Heat-related illness - more commonly known as "heat stroke" - is a potentially fatal disorder that can affect both man and animals. The condition has two main causes: exertional and environmental heat. Exertional heat-related illness occurs either when a dog is active in a hot environment, or associated with strenuous and typically prolonged activity in any temperature. Environmental heat-related illness occurs when the ambient temperature and humidity increase beyond the dog's cooling limits, cases of environmental heat-related illness typically occur during heatwave events.
- canine heatstroke
- heat‐related illness
- exertional hyperthermia
1. Introduction
Heat-related illness (HRI) is a potentially fatal condition affecting man and animals, and is predicted to become more frequent as climate change increases the severity and regularity of heatwave events [1]. Rising global temperatures require human populations to consider mitigation strategies in order to survive; these could include migration away from the hottest regions [2] or adaptations to hot environments such as air cooling mechanisms and changes to working practices to reduce the risk of HRI when working outside [3]. Domestic dogs intertwine with every aspect of human society, providing both companionship and essential working services such as hearing and visual assistant dogs, medical detection dogs and military working dogs [4]. Greater understanding of the risk factors for HRI in dogs can provide a solid evidence base on which to develop adaptations to protect dogs as global temperatures continue to rise.
Heat induced illnesses were previously defined by the terms "heat cramps", "heat exhaustion" and "heat stroke", largely distinguishable as separate conditions defined by the patient's body temperature and neurological status [5]. Recent studies have suggested a novel staging system for humans - the Japanese Association of Acute Medicine Heat-Related Illness Classification - which recognises that heat-related illness is a progressive disorder [6][7]. The novel staging system describes three stages, ranging from mild (stage I) to severe (stage III) HRI. This classification acknowledges that a patient with stage I HRI will progress to stage II if they are not treated appropriately or continue to be exposed to a heat source [7]. Whilst the applicability of this novel classification to dogs has not yet been explored, it is likely dogs with HRI experience a similarly progressive disorder.
Two main triggers are identified for HRI in humans: exertional and environmental [5]. Exertional HRI typically follows prolonged, intense exercise in any temperature, or even limited exercise or physical labour in a hot environment [5][8]. Environmental HRI, sometimes referred to as classic or non-exertional HRI, occurs after prolonged exposure to high ambient temperatures or short exposure to extreme heat [9]. Young children and babies are at risk of a subtype of environmental HRI - vehicular HRI - following confinement in a hot vehicle after being left or after accidentally locked inside the vehicle [10]. In humans, exertional HRI most commonly affects young active men either working in physically demanding industries or participating in sports [11]. Exertional HRI is the third leading cause of death in US high school athletes, and the incidence of HRI in the US Armed Forces has been gradually increasing since 2014 [12]. Conversely, environmental HRI typically affects the socially vulnerable, the elderly or people with chronic medical conditions, who may be confined indoors and less able to thermoregulate or adapt [13][14].
Studies from Israel [15][16][17][18] and the UK [19] suggest exertional HRI as the predominant trigger of heatstroke in dogs, whilst a German veterinary hospital reported more vehicular HRI cases [20], and a study from Philadelphia USA reported roughly equal numbers of environmental and exertional canine HRI [21]. Dogs are likely to share similar risk factors to humans for the various types of HRI. Understanding the predominant triggers for HRI in dogs and identifying risk factors for different types of these HRI events, may improve both early recognition and prevention of HRI in dogs.
2. Incidence and fatality rates
Whilst HRI is reported as a relatively common condition in dogs living in hot or tropical climates [15], these reports are from veterinary hospitals, often receiving referrals from a large geographical locations and thus are potentially poorly representative of the general canine population [2]. Conversely a large scale UK study reported the 2016 HRI incidence of 4 in 10,000 (0.04%), from a denominator population of over 900,000 dogs presenting to primary-care veterinary practices [23]. Whether it was the primary-care based population or the temperate UK climate that resulted in a comparatively lower incidence of HRI is unclear; however, as climate change accelerates the frequency and intensity of heatwaves [24] the number of dogs affected by HRI is likely to increase dramatically.
