zaitsub, Y.; Funakoshia, A.; Wakasugia, H.; Iguchi, H. Increased incidence of bone metastases in hepatocellular carcinoma. Eur. J. Gastroenterol. Hepatol. 2001, 13, 1083–1088.
- Weilbaecher, K.N.; Guise, T.A.; McCauley, L.K. Cancer to bone: A fatal attraction. Nat. Rev. Cancer 2011, 11, 411–425.
- Suva, L.J.; Washam, C.; Nicholas, R.W.; Griffin, R.J. Bone metastasis: Mechanisms and therapeutic opportunities. Nat. Rev. Endocrinol. 2011, 7, 208–218.
- Heck, R.K.; Peabody, T.D.; Simon, M.A. Staging of Primary Malignancies of Bone. CA Cancer J. Clin. 2006, 56, 366–375.
- Saber-Samandari, S.; Nezafati, N.; Saber-Samandari, S. The Effective Role of Hydroxyapatite-Based Composites in Anticancer Drug-Delivery Systems. Crit. Rev. Ther. Drug Carrier Syst. 2016, 33, 41–75.
- Van der Bij, G.J.; Oosterling, S.J.; Beelen, R.H.; Meijer, S.; Coffey, J.C.; van Egmond, M. The perioperative period is an underutilized window of therapeutic opportunity in patients with colorectal cancer. Ann. Surg. 2009, 249, 727–734.
- Thakor, A.S.; Gambhir, S.S. Nanooncology: The Future of Cancer Diagnosis and Therapy. CA Cancer J. Clin. 2013, 63, 395–418.
- Shakhar, G.; Ben-Eliyahu, S. Potential prophylactic measures against postoperative immunosuppression: Could they reduce recurrence rates in oncological patients? Ann. Surg. Oncol. 2003, 10, 972–992.
- Letfullin, R.R.; Rice, C.E.; George, T.F. Theoretical study of bone cancer therapy by plasmonic nanoparticles. Ther. Deliv. 2011, 2, 1259–1273.
- Au, C.M.; Luk, S.K.; Jackson, C.J.; Ng, H.K.; Yow, C.M.; To, S.S. Differential effects of photofrin, 5-aminolevulinic acid and calphostin C on glioma cells. J. Photochem. Photobiol. B 2006, 85, 92–101.
- Gu, W.; Zhang, T.; Gao, J.; Wang, Y.; Li, D.; Zhao, Z.; Jiang, B.; Dong, Z.; Liu, H. Albumin-bioinspired iridium oxide nanoplatform with high photothermal conversion efficiency for synergistic chemo-photothermal of osteosarcoma. Drug Deliv. 2019, 26, 918–927.
- Bu, W.; Wang, Y.; Chen, X.; Fang, F. Novel strategy in giant cutaneous squamous cell carcinoma treatment: The case experience with a combination of photodynamic therapy and surgery. Photodiagn. Photodyn. Ther. 2017, 19, 116–118.
- Castilho-Fernandes, A.; Lopes, T.G.; Primo, F.L.; Pinto, M.R.; Tedesco, A.C. Photodynamic process induced by chloro-aluminum phthalocyanine nanoemulsion in glioblastoma. Photodiagn. Photodyn. Ther. 2017, 19, 221–228.
- Fahey, J.M.; Korytowski, W.; Girotti, A.W. Upstream signaling events leading to elevated production of pro-survival nitric oxide in photodynamically-challenged glioblastoma cells. Free Radic. Biol. Med. 2019, 137, 37–45.
- Kargozar, S.; Mozafari, M.; Ghodrat, S.; Fiume, E.; Baino, F. Copper-containing bioactive glasses and glass-ceramics: From tissue regeneration to cancer therapeutic strategies. Mater. Sci. Eng. C Mater. Biol. Appl. 2021, 121, 111741.
- Zhou, M.; Xing, Y.; Li, X.; Du, X.; Xu, T.; Zhang, X. Cancer Cell Membrane Camouflaged Nanomotor for Enhanced Cell Adhesion and Synergistic Therapy. Small 2020, 16, e2003834.
- Cheng, K.; Zhang, R.Y.; Yang, X.Q.; Zhang, X.S.; Zhang, F.; An, J.; Wang, Z.Y.; Dong, Y.; Liu, B.; Zhao, Y.D.; et al. One-for-All Nanoplatform for Synergistic Mild Cascade-Potentiated Ultrasound Therapy Induced with Targeting Imaging-Guided Photothermal Therapy. ACS Appl. Mater. Interface 2020, 12, 40052–40066.
- Hu, Z.; Wang, S.; Dai, Z.; Zhang, H.; Zheng, X. A novel theranostic nano-platform () for tumor chemodynamic-photothermal co-therapy and triple-modal imaging (MR/CT/PI) diagnosis. J. Mater. Chem. B 2020, 8, 5351–5360.
- Doughty, A.C.V.; Hoover, A.R.; Layton, E.; Murray, C.K.; Howard, E.W.; Chen, W.R. Nanomaterial Applications in Photothermal Therapy for Cancer. Materials 2019, 12, 779.
- Du, P.; Hu, S.; Cheng, Y.; Li, F.; Li, M.; Li, J.; Yi, L.; Feng, H. Photodynamic therapy leads to death of C6 glioma cells partly through AMPAR. Brain Res. 2012, 1433, 153–159.
- Caesar, L.; van Doeveren, T.E.; Tan, I.B.; Dilci, A.; van Veen, R.L.; Karakullukcu, B. The use of photodynamic therapy as adjuvant therapy to surgery in recurrent malignant tumors of the paranasal sinuses. Photodiagn. Photodyn. Ther. 2015, 12, 414–421.
- Chen, S.; Lei, Q.; Qiu, W.X.; Liu, L.H.; Zheng, D.W.; Fan, J.X.; Rong, L.; Sun, Y.X.; Zhang, X.Z. Mitochondria-targeting “Nanoheater” for enhanced photothermal/chemo-therapy. Biomaterials 2017, 117, 92–104.
- Wang, D.; Dong, H.; Li, M.; Cao, Y.; Yang, F.; Zhang, K.; Dai, W.; Wang, C.; Zhang, X. Erythrocyte-Cancer Hybrid Membrane Camouflaged Hollow Copper Sulfide Nanoparticles for Prolonged Circulation Life and Homotypic-Targeting Photothermal/Chemotherapy of Melanoma. ACS Nano 2018, 12, 5241–5252.
- Allison, R.R.; Mota, H.C.; Sibata, C.H. Clinical PD/PDT in North America: An historical review. Photodiagn. Photodyn. Ther. 2004, 1, 263–277.
