Approximately 100–400 million people from more than 100 countries in the tropical and subtropical world are affected by dengue infections. Recent scientific breakthroughs have brought new insights into novel strategies for the production of dengue antivirals and vaccines. The search for specific dengue inhibitors is expanding, and the mechanisms for evaluating the efficacy of novel drugs are currently established, allowing for expedited translation into human trials. Furthermore, in the aftermath of the only FDA-approved vaccine, Dengvaxia, a safer and more effective dengue vaccine candidate is making its way through the clinical trials. Until an effective licensed vaccine are available, disease monitoring and vector population control will be the mainstays of dengue prevention. In this review, we highlighted recent advances made in the perspectives of efforts made recently also to shed some light on the direction of the dengue vaccine development.
Dengue Vaccine Development
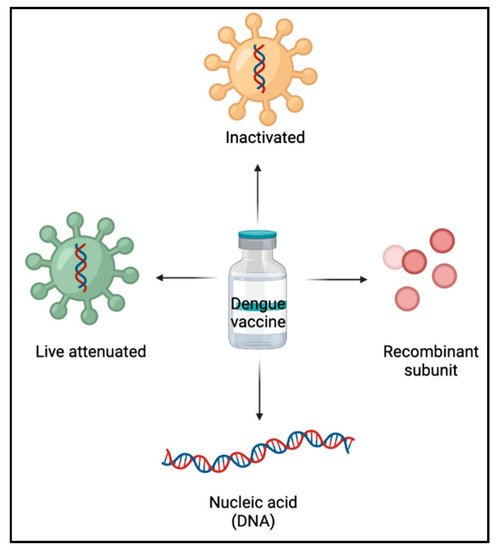
In the development of dengue vaccines, a thorough understanding of immune responses to DENV aid in the formulation of an effective approach [
16]. Live-attenuated vaccines, inactivated vaccines, recombinant subunit vaccines, and nucleic acid (DNA) vaccines are the primary forms of dengue vaccines currently under research (
Figure 1).
Figure 1. Types of dengue vaccines.
These types of vaccines confer protection by increasing the immune responses to the E protein and non-structural protein 1 of the dengue virus (DENV) (NS1). The vaccine candidates that have progressed to the clinical trial stage are summarized in Table 1 below.
Table 1. DENV vaccines currently under development.
| Vaccine Type |
Vaccine Name |
Developer |
Current Stage |
Target Antigen |
Strategy |
Key Clinical Outcome |
References |
| Live attenuated |
Dengvaxia© (CYD-TDV) |
Sanofi Pasteur |
Licensed |
Live virus |
DENV 1–4 genes substituted for the YF17D virus genes (prM/E). |
Age limit; increased risk of severe dengue in seronegative subjects but high effectiveness and safe in seropositive individuals |
[11,17,18] |
| Tetravax; TV003/TV005 |
NIH (USA); Butantan Institute (Brazil); Panacea Biotec Ltd. (India) |
Phase II/III |
Live virus |
Attenuation of DENV1, DENV3, DENV4, and a DENV2/DENV4 chimerical by excluding 30 nucleotides from the 3′ UTR. |
Well-tolerated; balanced immune response in subjects, effective with administration of a single dose. Adverse reaction (mild rash) |
[19,20] |
| TAK-003; DENVax |
Mahidol University; Inviragen; Takeda |
Phase III |
Live virus |
DENV2 PDK-53 attenuated vaccine coding sequences are replaced with DENV1, DENV3, and DENV4 coding sequences. |
Immunogenic and well-tolerated in multiple phase I and II clinical studies, independent of the participants’ age or serostatus, safety profile not entirely known |
[21] |
| TDEN F17/F19 |
WRAIR and GSK |
Phase II |
Live virus |
Involving primary cells of dog kidney (PDK) and lung cells of fetal rhesus (FrhL) in serial passages |
Proven to be a safe, well-tolerated, and immunogenic DENV vaccine candidate in phase II trial |
[22,23] |
| Inactivated |
TDEV-PIV |
GSK, Firocruz and WRAIR Merck |
Phase I |
Inactive virus |
Employing adjuvants and purified formalin-inactivated virus |
Well-tolerated, immunogenic in naive and seropositive individuals. No risk of re-activation and good immuno-logical balance |
[24,25] |
| Recombinant subunit |
V180 |
GSK, Firocruz and WRAIR Merck |
Phase I/II |
80% of the E protein |
DEN-80E-containing recombinant truncated protein |
Induce steady immune responses against all DENV serotypes, decreasing the likelihood of the ADE effect |
[26,27] |
| Nucleic acid (DNA) |
TVDV |
U.S Naval Medical Research Centre |
Phase I |
prM and E proteins |
prM/E proteins are encoded via a recombinant plasmid vector |
Stable but lack of immunogenicity. Plasmid modification required. |
[28,29] |
| D1ME100 |
US Naval Medical Research Center |
Phase I |
prM and E proteins |
recombinant plasmid vector encoding prM/E |
No neutralizing antibody response detected in individuals with low-dose immunization |
[30] |
1. Live-Attenuated Vaccines
Antigenic compounds synthesized from a living pathogen that has been engineered to be less virulent or avirulent are known as live-attenuated vaccines. Once administered, the viruses multiply locally, eliciting neutralizing antibodies and cell-mediated immune responses against the four dengue virus serotypes. These vaccines demonstrate the benefits of delivering protective antigens while offering long-term immune protection [
31]. Using recombinant DNA technology, several live dengue attenuated vaccines have been developed.