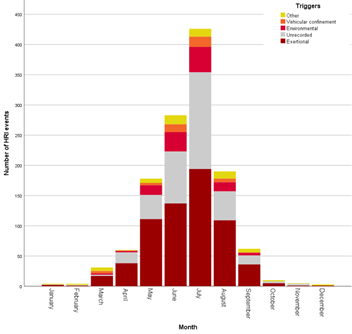
Whilst HRI predominantly affects dogs in the traditionally warmer summer months, it can occur all year round [19]. In the UK exertional HRI can occur all year round (Figure 1), whilst fatalities typically occur between March and October, one exertional HRI fatality has been reported in January [19]. Exertional HRI events in UK dogs were predominantly triggered by relatively low intensity exercises, namely walking and playing [19]. In the UK, vehicular and environmental HRI have only been recorded between March and September, coinciding with the period where internal vehicle temperatures have been recorded exceeding 35 °C [25].
Figure 1. Histogram showing the number of heat‐related illness events by trigger, per month in UK dogs between 2016-2018 [19].
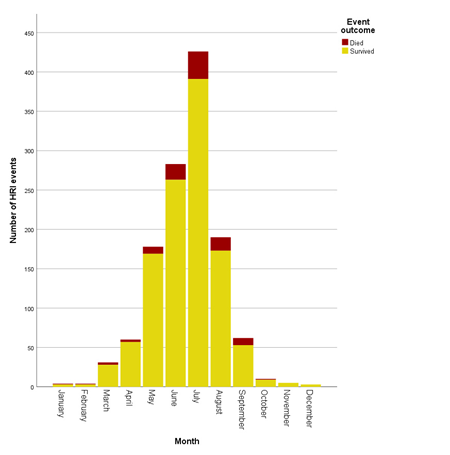
Reports of fatality rates for dogs with HRI treated at referral hospital populations range from 36-50% [15][20][21], these studies generally included dogs with the most severe form of HRI (commonly referred to as heat stroke), and were typically from hotter climates. A fatality rate of 14% (1 in 7 affected dogs) was reported from the UK based primary-care study [23], which included dogs with all three stages of HRI severity. In the UK, around a third of HRI fatalities have been reported to occur in July, typically the warmest month (Figure 2).
Figure 2. Histogram showing the number of heat‐related illness events by outcome per month in UK dogs between 2016-2018 [19].
3. Canine risk factors for HRI
3.1 Breed
The following breeds have been reported with increased risk of HRI:
- Bulldog [15][21][23]
- Chow Chow [23]
- French Bulldog [23]
- Dogue de Bordeaux [23]
- Greyhound [23]
- Cavalier King Charles Spaniel [23]
- Pug [23]
- English Springer Spaniel [23]
- Golden Retriever [15][23]
- Labrador Retriever [15]
- Belgian Mallinois [15]
The Labrador Retriever, Chow Chow, Bulldog, French Bulldog, Greyhound, English Springer Spaniel, Cavalier King Charles Spaniel, Staffordshire Bull Terrier, Boxer, Golden Retriever and Border Collie have all be identified at particularly at risk of exertional HRI [19]. The Chow Chow, Bulldog, Pug and French Bulldog are also at greater risk of environmental HRI, and the Bulldog, Greyhound, Cavalier King Charles Spaniel, French Bulldog and Pug are at greater risk of vehicular HRI [19]. No breeds have been identified with a reduced risk of HRI in general likely because HRI requires extrinsic input where affected dogs must be exposed to a hot environment and/or an activity that significantly increases body temperature in order to develop the disorder [23]. The Chihuahua was identified as having reduced odds for exertional HRI compared to crossbred dogs [19]. This is likely to be partly due to their small body size and also potentially as a result of their status as a "handbag dog", meaning they are perhaps more likely to be carried than walked [26].