- Dougherty, T.J. Photodynamic therapy (PDT) of malignant tumors. Crit. Rev. Oncol. Hematol. 1984, 2, 83–116.
- Felsher, D.W. Cancer revoked: Oncogenes as therapeutic targets. Nat. Rev. Cancer 2003, 3, 375–380.
- Ghorbani, J.; Rahban, D.; Aghamiri, S.; Teymouri, A.; Bahador, A. Photosensitizers in antibacterial photodynamic therapy: An overview. Laser Ther. 2018, 27, 293–302.
- Wen, X.; Li, Y.; Hamblin, M.R. Photodynamic therapy in dermatology beyond non-melanoma cancer: An update. Photodiagn. Photodyn. Ther. 2017, 19, 140–152.
- Rkein, A.M.; Ozog, D.M. Photodynamic therapy. Dermatol. Clin. 2014, 32, 415–425.
- Mansoori, B.; Mohammadi, A.; Amin Doustvandi, M.; Mohammadnejad, F.; Kamari, F.; Gjerstorff, M.F.; Baradaran, B.; Hamblin, M.R. Photodynamic therapy for cancer: Role of natural products. Photodiagn. Photodyn. Ther. 2019, 26, 395–404.
- Agostinis, P.; Berg, K.; Cengel, K.A.; Foster, T.H.; Girotti, A.W.; Gollnick, S.O.; Hahn, S.M.; Hamblin, M.R.; Juzeniene, A.; Kessel, D.; et al. Photodynamic therapy of cancer: An update. CA Cancer J. Clin. 2011, 61, 250–281.
- Cruz, P.M.; Mo, H.; McConathy, W.J.; Sabnis, N.; Lacko, A.G. The role of cholesterol metabolism and cholesterol transport in carcinogenesis: A review of scientific findings, relevant to future cancer therapeutics. Front. Pharmacol. 2013, 4, 119.
- Castano, A.P.; Demidova, T.N.; Hamblin, M.R. Mechanisms in photodynamic therapy: Part three—Photosensitizer pharmacokinetics, biodistribution, tumor localization and modes of tumor destruction. Photodiagn. Photodyn. Ther. 2005, 2, 91–106.
- Sattler, U.G.; Mueller-Klieser, W. The anti-oxidant capacity of tumour glycolysis. Int. J. Radiat. Biol. 2009, 85, 963–971.
- Golab, J.; Nowis, D.; Skrzycki, M.; Czeczot, H.; Baranczyk-Kuzma, A.; Wilczynski, G.M.; Makowski, M.; Mroz, P.; Kozar, K.; Kaminski, R.; et al. Antitumor effects of photodynamic therapy are potentiated by 2-methoxyestradiol. A superoxide dismutase inhibitor. J. Biol. Chem. 2003, 278, 407–414.
- Oleinick, N.L.; Morris, R.L.; Belichenko, I. The role of apoptosis in response to photodynamic therapy: What, where, why, and how. Photochem. Photobiol. Sci. 2002, 1, 1–21.
- Kwiatkowski, S.; Knap, B.; Przystupski, D.; Saczko, J.; Kedzierska, E.; Knap-Czop, K.; Kotlinska, J.; Michel, O.; Kotowski, K.; Kulbacka, J. Photodynamic therapy—Mechanisms, photosensitizers and combinations. Biomed. Pharmacother. 2018, 106, 1098–1107.
- Zhang, X.; Liu, T.; Li, Z.; Zhang, X. Progress of photodynamic therapy applications in the treatment of musculoskeletal sarcoma (Review). Oncol. Lett. 2014, 8, 1403–1408.
- Chilakamarthi, U.; Giribabu, L. Photodynamic Therapy: Past, Present and Future. Chem. Rec. 2017, 17, 775–802.
- TJ, D.; MT, C.; TS, M. Cutaneous phototoxic occurrences in patients receiving Photofrin. Lasers Surg. Med. 1990, 10, 485–488.
- Zhang, J.; Jiang, C.; Figueiro Longo, J.P.; Azevedo, R.B.; Zhang, H.; Muehlmann, L.A. An updated overview on the development of new photosensitizers for anticancer photodynamic therapy. Acta Pharm. Sin. B. 2018, 8, 137–146.
- Abrahamse, H.; Hamblin, M.R. New photosensitizers for photodynamic therapy. Biochem. J. 2016, 473, 347–364.
- Yoon, I.; Li, J.Z.; Shim, Y.K. Advance in photosensitizers and light delivery for photodynamic therapy. Clin. Endosc. 2013, 46, 7–23.
- Kennedy, J.C.; Pottier, R.H. Endogenous protoporphyrin IX, a clinically useful photosensitizer for photodynamic therapy. J. Photochem. Photobiol. B 1992, 14, 275–292.
- Lan, M.; Zhao, S.; Liu, W.; Lee, C.S.; Zhang, W.; Wang, P. Photosensitizers for Photodynamic Therapy. Adv. Healthc. Mater. 2019, 8, e1900132.
- Josefsen, L.B.; Boyle, R.W. Photodynamic therapy: Novel third-generation photosensitizers one step closer? Br. J. Pharmacol. 2008, 154, 1–3.
- Beharry, A.A. Next-Generation Photodynamic Therapy: New Probes for Cancer Imaging and Treatment. Biochemistry 2018, 57, 173–174.
- Kataoka, H.; Nishie, H.; Hayashi, N.; Tanaka, M.; Nomoto, A.; Yano, S.; Joh, T. New photodynamic therapy with next-generation photosensitizers. Ann. Transl. Med. 2017, 5, 183.
- Savellano, M.D.; Hasan, T. Targeting cells that overexpress the epidermal growth factor receptor with polyethylene glycolated BPD verteporfin photosensitizer immunoconjugates. Photochem. Photobiol. 2003, 74, 431–439.
- Huang, Z. A review of progress in clinical photodynamic therapy. Technol. Cancer Res. Treat. 2005, 4, 283–293.
- Juzeniene, A.; Juzenas, P.; Ma, L.W.; Iani, V.; Moan, J. Effectiveness of different light sources for 5-aminolevulinic acid photodynamic therapy. Lasers Med. Sci. 2004, 19, 139–149.
- Brancaleon, L.; Moseley, H. Laser and non-laser light sources for photodynamic therapy. Lasers Med. Sci. 2002, 17, 173–186.
- Kim, M.M.; Darafsheh, A. Light Sources and Dosimetry Techniques for Photodynamic Therapy. Photochem. Photobiol. 2020, 96, 280–294.
- Calin, M.A.; Diaconeasa, A.; Savastru, D.; Tautan, M. Photosensitizers and light sources for photodynamic therapy of the Bowen’s disease. Arch. Dermatol. Res. 2011, 303, 145–151.
