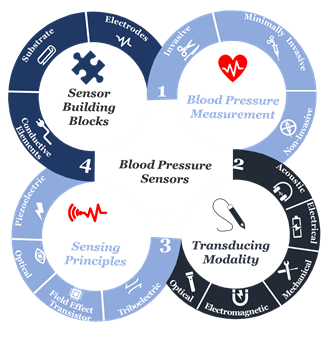
In our unique transdisciplinary approach, we studied the fundamentals of blood pressure and examined its measuring modalities while focusing on their clinical use and sensing principles to identify material functionalities. Then, we carefully reviewed various categories of functional materials utilized in sensor building blocks allowing for comparative analysis of the performance of a wide range of materials throughout the sensor operational-life cycle. Not only this provides essential data to enhance the materials’ properties and optimize their performance, but also, it highlights new perspectives and provides suggestions to develop the next generation pressure sensors for clinical use.
- Blood Pressure Sensors
- wearable sensors
- sensing materials
- smart health monitor devices
- sensor operational lifecycle
Advancements in materials science and fabrication techniques have contributed to the significant growing attention to a wide variety of sensors for digital healthcare. While the progress in this area is tremendously impressive, few wearable sensors with the capability of real-time blood pressure monitoring are approved for clinical use. One of the key obstacles in the further development of wearable sensors for medical applications is the lack of comprehensive technical evaluation of sensor materials against the expected clinical performance. Here, we present an extensive review and critical analysis of various blood pressure approaches, sensing and transducing principles, as well as materials applied in the design and fabrication of wearable sensors.
-
Introduction
Cardiovascular diseases caused 31% of deaths worldwide [1], and recently, they had the highest confirmed death cases in Italy and China during the novel pandemic known as the coronavirus disease 2019 (COVID-19) [2,3]. In return, the demand for an accurate home-diagnostic tool for blood pressure measurements, along with other vital signs (e.g., temperature, respiratory rate) has increased massively. These tools, especially if enabled with telemedicine, will not only help assess a patient’s health status, triage the patient to appropriate care, determine potential diagnoses, and predict recovery, but also, it will help provide real-time medical monitoring, for instance, people in home-quarantine [4,5]. Hence, improving the precision and accuracy in blood pressure measurements can help significantly with early diagnosis and cardiovascular risk stratification [6–9], because inadequate performance in blood pressure measurement will increase current levels of fatal stroke and fatal myocardial infections [10], as well as impose an avoidable financial burden [11].
At the beginning of the twenty-first century, the use of sensors and mobile internet begins to provide a platform to continuously monitor all vital signs [12–20], including blood pressure. Not only does this help reduce the risk of cardiovascular complications, but also it supports making accurate and real-time healthcare data available for healthcare professionals at the office to assist select the best treatment strategies and consider the impact on patient outcomes [21–26]. Furthermore, this type of monitoring can save millions of lives around the globe annually [27–29]. Advancements in engineering and material science have been the main driver in the development of sensor technologies during the past decade [29–31]. Indeed, tactile sensors, and more precisely, skin-like soft electronics begin to transform healthcare [32–34]. In return, several studies highlight the crucial implications of this field and indicate that a timely review is necessary [35–37]. Since most studies focus on device functionality [38-40 ]., there is a need to investigate device clinical performance and capabilities beyond proof-of-concept measurements outside of the laboratory [41], following standardized evaluation approaches [42]. By precisely studying the unique nature of medical needs and evaluating the functionality of sensing principles and materials, we will comprehensively identify materials’ properties and their associated performance in line with structure strategies needed for accurate and continuous blood pressure measurement. Also, we will identify challenges along with future research opportunities. We aim to create a crosslink between healthcare practice and material science following a transdisciplinary approach illustrated in (Figure 1) to emphasize the importance of design and fabrication elements that have been either overlooked or compromised.
Figure 1. The transdisciplinary approach for the comprehensive review of the recent development in biomaterials used for an accurate yet continuous blood pressure measurement.