3.2 Skull shape
Brachycephalic (flat-faced) dogs have been identified with greater odds for exertional, environmental and vehicular HRI [19]. A third of owners recognise that their brachycephalic dogs struggle to regulate their temperature [27]. Unlike humans, dogs do not use sweating as a primary cooling mechanism [28], but instead rely on evaporative heat loss through panting, with inspired air passing over nasal mucosa that acts as the primary site of evaporative heat loss [29]. Brachycephalic dogs have shortened muzzles, that dramatically reduce the surface area for effective evaporative cooling. Dogs affected by Brachycephalic Obstructive Airway Syndrome (BOAS), often have narrowed nostrils, larynxes and tracheas that further increases the resistance to air flow during respiration [30]. This resistance results in increased muscular effort required for effective ventilation, meaning affected dogs may generate more heat trying to breathe, than they lose via panting. Respiratory diseases such as BOAS have been shown to accelerate the increase in body temperature during exercise [31] and promote greater odds of developing HRI compared to dogs with longer muzzle [23].
3.3 Body weight
Elevated body weight can be due to either increased lean muscle mass, or increased body fat. As muscles generate heat during exercise, dogs with greater muscle mass develop higher body temperatures during exercise [32][33]. Increased fat deposition limits conduction and radiation of heat from the surface of the skin, and can also limit effective cooling via respiration by reducing tidal volume [34]. Overweight animals also overheat faster and take longer to cool [35]. Obesity has been reported as an important risk factor for death in dogs with HRI [15], and dogs with a bodyweight above the relative breed/sex mean have been reported at increased risk for HRI compared to dogs that weighed below the breed/sex mean [23]. Dogs weighing over 50kg appear to have the greatest risk of HRI in general [23], whilst all dogs weighing over 10kg have increased risk of exertional HRI when compared to dogs weighing 10kg or under [19]. Smaller dogs have a higher heat storage to radiative surface area ratio than large dogs, meaning they can cool more effectively and exercise for longer before overheating [36][37].
3.4 Age
Similar to human risk factors for HRI, the risk of different types of HRI varies between dogs of different ages. Young active dogs are at greater risk of exertional HRI, whilst dogs 12 years old or over are at greater risk for environmental HRI [19]. Older dogs are more likely to suffer from underlying health conditions such as heart diease that reduce thermoregulation [38], and that could increase the likelihood of environmental HRI [39]. In humans, advancing age increases environmental HRI risk due to reduced physiological thermoregulation ability, namely reduced sweat production and decreased blood flow to the skin [40]. Similarly impaired cooling mechanisms are also likely to affect older animals.
3.5 Sex and neuter status
Reflecting the male predisposition to exertional HRI in humans, male dogs develop a higher body temperature than females during intense exercise [32][33], and are at increased risk of exertional HRI [19]. Neutered female dogs have also been identified as having increased risk of exertional HRI compared to entire females [19], although the precise mechanism behind this is not yet fully understood. Females may be at reduced risk compared to males due to their typically smaller body size and reduced lean muscle mass, or it may be that periods of confinement due to oestrous, pregnancy and lactation may simply reduce their exercise levels.
4. Conclusion
Dogs share similar risk factors to humans for both environmental and exertional HRI. Young, active male dogs are most at risk of exertional HRI, whilst older dogs and dogs with underlying health issues such as respiratory compromise are most at risk of environmental HRI during hot weather such as heatwaves. Certain breeds of dogs, and especially those with brachycephaly, are at greater risk of HRI. Studies from the UK and Israel suggest that exertional HRI is the predominant heat-related disorder affecting dogs, with 74% of UK HRI events triggered by exercise. As societies plan mitigation strategies to cope with rising global temperatures it is essential that consideration is given to dogs, not only to protect the health and welfare of millions of pets, but also to ensure working dogs can continue to fulfil their vital roles as assistance, detection and policing dogs.
References
- Macintyre, H.L.; Heaviside, C.; Taylor, J.; Picetti, R.; Symonds, P.; Cai, X.M.; Vardoulakis, S.; Assessing urban population vulnerability and environmental risks across an urban area during heatwaves – Implications for health protection. Science of The Total Environment 2018, 610, 678-690, 10.1016/j.scitotenv.2017.08.062.