- Jayadevappa, R.; Chhatre, S.; Soukiasian, H.J.; Murgu, S. Outcomes of patients with advanced non-small cell lung cancer and airway obstruction treated with photodynamic therapy and non-photodynamic therapy ablation modalities. J. Thorac. Dis. 2019, 11, 4389–4399.
- Saravana-Bawan, S.; David, E.; Sahgal, A.; Chow, E. Palliation of bone metastases-exploring options beyond radiotherapy. Ann. Palliat. Med. 2019, 8, 168–177.
- Fingar, V.H.; Wieman, T.J.; Doak, K.W. Role of Thromboxane and Prostacyclin Release on Photodynamic Therapy-induced Tumor Destruction. Cancer Res. 1990, 50, 2599–2603.
- Fingar, V.H.; Wieman, T.J.; Doak, K.W. Changes in tumor interstitial pressure induced by photodynamic therapy. Photochem. Photobiol. 1991, 53, 763–768.
- Meyer, M.; Speight, P.; Bown, S.G. A study of the effects of photodynamic therapy on the normal tissues of the rabbit jaw. Br. J. Cancer 1991, 64, 1093–1097.
- Hourigan, A.J.; Kells, A.F.; Schwartz, H.S. In vitro Photodynamic Therapy of Musculoskeletal Neoplasms. J. Orthop. Res. 1993, 11, 633–637.
- Fingar, V.H.; Kik, P.K.; Haydon, P.S.; Cerrito, P.B.; Tseng, M.; Abang, E.; Wieman, T.J. Analysis of acute vascular damage after photodynamic therapy using benzoporphyrin derivative (BPD). Br. J. Cancer 1999, 79, 1702–1708.
- Burch, S.; London, C.; Seguin, B.; Rodriguez, C.; Wilson, B.C.; Bisland, S.K. Treatment of canine osseous tumors with photodynamic therapy: A pilot study. Clin. Orthop. Relat. Res. 2009, 467, 1028–1034.
- Burch, S.; Bogaards, A.; Siewerdsen, J.; Moseley, D.; Yee, A.; Finkelstein, J.; Weersink, R.; Wilson, B.C.; Bisland, S.K. Photodynamic therapy for the treatment of metastatic lesions in bone: Studies in rat and porcine models. J. Biomed. Opt. 2005, 10, 034011.
- Bisland, S.K.; Burch, S. Photodynamic therapy of diseased bone. Photodiagn. Photodyn. Ther. 2006, 3, 147–155.
- Akens, M.K.; Yee, A.J.; Wilson, B.C.; Burch, S.; Johnson, C.L.; Lilge, L.; Bisland, S.K. Photodynamic therapy of vertebral metastases: Evaluating tumor-to-neural tissue uptake of BPD-MA and ALA-PpIX in a murine model of metastatic human breast carcinoma. Photochem. Photobiol. 2007, 83, 1034–1039.
- Akens, M.K.; Hardisty, M.R.; Wilson, B.C.; Schwock, J.; Whyne, C.M.; Burch, S.; Yee, A.J. Defining the therapeutic window of vertebral photodynamic therapy in a murine pre-clinical model of breast cancer metastasis using the photosensitizer BPD-MA (Verteporfin). Breast Cancer Res. Treat. 2010, 119, 325–333.
- Won, E.; Akens, M.K.; Hardisty, M.R.; Burch, S.; Bisland, S.K.; Yee, A.J.M.; Wilson, B.C.; Whyne, C.M. Effects of Photodynamic Therapy on the Structural Integrity of Vertebral Bone. Spine 2010, 35, 272–277.
- Wise-Milestone, L.; Akens, M.K.; Lo, V.C.; Yee, A.J.; Wilson, B.C.; Whyne, C.M. Local treatment of mixed osteolytic/osteoblastic spinal metastases: Is photodynamic therapy effective? Breast Cancer Res. Treat. 2012, 133, 899–908.
- Matsubara, T.; Kusuzaki, K.; Matsumine, A.; Murata, H.; Marunaka, Y.; Hosogi, S.; Uchida, A.; Sudo, A. Photodynamic therapy with acridine orange in musculoskeletal sarcomas. J. Bone Jt. Surg. 2010, 92-B, 760–762.
- Matsubara, T.; Kusuzaki, K.; Matsumine, A.; Shintani, K.; Satonaka, H.; Uchida, A. Acridine Orange Used for Photodynamic Therapy Accumulates in Malignant Musculoskeletal Tumors Depending on pH Gradient. Anticancer Res. 2006, 26, 187–194.
- Kusuzaki, K.; Aomori, K.; Suginoshita, T.; Minami, G.; Takeshita, H.; Murata, H.; Hashiguchi, S.; Ashihara, T.; Hirasaw, Y. Total Tumor Cell Elimination with Minimum Damage to Normal Tissues in Musculoskeletal Sarcomas following Photodynamic Therapy with Acridine Orange. Oncology 2000, 59, 174–180.
- Kusuzaki, K.; Minami, G.; Takeshita, H.; Murata, H.; Hashiguchi, S.; Nozaki, T.; Ashihara, T.; Hirasawa, Y. Photodynamic Inactivation with Acridine Orange on a Multidrug-resistant Mouse Osteosarcoma Cell Line. Jpn. J. Cancer Res. 2000, 91, 439–445.
- Ueda, H.; Murata, H.; Takeshita, H.; Minami, G.; Hashiguchi, S.; Kubo, T. Unfiltered Xenon Light is Useful for Photodynamic Therapy with Acridine Orange. Anticancer Res. 2005, 25, 3979–3984.
- Satonaka, H.; Kusuzaki, K.; Matubara, T.; Shintani, K.; Wakabayashi, T.; Nakamura, T.; Matsumine, A.; Uchida, A. Flash Wave Light Strongly Enhanced the Cytocidal Effect of Photodynamic Therapy with Acridine Orange on a Mouse Osteosarcoma Cell Line. Anticancer Res. 2007, 27, 3339–3344.
- Dietze, A.; Berg, K. ALA-induced porphyrin formation and fluorescence in synovitis tissue. Photodiagn. Photodyn. Ther. 2005, 2, 299–307.
- White, B.; Rossi, V.; Baugher, P.J. Aminolevulinic Acid-Mediated Photodynamic Therapy Causes Cell Death in MG-63 Human Osteosarcoma Cells. Photomed. Laser Surg. 2016, 34, 400–405.
- Coupienne, I.; Fettweis, G.; Piette, J. RIP3 expression induces a death profile change in U2OS osteosarcoma cells after 5-ALA-PDT. Lasers Surg. Med. 2011, 43, 557–564.