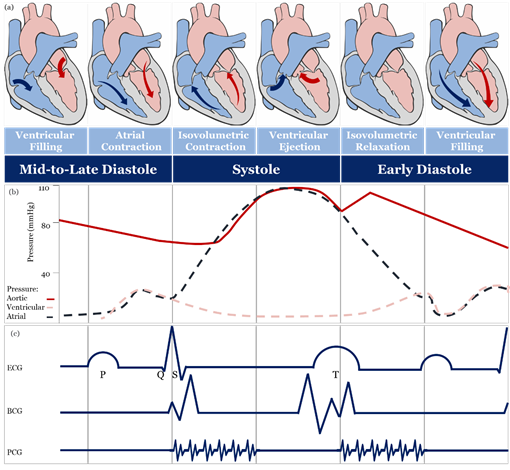
2. Blood Pressure Measurement
The theoretical and practical framework behind accurate blood pressure measurement is complex and, sometimes, overlooked entirely [43], therefore, understanding the effect of different approaches for blood pressure measurement is essential for developing accurate sensing materials suitable for medical use. The volume of blood ejected by the heart into the arteries, the elastance or stiffness of the walls of the arteries, and the rate at which the blood flows out of the arteries altogether affect blood pressure measurement [44]. During the cardiac cycle (Figure 2a,b), systolic pressure occurs as blood is ejected out of the heart and into the arteries, and diastolic pressure is created when the heart rests between heartbeats [43–45].
Figure 2. Schematic diagrams: (a) cardiac cycle, (b) arterial blood pressure versus ventricular and atrial blood pressure values, (c) morphological shapes of different signals associated with blood pressure.
2.1. Invasive and Minimally Invasive Blood Pressure Measurement and Materials
Invasive blood pressure is directly measured by an intravascular catheter unit, which comprises of three main components: an intra-arterial cannula, an infusion tube, and a transducer [52,53]. The invasive approach is accurate and free of operator bias. Indeed, it is considered the gold standard for all other measures [67,68].Minimally-invasive blood pressure measurement is based on nonvascular implantable miniaturized sensors that are compatible with body tissues, and these devices can provide real-time monitoring of the cardiac cycle [69], including intravascular [70], intraocular [71] and intracranial [72]. The accuracy of a minimally invasive approach, in contrast to the invasive, is still controversial, and it may be due to the drift in sensitivity over a long time that affects long-term accuracy [75].
2.2. Non-Invasive Blood Pressure Measurement and Materials
The full-occlusion technique includes auscultatory [76], oscillometry [77], and palpatory [78]. Auscultatory and oscillometry are comparable to a gold standard [6,79], unlike palpatory, which is not used because obtaining a diastolic blood pressure measurement is difficult and may lead to considerable error [78]. The accuracy of the oscillometry method can be highly affected by muscle contraction, noise artifacts, artery stiffness, age, and physical health [76], hence, validation and recalibration are crucial [6,76]. Auscultatory and oscillometry methods are intermittent [80] and different cuff types [81–86] and fabrics [87–91] may lead to different blood pressure measurements [92,93].
Semi-occlusion technique includes applanation tonometry [94–97], originally applied for monitoring intraocular blood pressure in glaucoma patients [98] using a Goldmann Applanation Tonometer [99] and quite recently contact lens-based sensors [100–102], and extended to include blood pressure measurement of the radial artery based on anisotropic conductive film [103] or a silicon-based MEMS sensing chip [104]. The accuracy of applanation tonometry is controversial, as it is highly dependent on artery location and changes in contact force required to maintain artery in an applanated status over time [105,106]. The volume clamp method of Peńăz, also known as vascular unloading, is a continuous blood pressure measurement [107], in which volumetric change in blood flow in a finger during the cardiac cycle is kept unchanged using a high-speed servo pump connected to a finger cuff and checked by a finger mounted photoplethysmography (PPG) sensor [108–113]. Several clinical studies demonstrated the accuracy and reproducibility of volume clamp methods [108,114], however, their accuracy is still controversial because different finger-cuff types [110–112] and fabrics [113] may lead to different blood pressure readings. The broad assumptions behind the use of the PPG sensor [115] and the underestimation of the effect of the significant difference in hydrostatic blood pressure between the finger and the heart may lead to an increase in inaccuracy [116,117]. Besides, the volume clamp method requires recalibration at regular times leading to an overestimation of systolic pressure [118]. It is recognized that the finger-cuff can be uncomfortable for patients, especially patients suffering from edema or patients with impaired peripheral blood flow [119,120].