Dengvaxia, also known as CYD-TDV, is the only approved tetravalent live-attenuated dengue vaccine candidate [
11,
17,
18]. Receiving FDA approval in 2015, this vaccine is now accessible in more than 20 countries. Its usage has been allowed with strict restrictions on the recipients’ age and serostatus [
32]. It offers high effectiveness in preventing dengue disease caused by DENV serotypes 1–4 and is safe in people who have had a past dengue infection, i.e., those who are seropositive. To date, the FDA has approved the usage in individuals 9 through 16 years of age with laboratory-confirmed previous dengue infection and living in endemic areas [
33]. However, for those who are seronegative, the vaccine increases the chance of having severe dengue when the person has a spontaneous dengue illness about 3 years following immunization. Vaccination in the naive subjects stimulates the development of neutralizing antibodies against all four DENV serotypes. Specific antibodies against one or a few serotypes dominate this response, whereas reactions against the other serotypes are mostly due to cross-reactive antibodies. Moreover, it produces serotype-specific and cross-reactive T cell responses against DENV structural antigens. Therefore, the seronegative individuals may thus constitute a subclinical attenuated ‘primary-like’ illness. Vaccination in this group also results in different immunological effects depending on the serotypes. When compared to cross-protection evoked by vaccination in seropositive individuals, minimal cross-protection in seronegative individuals can be observed, posing a greater risk of inducing antibody-dependent enhancement (ADE) [
34,
35,
36]. Consequently, WHO recommends that this vaccine is only given to seropositive individuals.
Tetravax (TV003/TV005), on the other hand, differs significantly from CYD-TDV in terms of the viral particle structure, infectivity, and immunogenicity [
20,
37]. To reduce DENV virulence, researchers utilized three untranslated regions (UTRs) deletions and structural gene prM/E chimerization. In comparison to TV003/TV005, CYD had a greater risk of viremia, lesser dengue virus type 2 resistance, and a reduced level of adaptive immune response [
37].
TAK-003, often known as DENVax, is a live-attenuated chimeric tetravalent dengue vaccine [
21]. At present, it is still in phase III of clinical investigations. The backbone of this vaccine is a weakened DENV2 strain (PDK-53) that contains the prM/E parts of all serotypes. The vaccine was proven to be immunogenic and well-tolerated in multiple phase I and II clinical studies, independent of the participants’ age or serostatus. TAK-003 showed a DENV serotype-dependent protective effectiveness, similar to its predecessor Dengvaxia, but with higher levels of DENV2 neutralizing antibodies and lower DENV3 and DENV4 protection rates, consequently, its safety profile is not entirely known [
38]. Although a previous clinical study indicated it triggers CD8+ T lymphocytes directed at NS1, NS3, and NS5 in patients that have never been infected with DENV [
39], this data were not included in later clinical studies.
In addition to live-attenuated dengue vaccines is TDEN F17/F19 [
22,
23]. In a phase II trial, this vaccine was proven to be a safe, well-tolerated, and immunogenic DENV vaccine candidate. One month following the second dosage, antibody responses to all four DENV types were recorded in more than half of the infants/toddlers and all of the children [
40]. The vaccines used in these studies were lyophilized monovalent vaccines that were combined into a tetravalent vaccine at the point of administration.
Conclusively, based on the experiences obtained during the development prospective live-attenuated vaccines, the WHO have highlighted the guidelines on the quality, safety, and efficacy of the dengue tetravalent vaccines (live, attenuated). Furthermore, according to FDA, dengue live-attenuated vaccine, particularly Dengvaxia, elicits dengue-specific immune responses against the four dengue virus serotypes after injection. However, the exact mechanism of protection has yet to be discovered [
33].