- Meier, D.; Campanile, C.; Botter, S.M.; Born, W.; Fuchs, B. Cytotoxic efficacy of photodynamic therapy in osteosarcoma cells in vitro. J. Vis. Exp. 2014.
- Reidy, K.; Campanile, C.; Muff, R.; Born, W.; Fuchs, B. mTHPC-mediated photodynamic therapy is effective in the metastatic human 143B osteosarcoma cells. Photochem. Photobiol. 2012, 88, 721–727.
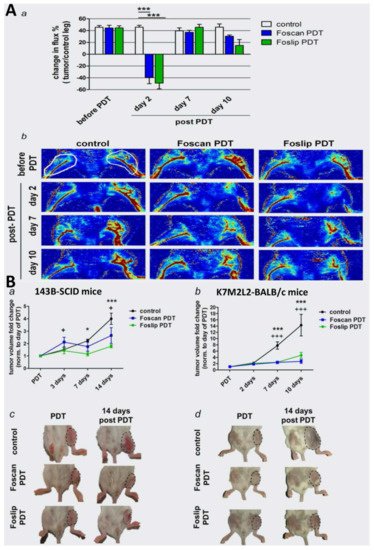
- Meier, D.; Botter, S.M.; Campanile, C.; Robl, B.; Grafe, S.; Pellegrini, G.; Born, W.; Fuchs, B. Foscan and foslip based photodynamic therapy in osteosarcoma in vitro and in intratibial mouse models. Int. J. Cancer 2017, 140, 1680–1692.
- Sakka, S.G. Assessment of liver perfusion and function by indocyanine green in the perioperative setting and in critically ill patients. J. Clin. Monit. Comput. 2018, 32, 787–796.
- Maarek, J.-M.I.; Holschneider, D.P.; Rubinstein, E.H. Fluorescence dilution technique for measurement of cardiac output and circulating blood volume in healthy human subjects. Anesthesiology 2007, 106, 491–498.
- Bozkulak, O.; Yamaci, R.F.; Tabakoglu, O.; Gulsoy, M. Photo-toxic effects of 809-nm diode laser and indocyanine green on MDA-MB231 breast cancer cells. Photodiagn. Photodyn. Ther. 2009, 6, 117–121.
- Skrivanova, K.; Skorpikova, J.; Svihalek, J.; Mornstein, V.; Janisch, R. Photochemical properties of a potential photosensitiser indocyanine green in vitro. J. Photochem. Photobiol. B 2006, 85, 150–154.
- Bäumler, W.; Abels, C.; Karrer, S.; Weiß, T.; Messmann, H.; Landthaler, M.; Szeimies, R.-M. Photo-oxidative killing of human colonic cancer cells using indocyanine green and infrared light. Br. J. Cancer 1999, 80, 360–363.
- Funayama, T.; Sakane, M.; Abe, T.; Ochiai, N. Photodynamic therapy with indocyanine green injection and near-infrared light irradiation has phototoxic effects and delays paralysis in spinal metastasis. Photomed. Laser Surg. 2012, 30, 47–53.
- Funayama, T.; Tsukanishi, T.; Hara, I.; Ozeki, E.; Sakane, M. Tumor-selective near-infrared photodynamic therapy with novel indocyanine green-loaded nanocarrier delays paralysis in rats with spinal metastasis. Photodiagn. Photodyn. Ther. 2013, 10, 374–378.
- GS, T.; SL, F.; VM, R.; MA, C. Methylene blue reverts multidrug resistance: Sensitivity of multidrug resistant cells to this dye and its photodynamic action. Cancer Lett. 2000, 151, 161–167.
- Rice, L.; Wainwright, M.; Phoemix, D.A. Phenothiazine photosensitizers. III. Activity of methylene blue derivatives against pigmented melanoma cell lines. J. Chemother. 2000, 12, 94–104.
- Matsubara, T.; Kusuzaki, K.; Matsumine, A.; Satonaka, H.; Shintani, K.; Nakamura, T.; Uchida, A. Methylene blue in place of acridine orange as a photosensitizer in photodynamic therapy of osteosarcoma. In Vivo 2008, 22, 297–304.
- Guan, J.; Lai, X.; Wang, X.; Leung, A.W.; Zhang, H.; Xu, C. Photodynamic action of methylene blue in osteosarcoma cells in vitro. Photodiagn. Photodyn. Ther. 2014, 11, 13–19.
- Elfeky, S.A.; Elsayed, A.; Moawad, M.; Ahmed, W.A. Hydroxyapatite nanocomposite as a potential agent in osteosarcoma PDT. Photodiagn. Photodyn. Ther. 2020, 32, 102056.
- Darwish, K.M.; Salama, I.; Mostafa, S.; El-Sadek, M. RP-HPLC/pre-column derivatization for analysis of omeprazole, tinidazole, doxycycline and clarithromycin. J. Chromatogr. Sci. 2013, 51, 566–576.
- Wang, X.; Hu, J.; Wang, P.; Zhang, S.; Liu, Y.; Xiong, W.; Liu, Q. Analysis of the in vivo and in vitro effects of photodynamic therapy on breast cancer by using a sensitizer, sinoporphyrin sodium. Theranostics 2015, 5, 772–786.
- Mohsenian, N.B.; Shanei, A.; Alavi, S.J.; Kheirollahi, M.; Nia, A.H.; Tavakoli, M.B. Mn-doped ZnS quantum dots-chlorin e6 shows potential as a treatment for chondrosarcoma: An in vitro study. IET Nanobiotechnol. 2019, 13, 387–391.
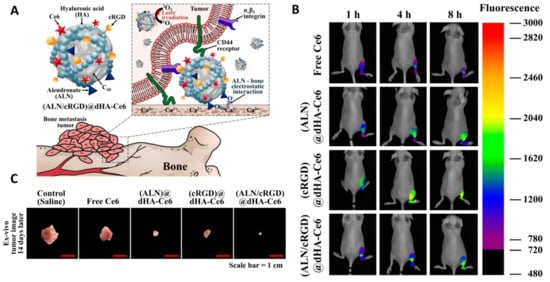
- Lee, E.; Park, J.; Youn, Y.S.; Oh, K.T.; Kim, D.; Lee, E.S. Alendronate/cRGD-Decorated Ultrafine Hyaluronate Dot Targeting Bone Metastasis. Biomedicines 2020, 8, 492.
- Iriuchishima, T.; Saito, A.; Aizawa, S.; Taira, K.; Yamamoto, T.; Ryu, J. The minimum influences for murine normal joint tissue by novel bactericidal treatment and photodynamic therapy using na-pheophorbide a for septic arthritis. Photomed. Laser Surg. 2008, 26, 153–158.