- Xu, C.; Kohler, T.A.; Lenton, T.M.; Svenning, J.-C.; Scheffer, M.; Future of the human climate niche. Proceedings of the National Academy of Sciences 2020, 117, 11350-11355, 10.1073/pnas.1910114117.
- Kjellstrom, T.; Briggs, D.; Freyberg, C.; Lemke, B.; Otto, M.; Hyatt, O.; Heat, Human Performance, and Occupational Health: A Key Issue for the Assessment of Global Climate Change Impacts. Annual Review of Public Health 2016, 37, 97-112, 10.1146/annurev-publhealth-032315-021740.
- Hoffman, J.M.; Creevy, K.E.; Franks, A.; O’Neill, D.G.; Promislow, D.E.L.; The companion dog as a model for human aging and mortality. Aging Cell 2018, 17, e12737, 10.1111/acel.12737.
- Bouchama, A.; Knochel, J.P.; Heat Stroke. New England Journal of Medicine 2002, 346, 1978-1988, 10.1056/nejmra011089.
- Yamamoto, T.; Todani, M.; Oda, Y., Kaneko, T.; Kaneda, K.; Fujita, M.; Miyauchi, T.; Tsuruta, R.; Predictive Factors for Hospitalization of Patients with Heat Illness in Yamaguchi, Japan. International Journal of Environmental Research and Public Health 2015, 12(9), 11770–11780, 10.3390/ijerph120911770.
- Yamamoto, T.; Fujita, M.; Oda, Y.; Todani, M.; Hifumi, T.; Kondo, Y.; Shimazaki, J.; Shiraishi, S.; Hayashida, K.; Yokobori, S.; et al. Evaluation of a Novel Classification of Heat-Related Illnesses: A Multicentre Observational Study (Heat Stroke STUDY 2012). International Journal of Environmental Research and Public Health 2018, 15, 1962, 10.3390/ijerph15091962.
- Johnson, S.I.; McMichael, M.; White, G.; Heatstroke in small animal medicine: a clinical practice review. Journal of Veterinary Emergency and Critical Care 2006, 16, 112-119, 10.1111/j.1476-4431.2006.00191.x.
- Rogers, B.; Stiehl, K.; Borst, J.; Hess, A.; Hutchins, S; Heat-related illnesses: the role of the occupational and environmental health nurse. AAOHN Journal 2007, 55, 279-287.
- Duzinski, S.V.; Barczyk, A.N.; Wheeler, T.C.; Iyer, S.S.; Lawson, K.A.; Threat of paediatric hyperthermia in an enclosed vehicle: a year-round study. Injury Prevention 2013, 20, 220-225, 10.1136/injuryprev-2013-040910.
- Armstrong, L.E.; Casa, D.J.; Millard-Stafford, M.; Moran, D.S.; Pyne, S.W.; Roberts, W.O.; Exertional Heat Illness during Training and Competition. Medicine & Science in Sports & Exercise 2007, 39, 556-572, 10.1249/mss.0b013e31802fa199.
- Gauer, R.; Meyers, B.K.; Heat-Related Illnesses. American Family Physician 2019, 99 (8), 482-489.
- Lewis, A.M.; Heatstroke in Older Adults. AJN, American Journal of Nursing 2007, 107, 52-56, 10.1097/01.naj.0000271850.53462.06.
- Gaudio, F.G.; Grissom, C.K.; Cooling Methods in Heat Stroke. The Journal of Emergency Medicine 2016, 50, 607-616, 10.1016/j.jemermed.2015.09.014.
- Bruchim, Y.; Klement, E.; Saragusty, J.; Finkeilstein, E.; Kass, P.; Aroch, I.; Heat stroke in dogs: A retrospective study of 54 cases (1999-2004) and analysis of risk factors for death. Journal of Veterinary Internal Medicine 2006, 20, 38-46.
- Bruchim, Y.; Segev, G.; Kelmer, E.; Codner, C.; Marisat, A.; Horowitz, M; Hospitalized dogs recovery from naturally occurring heatstroke; does serum heat shock protein 72 can provide prognostic biomarker. Cell Stress and Chaperones 2015, 21, 123-130, 10.1007/s12192-015-0645-5.