2. Inactivated Vaccines
Inactivated vaccines are antigenic compounds made up of denatured substances from other microbes such as bacteria and viruses that can provide protection against the live pathogen [
41]. This vaccine stimulates immunity by using antigens from the capsid (c), membrane (M), envelope (E), and non-structural 1 (NS1) protein, although composite vaccinations provide superior protection compared to single-type immunizations.
The tetravalent purified formalin-inactivated virus (TPIV), which contains four non-active dengue serotypes, is an example of an inactivated vaccine now in clinical trials [
42]. TDENV PIV/AS03B is now being investigated in a clinical study with various dosing regimens [
24,
25]. In both flavivirus-naive and experienced groups of infected individuals, TDEV PIV was well tolerated and immunogenic. Furthermore, this type of vaccine is safer than live-attenuated vaccines since there is no risk of reactivation and immunological balance is better regulated.
3. Recombinant Subunit Vaccine
Following the failure and controversy surrounding Dengvaxia
®, recombinant subunit vaccination options have regained some interest. In this type of immunization, antigenic proteins produced by prokaryotic or eukaryotic cells generate long-lasting protective/therapeutic immune responses [
43]. By far the most prevalent DENV recombinant subunit candidates are the envelope E protein or shortened variants. These rely on the formation of neutralizing antibodies to prevent DENV from infecting its host cells.
Despite the ease with which recombinant dengue proteins may be expressed in
E. coli, there are potential concerns of being exposed to endotoxin contaminants and protein misfolding [
44]. V180, which is made up of a shortened version of the protein DEN-80, is the most promising subunit vaccine [
26,
27]. Recombinant subunit vaccinations are more likely than live-attenuated vaccinations to induce steady immune responses against all DENV serotypes, decreasing the likelihood of the ADE effect [
35].
4. DNA Vaccine
In the development of DNA vaccines, no less than a gene encoding specific antigens were incorporated into the plasmid. The E glycoprotein anchored to the prM protein mediates the first interaction between DENV and host cells, hence, it becomes the primary target for inducing neutralizing antibodies. Through in vivo injection of the expressed antigens, the vaccines induce both arms of the immune system which are the T cell responses and antibody production [
45].
D1ME100 is an example of a DNA vaccine that has been clinically tested on
Aotus nancymaae monkeys and humans [
30,
46]. In the initial phase of immunization, the vaccine proved to be safe and tolerable. Notwithstanding, with only about half of those who had high-dose immunization producing neutralizing antibodies, this immunogenicity produced was found to be weak. Furthermore, in those who received low-dose immunization, no neutralizing antibody response was detected [
28]. Another example is the tetravalent dengue vaccine (TVDV), which is made up of four plasmids carrying the prM and E encoding genes from each DENV serotype [
28,
29]. The robust DENV-specific IFN T-cell response generated in 79% of the highest vaccination dosage recipients [
29], however, is cause for concern. Despite its lack of immunogenicity, this vaccine has been shown to be stable, simple to make, inexpensive, and large-scale production. Plasmid modification with extremely efficient promoters, alternative delivery strategies, multiple doses, and co-immunization with adjuvants are recommended as solutions to the drawbacks of this form of vaccination.
An Ideal Vaccine against Dengue
Despite the fact that a dengue vaccine is now available, which is an important step forward, the long-lasting protective efficacy against each of the four dengue virus serotypes has yet to be confirmed. The characteristics of DENV, as well as the immunological protection and pathologic processes involved, including the transmission and epidemiology of dengue illness, have all hindered the development of a dengue vaccine. Vaccine development also has encountered conceptual problems since its inception, including the biology of the viruses that cause it, immunological protection and pathogenesis processes, and transmission and epidemiology.
Moreover, in endemic regions, the establishment of a protective antibody response against the infection is acquired through recurrent viral exposure. After being infected with one of the four DENV serotypes, the patient can be infected with any of the other serotypes. However, the infected individuals most likely do not manifest the clinical symptoms as a consequence of cross-protection.
The ideal dengue vaccine is abridged from the fact that it must elicit a multitypic response similar to that of people living in endemic areas, aided by persistent exposure and perhaps symptomatic or asymptomatic reinfection. An explicit elaboration on factors influencing vaccine responses, such as the pre-vaccination environment, as well as the significant challenges that face the development of an efficient/protective dengue vaccine, such as the presence of multiple serotypes, ADE, and cross-reactivity with other flaviviruses, have also been discussed to enhance the search of reliable dengue vaccine [
47]. Hence, we concluded the key barriers to dengue vaccine development include a lack of a proper mechanistic investigation in pathogenesis and ADE.
This entry is adapted from the peer-reviewed paper 10.3390/molecules26226768