- Nagai, Y.; Aizawa, S.; Iriuchishima, T.; Goto, B.; Nagaoka, M.; Tokuhashi, Y.; Saito, A. Phototoxic effect of na-pheophorbide a toward osteosarcoma cells in vitro using a laser diode. Photomed. Laser Surg. 2014, 32, 481–489.
- Schreiber, S.; Gross, S.; Brandis, A.; Harmelin, A.; Rosenbach-Belkin, V.; Scherz, A.; Salomon, Y. Local photodynamic therapy (PDT) of rat C6 glioma xenografts with Pd-bacteriopheophorbide leads to decreased metastases and increase of animal cure compared with surgery. Int. J. Cancer 2002, 99, 279–285.
- Koudinova, N.V.; Pinthus, J.H.; Brandis, A.; Brenner, O.; Bendel, P.; Ramon, J.; Eshhar, Z.; Scherz, A.; Salomon, Y. Photodynamic therapy with Pd-Bacteriopheophorbide (TOOKAD): Successful in vivo treatment of human prostatic small cell carcinoma xenografts. Int. J. Cancer 2003, 104, 782–789.
- Huang, Q.; Ou, Y.S.; Tao, Y.; Yin, H.; Tu, P.H. Apoptosis and autophagy induced by pyropheophorbide-alpha methyl ester-mediated photodynamic therapy in human osteosarcoma MG-63 cells. Apoptosis 2016, 21, 749–760.
- Chen, Y.; Yin, H.; Tao, Y.; Zhong, S.; Yu, H.; Li, J.; Bai, Z.; Ou, Y. Antitumor effects and mechanisms of pyropheophorbidealpha methyl estermediated photodynamic therapy on the human osteosarcoma cell line MG. Int. J. Mol. Med. 2020, 45, 971–982.
- Yao, J.; Zhang, W.; Sheng, C.; Miao, Z.; Yang, F.; Yu, J.; Zhang, L.; Song, Y.; Zhou, T.; Zhou, Y. Design, synthesis, and in vitro photodynamic activities of benzochloroporphyrin derivatives as tumor photosensitizers. Bioorg. Med. Chem. Lett. 2008, 18, 293–297.
- Gong, H.Y.; Sun, M.X.; Hu, S.; Tao, Y.Y.; Gao, B.; Li, G.D.; Cai, Z.D.; Yao, J.Z. Benzochloroporphyrin derivative induced cytotoxicity and inhibition of tumor recurrence during photodynamic therapy for osteosarcoma. Asian Pac. J. Cancer Prev. 2013, 14, 3351–3355.
- Sun, M.; Zhou, C.; Zeng, H.; Yin, F.; Wang, Z.; Yao, J.; Hua, Y.; Cai, Z. Benzochloroporphyrin derivative photosensitizer-mediated photodynamic therapy for Ewing sarcoma. J. Photochem. Photobiol. B 2016, 160, 178–184.
- Zeng, H.; Sun, M.; Zhou, C.; Yin, F.; Wang, Z.; Hua, Y.; Ca, Z. Hematoporphyrin Monomethyl Ether-Mediated Photodynamic Therapy Selectively Kills Sarcomas by Inducing Apoptosis. PLoS ONE 2013, 8, e77727.
- Huang, Z. An update on the regulatory status of PDT photosensitizers in China. Photodiagn. Photodyn. Ther. 2008, 5, 285–287.
- Sun, M.; Zhou, C.; Zeng, H.; Puebla-Osorio, N.; Damiani, E.; Chen, J.; Wang, H.; Li, G.; Yin, F.; Shan, L.; et al. Hiporfin-mediated photodynamic therapy in preclinical treatment of osteosarcoma. Photochem. Photobiol. 2015, 91, 533–544.
- Serra, A.; Pineiro, M.; Santos, C.I.; Gonsalves, A.M.d.R.; Abrantes, M.; Laranjo, M.; Botelho, M.F. In vitro photodynamic activity of 5,15-bis(3-hydroxyphenyl)porphyrin and its halogenated derivatives against cancer cells. Photochem. Photobiol. 2010, 86, 206–212.
- De Miguel, G.C.; Abrantes, A.M.; Laranjo, M.; Grizotto, A.Y.K.; Camporeze, B.; Pereira, J.A.; Brites, G.; Serra, A.; Pineiro, M.; Rocha-Gonsalves, A.; et al. A new therapeutic proposal for inoperable osteosarcoma: Photodynamic therapy. Photodiagn. Photodyn. Ther. 2018, 21, 79–85.
- Makhadmeh, G.N.; Abdul Aziz, A. Photodynamic application of protoporphyrin IX as a photosensitizer encapsulated by silica nanoparticles. Artif. Cell. Nanomed. B 2018, 46, S1043–S1046.
- Duchi, S.; Sotgiu, G.; Lucarelli, E.; Ballestri, M.; Dozza, B.; Santi, S.; Guerrini, A.; Dambruoso, P.; Giannini, S.; Donati, D.; et al. Mesenchymal stem cells as delivery vehicle of porphyrin loaded nanoparticles: Effective photoinduced in vitro killing of osteosarcoma. J. Control Release 2013, 168, 225–237.
- Hanahan, D.; Weinberg, R.A. Hallmarks of cancer: The next generation. Cell 2011, 144, 646–674.
- Zheng, G.; Chen, J.; Stefflova, K.; Jarvi, M.; Li, H.; Wilson, B.C. Photodynamic molecular beacon as an activatable photosensitizer based on protease-controlled singlet oxygen quenching and activation. Proc. Natl. Acad. Sci. USA 2007, 104, 8989–8994.
- Liu, T.W.; Akens, M.K.; Chen, J.; Wise-Milestone, L.; Wilson, B.C.; Zheng, G. Imaging of specific activation of photodynamic molecular beacons in breast cancer vertebral metastases. Bioconjug. Chem. 2011, 22, 1021–1030.
- Liu, T.W.; Akens, M.K.; Chen, J.; Wilson, B.C.; Zheng, G. Matrix metalloproteinase-based photodynamic molecular beacons for targeted destruction of bone metastases in vivo. Photoch. Photobio. Sci. 2016, 15, 375–381.
- Chen, R.; Zhang, J.; Hu, Y.; Wang, S.; Chen, M.; Wang, Y. Potential antineoplastic effects of Aloe-emodin: A comprehensive review. Am. J. Chin. Med. 2014, 42, 275–288.
- Vargas, F.; Rivas, C.; Medrano, M. Interaction of emodin, aloe-emodin, and rhein with human serum albumin: A fluorescence spectroscopic study. Toxicol. Mech. Methods 2004, 14, 227–231.