No-occlusion blood pressure measurement includes blood flow, pulse wave, and stroke volume methods. In the blood flow method, blood pressure is estimated utilizing the bifurcated or diseased artery geometry and the pulsatile blood flow equations [121]. The pulse wave method is a simplified form of pulsatile blood flow equations under certain assumptions is used [122]. In the stroke volume method, mean arterial blood pressure is estimated through measuring changes in the volume of blood pumped from the left ventricle (i.e., cardiac output) and the resistance that must be overcome to push blood and create flow in arteries (i.e., systemic vascular resistance) or through estimating cardiac output from O2 consumption levels [123]. The accuracy of the contact [124,125] and non-contact [126–128] sensing modalities of the blood flow method is controversial. Contact sensing has met the gold standard level of accuracy under certain conditions and failed to meet it under others, whereas non-contact sensing modalities show a significant reduction in diagnostic performance [127,128]. Likewise, a non-invasive form of FFR (i.e., FFRCT) has been described, with some studies showing that it is safe and feasible [129] and with others showing that current clinical trial data are insufficient to make a recommendation for its use in clinical practice [130–132].
Sensors based on stroke volume methods, including wearable ICG/ECG, are widely used [133]. The wearable ICG/ECG includes flexible dry electrodes made of a Ti-Au composite [134], a Ni-P plated polyester fabric [135], Ag flakes with MWCNT/PDMS composite [136], a woven fabric treated with PEDOT:PSS [137] and an Ecoflex-Ag MPs self-adhesive micropillar electrode inspired by gecko and grasshopper feet [138]. Furthermore, they can be fabricated of an EPDM rubber electrode containing various additives such as carbon, stainless steel fibers, and CNT [139].
Wearable ICG/ECG performance depends on the design and fabrication of high sensitivity electrodes and the continuous contact with skin, as well as their location when placed on the human body surface [139]. Also, their accuracy is mainly associated with the level of calculation complexity, which requires many mathematical assumptions, as well as measurement and physiological artifacts [108,140].
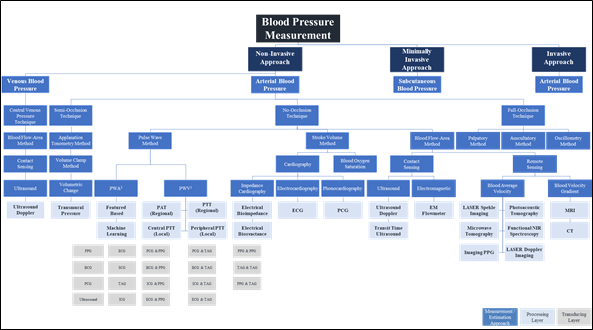
The pulse wave method is widely used in wearable and wireless applications due to its ability to integrate with a wide variety of transducers used in sensor application architectures. In addition to the effect of changes in measurement and physiological artifacts [141] and the pulse wave method does not collectively consider the impact of changes in physiological factors in blood viscosity, vascular wall elasticity, peripheral resistance of the arterial tree, and morphological characteristics in pressure pulse wave that vary regularly [142]. Figure 4 depicts the landscape of blood pressure measurement, approaches, methods, processing, and transducing modality layers, and Table 1 summarizes our analysis findings and highlights areas for further investigation.
Figure 3. Blood pressure measurement landscape; approaches, methods, processing, and transducing layers. 1 PWA: At least a single pulsatility sensor or a single cardiovascular sensor is implemented; 2 PWV: At least two pulsatility sensors and/or additional cardiovascular sensor is implemented.
Non-invasive methods—with no-occlusion blood pressure measurements based on wearable devices—offer a promising future. Failing to choose the right materials for the fabrication of wearable devices can lead to either high noise in the received signal, which affects accuracy, or red and itchy rash in the skin caused by direct contact of the materials or even an allergic reaction to a body part causing highly frequent diseases that are clinically referred to by contact dermatitis [143]. Long direct contact of skin with medically unsuitable wearable device materials can foster an attractive and supportive environment for harmful microbiota, increasing the risk of infectious skin diseases, especially amongst patients with chronic diseases [144,145].
3.Sensing Principles
Sensing principles used in blood pressure sensors include; Piezoelectric, Piezocapacitive, Optical, Field Effect Transistor (FET), and Triboelectric. Figure 4 illustrates the mechanism of each of the fundamental sensing principles studied in this review.
Figure 4. Fundamental sensing principles used in sensors
4.Sensor Building Blocks
5.Operational Lifecycle
6.Outlook
Biomaterials have attracted considerable attention due to their exceptional performance and are, therefore, well-received as one of the future building blocks of digital healthcare. For blood pressure measurements and real-time monitoring, wearable sensors have not comprehensively reached a medically accepted level of functionality to replace intermittent cuff-based devices. This gap has been seemingly associated with a disconnect between the two knowledge areas, particularly, blood pressure measurement approaches and their related modalities at one side, and functional materials design and fabrication strategies and their relevant sensing mechanisms at the other one.