- Bruchim, Y.; Ginsburg, I.; Segev, G.; Mreisat, A.; Avital, Y.; Aroch, I.; Horowitz, M.; Serum histones as biomarkers of the severity of heatstroke in dogs. Cell Stress and Chaperones 2017, 22, 903-910, 10.1007/s12192-017-0817-6.
- Bruchim, Y.; Kelmer, E.; Cohen, A.; Codner, C.; Segev, G.; Aroch, I.; Hemostatic abnormalities in dogs with naturally occurring heatstroke. Journal of Veterinary Emergency and Critical Care 2017, 346, 1978-324, 10.1111/vec.12590.
- Hall, E.J.; Carter, A.J.; O’Neill, D.G.; Dogs Don’t Die Just in Hot Cars—Exertional Heat-Related Illness (Heatstroke) Is a Greater Threat to UK Dogs. Animals 2020, 10, 1324, 10.3390/ani10081324.
- Teichmann, S.; Turković, V.; Dörfelt, R. ; Heatstroke in dogs in southern Germany. A retrospective study over a 5.5-year period. Tierärztliche Praxis Ausgabe K: Kleintiere / Heimtiere 2014, 42, 213-22.
- Drobatz, K.J.; Macintire, D.K.; Heat-induced illness in dogs: 42 cases (1976-1993). Journal of the American Veterinary Medical Association 1996, 209, 1894-9.
- Bartlett, P. C., Van Buren, J. W., Neterer, M. & Zhou, C.; Disease surveillance and referral bias in the veterinary medical database. Preventive Veterinary Medicine 2010, 94, 264-271, 10.1016/j.prevetmed.2010.01.007.
- Hall, E.J.; Carter, A.J.; O’Neill, D.G.; Incidence and risk factors for heat-related illness (heatstroke) in UK dogs under primary veterinary care in 2016. Scientific Reports 2020, 10, 9128, 10.1038/s41598-020-66015-8.
- Mora, C., Dousset, B., Caldwell, I. R., Powell, F. E., Geronimo, R. C., Bielecki, C. R., Counsell, C. W. W., Dietrich, B. S., Johnston, E. T., Louis, L. V., Lucas, M. P., McKenzie, M. M., Shea, A. G., Tseng, H., Giambelluca, T. W., Leon, L. R., Hawkins, E., & Trauernicht, C.; Global risk of deadly heat. Nature Climate Change 2017, 7, 501-506, 10.1038/nclimate3322.
- Carter, A.J.; Hall, E.J.; Connolly, S.L.; Russell, Z.F.; Mitchell, K.; Drugs, dogs, and driving: The potential for year‐round thermal stress in UK vehicles. Open Veterinary Journal 2020, 10, 216–225, .
- Redmalm, D.; Holy bonsai wolves: Chihuahuas and the Paris Hilton syndrome. International Journal of Cultural Studies 2013, 17, 93-109, 10.1177/1367877912464539.
- Packer, R.M.A.; O’Neill, D.G.; Fletcher, F.; Farnworth, M.J.; Great expectations, inconvenient truths, and the paradoxes of the dog-owner relationship for owners of brachycephalic dogs. PLOS ONE 2019, 14, e0219918, 10.1371/journal.pone.0219918.
- Cotton, D.W.K.; van Hasselt, P.; Bergers, A.M.G.,; Nature of the Sweat Glands in the Hairy Skin of the Beagle. Dermatology 1975, 150, 75-85, 10.1159/000251406.
- Schmidt-Nielsen, K.; Bretz, W.L.; Taylor, C.R.; Panting in Dogs: Unidirectional Air Flow over Evaporative Surfaces. Science 1970, 169, 1102-1104, 10.1126/science.169.3950.1102.
- Ladlow, J.; Liu, N. C.; Kalmar, L.; Sargan, D; Brachycephalic obstructive airway syndrome. Veterinary Record 2018, 182, 375-378, 10.1136/vr.k1403.