- Lee, H.Z.; Yang, W.H.; Hour, M.J.; Wu, C.Y.; Peng, W.H.; Bao, B.Y.; Han, P.H.; Bau, D.T. Photodynamic activity of aloe-emodin induces resensitization of lung cancer cells to anoikis. Eur. J. Pharmacol. 2010, 648, 50–58.
- Tu, P.; Huang, Q.; Ou, Y.; Du, X.; Li, K.; Tao, Y.; Yin, H. Aloe-emodin-mediated photodynamic therapy induces autophagy and apoptosis in human osteosarcoma cell line MG63 through the ROS/JNK signaling pathway. Oncol. Rep. 2016, 35, 3209–3215.
- Duchi, S.; Ramos-Romero, S.; Dozza, B.; Guerra-Rebollo, M.; Cattini, L.; Ballestri, M.; Dambruoso, P.; Guerrini, A.; Sotgiu, G.; Varchi, G.; et al. Development of near-infrared photoactivable phthalocyanine-loaded nanoparticles to kill tumor cells: An improved tool for photodynamic therapy of solid cancers. Nanomedicine 2016, 12, 1885–1897.
- Lenna, S.; Bellotti, C.; Duchi, S.; Martella, E.; Columbaro, M.; Dozza, B.; Ballestri, M.; Guerrini, A.; Sotgiu, G.; Frisoni, T.; et al. Mesenchymal stromal cells mediated delivery of photoactive nanoparticles inhibits osteosarcoma growth in vitro and in a murine in vivo ectopic model. J. Exp. Clin. Cancer Res. 2020, 39, 40.
- Yousefi Sadeghloo, A.; Khorsandi, K.; Kianmehr, Z. Synergistic effect of photodynamic treatment and doxorubicin on triple negative breast cancer cells. Photochem. Photobiol. Sci. 2020, 19, 1580–1589.
- Martinez de Pinillos Bayona, A.; Moore, C.M.; Loizidou, M.; MacRobert, A.J.; Woodhams, J.H. Enhancing the efficacy of cytotoxic agents for cancer therapy using photochemical internalisation. Int. J. Cancer 2016, 138, 1049–1057.
- Ecker, R.D.; Endo, T.; Wetjen, N.M.; Krauss, W.E. Diagnosis and treatment of vertebral column metastases. Mayo Clin. Proc. 2005, 80, 1177–1186.
- Kaijzel, E.L.; van der Pluijm, G.; Lowik, C.W. Whole-body optical imaging in animal models to assess cancer development and progression. Clin. Cancer Res. 2007, 13, 3490–3497.
- Won, E.; Wise-Milestone, L.; Akens, M.K.; Burch, S.; Yee, A.J.; Wilson, B.C.; Whyne, C.M. Beyond bisphosphonates: Photodynamic therapy structurally augments metastatically involved vertebrae and destroys tumor tissue. Breast Cancer Res. Treat. 2010, 124, 111–119.
- Hojjat, S.P.; Won, E.; Hardisty, M.R.; Akens, M.K.; Wise-Milestone, L.M.; Whyne, C.M. Non-destructive evaluation of the effects of combined bisphosphonate and photodynamic therapy on bone strain in metastatic vertebrae using image registration. Ann. Biomed. Eng. 2011, 39, 2816–2822.
- Akens, M.K.; Wise-Milestone, L.; Won, E.; Schwock, J.; Yee, A.J.; Wilson, B.C.; Whyne, C.M. In vitro and in vivo effects of photodynamic therapy on metastatic breast cancer cells pre-treated with zoledronic acid. Photodiagn. Photodyn. Ther. 2014, 11, 426–433.
- Heymann, P.G.; Ziebart, T.; Kammerer, P.W.; Mandic, R.; Saydali, A.; Braun, A.; Neff, A.; Draenert, G.F. The enhancing effect of a laser photochemotherapy with cisplatin or zolendronic acid in primary human osteoblasts and osteosarcoma cells in vitro. J. Oral Pathol. Med. 2016, 45, 803–809.
- Kotagiri, N.; Cooper, M.L.; Rettig, M.; Egbulefu, C.; Prior, J.; Cui, G.; Karmakar, P.; Zhou, M.; Yang, X.; Sudlow, G.; et al. Radionuclides transform chemotherapeutics into phototherapeutics for precise treatment of disseminated cancer. Nat. Commun. 2018, 9, 275.
- Chen, J.; Fan, T.; Xie, Z.; Zeng, Q.; Xue, P.; Zheng, T.; Chen, Y.; Luo, X.; Zhang, H. Advances in nanomaterials for photodynamic therapy applications: Status and challenges. Biomaterials 2020, 237, 119827.
- Debele, T.A.; Peng, S.; Tsai, H.C. Drug Carrier for Photodynamic Cancer Therapy. Int. J. Mol. Sci. 2015, 16, 22094–22136.
- Zhu, L.; Chen, L. Progress in research on paclitaxel and tumor immunotherapy. Cell Mol. Biol. Lett. 2019, 24, 40.
- Bernabeu, E.; Cagel, M.; Lagomarsino, E.; Moretton, M.; Chiappetta, D.A. Paclitaxel: What has been done and the challenges remain ahead. Int. J. Pharm. 2017, 526, 474–495.
- Martella, E.; Ferroni, C.; Guerrini, A.; Ballestri, M.; Columbaro, M.; Santi, S.; Sotgiu, G.; Serra, M.; Donati, D.M.; Lucarelli, E.; et al. Functionalized Keratin as Nanotechnology-Based Drug Deliv System for the Pharmacological Treatment of Osteosarcoma. Int. J. Mol. Sci. 2018, 19, 3670.
- Zhu, C.; Yan, X.; Yu, A.; Wang, Y. Doxycycline synergizes with doxorubicin to inhibit the proliferation of castration-resistant prostate cancer cells. Acta Bioch. Bioph. Sin. 2017, 49, 999–1007.
- Onoda, T.; Ono, T.; Dhar, D.K.; Yamanoi, A.; Fujii, T.; Nagasue, N. Doxycycline inhibits cell proliferation and invasive potential: Combination therapy with cyclooxygenase-2 inhibitor in human colorectal cancer cells. J. Lab. Clin. Med. 2004, 143, 207–216.
- Tong, F.; Ye, Y.; Chen, B.; Gao, J.; Liu, L.; Ou, J.; van Hest, J.C.M.; Liu, S.; Peng, F.; Tu, Y. Bone-Targeting Prodrug Mesoporous Silica-Based Nanoreactor with Reactive Oxygen Species Burst for Enhanced Chemotherapy. ACS Appl. Mater. Interface 2020, 12, 34630–34642.
- Manasanch, E.E.; Orlowski, R.Z. Proteasome inhibitors in cancer therapy. Nat. Rev. Clin. Oncol. 2017, 14, 417–433.