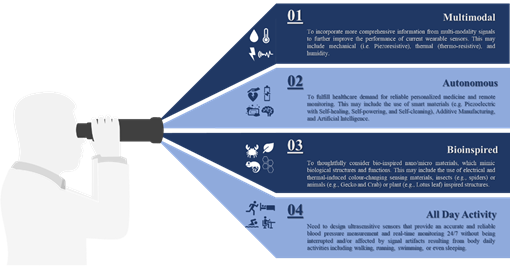
Invasive and minimally invasive blood pressure measurement does not support continuous measurement and real-time monitoring. Hence, ECG and PPG signals are mostly used to monitor health status without disturbing the users during daily activities. It would be beneficial to incorporate more comprehensive information collected from multi-modality signals such as mechanical (i.e., piezoresistive), thermal (i.e., thermoresistive), or even humidity to further improve the performance of current wearable sensors rather than considering a single sensing principle as illustrated in this review.
Apart from the rapid development demonstrated in this review, there is a bright future for tactile sensors utilizing smart materials (e.g., piezoelectric, self-healing, self-powering, self-cleaning), additive manufacturing, big data analytics (e.g., artificial intelligence) and cloud computing to fulfill healthcare demand for personalized medicine and remote monitoring. We found that sensitivity was the focus for most of the developed devices [247–249,251,257–260,274–285] and those with piezoresistive mechanisms generally showed high performance when compared with others [242,259,271,283,293]. Although piezocapacitive-based sensors still show excellent detectability and sensitivity, they are more susceptible to noise resulting from field interaction and fringing capacitance, as well as, other factors such as temperature [192,247,294,614]. FET-based sensors show high sensitivity with excellent response time due to their perfect functionalities of signal transduction and amplification, but their flexibility measured under continuous cycles of loading/unloading, is still a challenge [224,269,270,278] while the best performing device of this category shows a tiny bending radius lower than 0.02 cm with no significant variation in its electrical characteristics after more than 200 cycles [209] a piezoresistive-based sensor with a similar sensitivity can show consistent performance under continuous cycles of loading/unloading on the order of thousands. Also, FET based sensors require relatively higher operating voltage when compared to that of piezoresistive. This variation in performance should be considered as a motive, not only for further development of existing sensing principles but also for further investigation of novel mechanisms to go beyond meeting high sensitivity requirements to include linear performance without hysteresis.
The high sensitivity requirements have been achieved through the effective utilization of newly developed functional materials, such as PVDF/rGO [251] or ultrathin NWs [289], the optimization of device geometry, such as the design inspired by insects’ sensing capabilities [240] or plant leaves’ morphology [242] or the microstructure of human skin [282]. Other strategies include the reduction of active materials concentration in nanocomposite matrix through alignment [260], the utilization of novel additives manufacturing techniques such as LIG [271], or the imprinting technique to control the patterns and orientation of functional materials by template restriction [290]. The design and fabrication of wearable sensors with autonomous capabilities include wireless transmission [615,616] self-powered [220,617], self-healed [485] and self-degraded [519] will certainly enable continuous diagnosis of cardiovascular disease. However, these features and similar ones are no longer considered desirable, but they are becoming as crucial as other performance measures since they will allow automatic reparation of device malfunctions and disposal. Furthermore, the integrated sensing modality of tactile, temperature, and humidity [420,456,618,619] to extract additional features from other signals (e.g., respiratory) [620] with accuracy under the interface of strong body movement in real-time [621], will boost the performance of pressure measurements.
The performance of wearable sensors, capitalizing on the recent advancement in machine learning and cloud computation, can be further boosted by selecting optimal features that can contribute to dynamic blood pressure changes. In return, this will provide an accurate blood pressure measurement noninvasively and continuously, help enable early prevention and personalized treatment of hypertension, and reduce its burden on society. Finally, there is an essential need for a multidisciplinary approach encompasses of different knowledge areas, mainly, data, material, medical, and engineering sciences to ensure seamless integration between various sensor components and architecture, and address other challenges associated with sensor overall performance, as well as, evaluate the impact of each on device reliability and efficiency. Figure 6 summarises future development in blood pressure measurement and real-time monitoring.
Figure 7. Summary of future development in the field of blood pressure measurement and real-time monitoring.
This entry is adapted from the peer-reviewed paper 10.3390/s20164484