- Lilja-Maula, L.; Lappalainen, A.K.; Hyytiäinen, H.K.; Kuusela, E.; Kaimio, M.; Schildt, K.; Mölsä, S.; Morelius, M.; Rajamäki, M.M.; Comparison of submaximal exercise test results and severity of brachycephalic obstructive airway syndrome in English bulldogs. The Veterinary Journal 2017, 219, 22-26, 10.1016/j.tvjl.2016.11.019
- McNicholl, J.; Howarth, G.S.; Hazel, S.J.; Influence of the Environment on Body Temperature of Racing Greyhounds. Frontiers in Veterinary Science 2016, 3, 53, 10.3389/fvets.2016.00053.
- Carter, A.J.; Hall, E.J.; Investigating factors affecting the body temperature of dogs competing in cross country (canicross) races in the UK. Journal of Thermal Biology 2018, 72, 33-38, 10.1016/j.jtherbio.2017.12.006.
- Hemmelgarn, C.; Gannon, K. Heatstroke: thermoregulation, pathophysiology, and predisposing factors. Compend. Contin. Educ. Vet. 2013, 35, E4.
- Durkot, M.J.; Francesconi, R.P.; Hubbard, R.W. Effect of age, weight, and metabolic rate on endurance, hyperthermia, and heatstroke mortality in a small animal model. Aviat. Sp. Environ. Med. 1986, 57, 974–979.
- Young, D. R.; Mosher, R.; Erve, P.; Spector, H. Body; Body temperature and heat exchange during treadmill running in dogs. Journal of Applied Physiology 1959, 14, 839-843, 10.1152/jappl.1959.14.5.839.
- Phillips, C. J.; Coppinger, R. P.; Schimel, D. S.; Hyperthermia in running sled dogs. Journal of Applied Physiology 1981, 51, 135-142, 10.1152/jappl.1981.51.1.135.
- Mattin, M.J.; Boswood, A.; Church, D.B.; López‐Alvarez, J.; McGreevy, P.D.; O’Neill, D.G.; Thomson, P.C.; Brodbelt, D.C. Prevalence of and risk factors for degenerative mitral valve disease in dogs attending primary‐care veterinary practices in england. J. Vet. Intern. Med. 2015, 29, 847–854, doi:10.1111/jvim.12591
- Kuzuya, M. Heatstroke in older adults. Jpn. Med. Assoc. J. 2013, 56, 193–198, doi:10.1097/01.naj.0000271850.53462.06. 15.
- Balmain, B.N.; Sabapathy, S.; Louis, M.; Morris, N.R.; Aging and Thermoregulatory Control: The Clinical Implications of Exercising under Heat Stress in Older Individuals. BioMed Research International 2018, 2018, 1-12, 10.1155/2018/8306154.
This entry is adapted from the peer-reviewed paper 10.3390/ani10081324
References
- Bartlett, P. C., Van Buren, J. W., Neterer, M. & Zhou, C.; Disease surveillance and referral bias in the veterinary medical database. Preventive Veterinary Medicine 2010, 94, 264-271, 10.1016/j.prevetmed.2010.01.007.
- Hall, E.J.; Carter, A.J.; O’Neill, D.G.; Incidence and risk factors for heat-related illness (heatstroke) in UK dogs under primary veterinary care in 2016. Scientific Reports 2020, 10, 9128, 10.1038/s41598-020-66015-8.
- Kjellstrom, T.; Briggs, D.; Freyberg, C.; Lemke, B.; Otto, M.; Hyatt, O.; Heat, Human Performance, and Occupational Health: A Key Issue for the Assessment of Global Climate Change Impacts. Annual Review of Public Health 2016, 37, 97-112, 10.1146/annurev-publhealth-032315-021740.
- Hoffman, J.M.; Creevy, K.E.; Franks, A.; O’Neill, D.G.; Promislow, D.E.L.; The companion dog as a model for human aging and mortality. Aging Cell 2018, 17, e12737, 10.1111/acel.12737.