- Ling, Y.H.; Liebes, L.; Zou, Y.; Perez-Soler, R. Reactive oxygen species generation and mitochondrial dysfunction in the apoptotic response to Bortezomib, a novel proteasome inhibitor, in human H460 non-small cell lung cancer cells. J. Biol. Chem. 2003, 278, 33714–33723.
- Huang, Y.; Xiao, Z.; Guan, Z.; Shen, Y.; Jiang, Y.; Xu, X.; Huang, Z.; Zhao, C. A light-triggered self-reinforced nanoagent for targeted chemo-photodynamic therapy of breast cancer bone metastases via ER stress and mitochondria mediated apoptotic pathways. J. Control Release 2020, 319, 119–134.
- Lu, S.L.; Wang, Y.H.; Liu, G.F.; Wang, L.; Li, Y.; Guo, Z.Y.; Cheng, C. Graphene Oxide Nanoparticle-Loaded Ginsenoside Rg3 Improves Photodynamic Therapy in Inhibiting Malignant Progression and Stemness of Osteosarcoma. Front. Mol. Biosci. 2021, 8, 663089.
- Turubanova, V.D.; Balalaeva, I.V.; Mishchenko, T.A.; Catanzaro, E.; Alzeibak, R.; Peskova, N.N.; Efimova, I.; Bachert, C.; Mitroshina, E.V.; Krysko, O.; et al. Immunogenic cell death induced by a new photodynamic therapy based on photosens and photodithazine. J. Immunother. Cancer 2019, 7, 350.
- He, C.; Duan, X.; Guo, N.; Chan, C.; Poon, C.; Weichselbaum, R.R.; Lin, W. Core-shell nanoscale coordination polymers combine chemotherapy and photodynamic therapy to potentiate checkpoint blockade cancer immunotherapy. Nat. Commun. 2016, 7, 12499.
- Zheng, Y.; Yin, G.; Le, V.; Zhang, A.; Chen, S.; Liang, X.; Liu, J. Photodynamic-therapy Activates Immune Response by disrupting Immunity Homeostasis of Tumor Cells, which Generates Vaccine for Cancer Therapy. Int. J. Biol. Sci. 2016, 12, 120–132.
- Ji, J.; Zhang, Y.; Chen, W.R.; Wang, X. DC vaccine generated by ALA-PDT-induced immunogenic apoptotic cells for skin squamous cell carcinoma. Oncoimmunology 2016, 5, e1072674.
- Zhang, F.; Zhu, Y.; Fan, G.; Hu, S. Photodynamic therapy reduces the inhibitory effect of osteosarcoma cells on dendritic cells by upregulating HSP. Oncol. Lett. 2018, 16, 5034–5040.
- Furi, I.; Sipos, F.; Germann, T.M.; Kalmar, A.; Tulassay, Z.; Molnar, B.; Muzes, G. Epithelial toll-like receptor 9 signaling in colorectal inflammation and cancer: Clinico-pathogenic aspects. World J. Gastroenterol. 2013, 19, 4119–4126.
- Weiner, G.J. CpG oligodeoxynucleotide-based therapy of lymphoid malignancies. Adv. Drug Deliv. Rev. 2009, 61, 263–267.
- Salem, A.K.; Weiner, G.J. CpG oligonucleotides as immunotherapeutic adjuvants: Innovative applications and delivery strategies. Adv. Drug Deliv. Rev. 2009, 61, 193–194.
- Xia, Y.; Gupta, G.K.; Castano, A.P.; Mroz, P.; Avci, P.; Hamblin, M.R. CpG oligodeoxynucleotide as immune adjuvant enhances photodynamic therapy response in murine metastatic breast cancer. J. Biophotonics 2014, 7, 897–905.
- Marrache, S.; Choi, J.H.; Tundup, S.; Zaver, D.; Harn, D.A.; Dhar, S. Immune stimulating photoactive hybrid nanoparticles for metastatic breast cancer. Integr. Biol. 2013, 5, 215–223.
- Ribas, A.; Shin, D.S.; Zaretsky, J.; Frederiksen, J.; Cornish, A.; Avramis, E.; Seja, E.; Kivork, C.; Siebert, J.; Kaplan-Lefko, P.; et al. PD-1 Blockade Expands Intratumoral Memory T Cells. Cancer Immunol. Res. 2016, 4, 194–203.
- Herbst, R.S.; Soria, J.C.; Kowanetz, M.; Fine, G.D.; Hamid, O.; Gordon, M.S.; Sosman, J.A.; McDermott, D.F.; Powderly, J.D.; Gettinger, S.N.; et al. Predictive correlates of response to the anti-PD-L1 antibody MPDL3280A in cancer patients. Nature 2014, 515, 563–567.
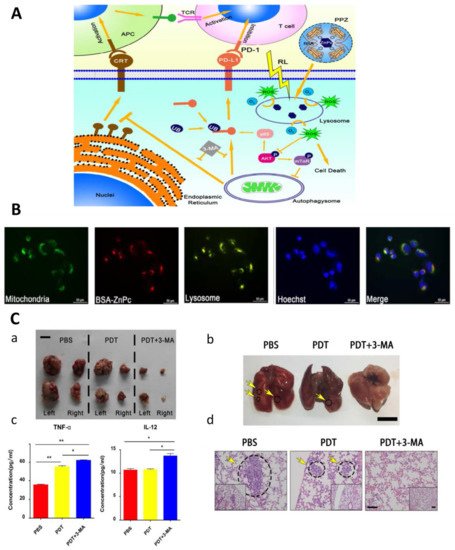
- Yu, W.; Wang, Y.; Zhu, J.; Jin, L.; Liu, B.; Xia, K.; Wang, J.; Gao, J.; Liang, C.; Tao, H. Autophagy inhibitor enhance ZnPc/BSA nanoparticle induced photodynamic therapy by suppressing PD-L1 expression in osteosarcoma immunotherapy. Biomaterials 2019, 192, 128–139.
- Yu, W.; Zhu, J.; Wang, Y.; Wang, J.; Fang, W.; Xia, K.; Shao, J.; Wu, M.; Liu, B.; Liang, C.; et al. A review and outlook in the treatment of osteosarcoma and other deep tumors with photodynamic therapy: From basic to deep. Oncotarget 2017, 8, 39833–39848.
- Harmon, B.V.; Corder, A.M.; Collins, R.J.; Gobé, G.C.; Allen, J.; Allan, D.J.; Kerr, J.F. Cell death induced in a murine mastocytoma by 42-47 degrees C heating in vitro: Evidence that the form of death changes from apoptosis to necrosis above a critical heat load. Int. J. Radiat. Biol. 1990, 58, 845–858.
- Yuen, W.F.; Fung, K.P.; Lee, C.Y.; Choy, Y.M.; Kong, S.K.; Ko, S.; Kwok, T.T. Hyperthermia and tumour necrosis factor-alpha induced apoptosis via mitochondrial damage. Life Sci. 2020, 67, 725–732.
- Nomura, J.; Yanase, S.; Matsumura, Y.; Nagai, K.; Tagawa, T. Efficacy of Combined Photodynamic and Hyperthermic Therapy with a New Light Source in an in Vivo Osteosarcoma Tumor Model. J. Clin. Laser Med. Surg. 2004, 22, 3–8.
- Yanase, S.; Nomura, J.; Matsumura, Y.; Watanabe, Y.; Tagawa, T. Synergistic Increase in Osteosarcoma Cell Sensitivity to Photodynamic Therapy with Aminolevulinic Acid Hexyl Ester in the Presence of Hyperthermia. Photomed. Laser Surg. 2009, 27, 791–797.
- Rich, S.E.; Chow, R.; Raman, S.; Liang Zeng, K.; Lutz, S.; Lam, H.; Silva, M.F.; Chow, E. Update of the systematic review of palliative radiation therapy fractionation for bone metastases. RadioTher. Oncol. 2018, 126, 547–557.
- Chow, E.; Harris, K.; Fan, G.; Tsao, M.; Sze, W.M. Palliative radiotherapy trials for bone metastases: A systematic review. J. Clin. Oncol. 2007, 25, 1423–1436.
- MA, F.; FD, V.; MH, S. Spinal radiosurgery for metastatic disease of the spine. Cancer Control. 2007, 14, 405–411.
- Lo, V.C.; Akens, M.K.; Wise-Milestone, L.; Yee, A.J.; Wilson, B.C.; Whyne, C.M. The benefits of photodynamic therapy on vertebral bone are maintained and enhanced by combination treatment with bisphosphonates and radiation therapy. J. Orthop. Res. 2013, 31, 1398–1405.
- Lo, V.C.; Akens, M.K.; Moore, S.; Yee, A.J.; Wilson, B.C.; Whyne, C.M. Beyond radiation therapy: Photodynamic therapy maintains structural integrity of irradiated healthy and metastatically involved vertebrae in a pre-clinical in vivo model. Breast Cancer Res. Treat. 2012, 135, 391–401.
- Fan, H.T.; Wang, L.; Zhang, P.; Liu, S.B. Photodynamic therapy in spinal metastases: A qualitative analysis of published results. Int. Surg. 2015, 100, 712–719.
- Okcu, M.F.; Munsell, M.; Treuner, J.; Mattke, A.; Pappo, A.; Cain, A.; Ferrari, A.; Casanova, M.; Ozkan, A.; Raney, B. Synovial sarcoma of childhood and adolescence: A multicenter, multivariate analysis of outcome. J. Clin. Oncol. 2003, 21, 1602–1611.
- Siegel, H.J.; Sessions, W.; Casillas, M.A., Jr.; Said-Al-Naief, N.; Lander, P.H.; Lopez-Ben, R. Synovial sarcoma: Clinicopathologic features, treatment, and prognosis. Orthopedics 2007, 30, 1020–1027.
- Kusuzaki, K.; Murata, H.; Matsubara, T.; Miyazaki, S.; Shintani, K.; Seto, M.; Matsumine, A.; Hosoi, H.; Sugimoto, T.; Uchida, A. Clinical Outcome of a Novel Photodynamic Therapy Technique Using Acridine Orange for Synovial Sarcomas. Photochem. Photobiol. 2005, 81, 705–709.
- Kusuzaki, K.; Murata, H.; Matsubara, T.; Miyazaki, S.; Okamura, A.; Seto, M.; Matsumine, A.; Hosoi, H.; Sugimoto, T.; Uchida, A. Clinical Trial of Photodynamic Therapy Using Acridine Orange with/without Low Dose Radiation as New Limb Salvage Modality in Musculoskeletal Sarcomas. Anticancer Res. 2005, 25, 1225–1236.
- Yoshida, K.; Kusuzaki, K.; Matsubara, T.; Matumine, A.; Kumamoto, T.; Komada, Y.; Naka, N.; Uchida, A. Periosteal Ewing’s sarcoma treated by photodynamic therapy with acridine orange. Oncol. Rep. 2005, 13, 279–282.
- Gelderblom, H.; Hogendoorn, P.C.; Dijkstra, S.D.; van Rijswijk, C.S.; Krol, A.D.; Taminiau, A.H.; Bovee, J.V. The clinical approach towards chondrosarcoma. Oncologist 2008, 13, 320–329.
- MacDonald, I.J.; Lin, C.Y.; Kuo, S.J.; Su, C.M.; Tang, C.H. An update on current and future treatment options for chondrosarcoma. Expert Rev. Anticancer Ther. 2019, 19, 773–786.
- Nhembe, F.; Jerjes, W.; Upile, T.; Hamdoon, Z.; Hopper, C. Chondrosarcoma of the hyoid treated with interstitial photodynamic therapy: Case study. Photodiagn. Photodyn. Ther. 2009, 6, 235–237.
- Burch, S.; Bisland, S.K.; Bogaards, A.; Yee, A.J.M.; Finkelstein, J.A.; Wilson, B.C.; Whyne, C.M. Photodynamic therapy for the treatment of vertebral metastases in a rat model of human breast carcinoma. J. Orthop. Res. 2005, 23, 995–1003.
- Fisher, C.; Ali, Z.; Detsky, J.; Sahgal, A.; David, E.; Kunz, M.; Akens, M.; Chow, E.; Whyne, C.; Burch, S.; et al. Photodynamic Therapy for the Treatment of Vertebral Metastases: A Phase I Clinical Trial. Clin. Cancer Res. 2019, 25, 5766–5776.
- Selbo, P.K.; Weyergang, A.; Hogset, A.; Norum, O.J.; Berstad, M.B.; Vikdal, M.; Berg, K. Photochemical internalization provides time- and space-controlled endolysosomal escape of therapeutic molecules. J. Control Release 2010, 148, 2–12.
- Berg, K.; Nordstrand, S.; Selbo, P.K.; Tran, D.T.; Angell-Petersen, E.; Hogset, A. Disulfonated tetraphenyl chlorin (TPCS2a), a novel photosensitizer developed for clinical utilization of photochemical internalization. Photoch. Photobio. Sci. 2011, 10, 1637–1651.
- Jerjes, W.; Hamdoon, Z.; Berg, K.; Hogset, A.; Hopper, C. Recurrent chondroblastic osteosarcoma of the right mandible subjected to photochemical internalization. Photodiagn. Photodyn. Ther. 2019, 27, 288–290.