- Bouchama, A.; Knochel, J.P.; Heat Stroke. New England Journal of Medicine 2002, 346, 1978-1988, 10.1056/nejmra011089.
- Yamamoto, T.; Todani, M.; Oda, Y., Kaneko, T.; Kaneda, K.; Fujita, M.; Miyauchi, T.; Tsuruta, R.; Predictive Factors for Hospitalization of Patients with Heat Illness in Yamaguchi, Japan. International Journal of Environmental Research and Public Health 2015, 12(9), 11770–11780, 10.3390/ijerph120911770.
- Yamamoto, T.; Fujita, M.; Oda, Y.; Todani, M.; Hifumi, T.; Kondo, Y.; Shimazaki, J.; Shiraishi, S.; Hayashida, K.; Yokobori, S.; et al. Evaluation of a Novel Classification of Heat-Related Illnesses: A Multicentre Observational Study (Heat Stroke STUDY 2012). International Journal of Environmental Research and Public Health 2018, 15, 1962, 10.3390/ijerph15091962.
- Johnson, S.I.; McMichael, M.; White, G.; Heatstroke in small animal medicine: a clinical practice review. Journal of Veterinary Emergency and Critical Care 2006, 16, 112-119, 10.1111/j.1476-4431.2006.00191.x.
- Rogers, B.; Stiehl, K.; Borst, J.; Hess, A.; Hutchins, S; Heat-related illnesses: the role of the occupational and environmental health nurse.. AAOHN Journal 2007, 55, 279-287.
- Duzinski, S.V.; Barczyk, A.N.; Wheeler, T.C.; Iyer, S.S.; Lawson, K.A.; Threat of paediatric hyperthermia in an enclosed vehicle: a year-round study. Injury Prevention 2013, 20, 220-225, 10.1136/injuryprev-2013-040910.
- Armstrong, L.E.; Casa, D.J.; Millard-Stafford, M.; Moran, D.S.; Pyne, S.W.; Roberts, W.O.; Exertional Heat Illness during Training and Competition. Medicine & Science in Sports & Exercise 2007, 39, 556-572, 10.1249/mss.0b013e31802fa199.
- Gauer, R.; Meyers, B.K.; Heat-Related Illnesses. American Family Physician 2019, 99 (8), 482-489.
- Lewis, A.M.; Heatstroke in Older Adults. AJN, American Journal of Nursing 2007, 107, 52-56, 10.1097/01.naj.0000271850.53462.06.
- Bruchim, Y.; Klement, E.; Saragusty, J.; Finkeilstein, E.; Kass, P.; Aroch, I.; Heat stroke in dogs: A retrospective study of 54 cases (1999-2004) and analysis of risk factors for death.. Journal of Veterinary Internal Medicine 2006, 20, 38-46.
- Bruchim, Y.; Segev, G.; Kelmer, E.; Codner, C.; Marisat, A.; Horowitz, M; Hospitalized dogs recovery from naturally occurring heatstroke; does serum heat shock protein 72 can provide prognostic biomarker?. Cell Stress and Chaperones 2015, 21, 123-130, 10.1007/s12192-015-0645-5.
- Bruchim, Y.; Ginsburg, I.; Segev, G.; Mreisat, A.; Avital, Y.; Aroch, I.; Horowitz, M.; Serum histones as biomarkers of the severity of heatstroke in dogs. Cell Stress and Chaperones 2017, 22, 903-910, 10.1007/s12192-017-0817-6.
- Bruchim, Y.; Kelmer, E.; Cohen, A.; Codner, C.; Segev, G.; Aroch, I.; Hemostatic abnormalities in dogs with naturally occurring heatstroke. Journal of Veterinary Emergency and Critical Care 2017, 346, 1978-324, 10.1111/vec.12590.
- Hall, E.J.; Carter, A.J.; O’Neill, D.G.; Dogs Don’t Die Just in Hot Cars—Exertional Heat-Related Illness (Heatstroke) Is a Greater Threat to UK Dogs. Animals 2020, 10, 1324, 10.3390/ani10081324.
- Teichmann, S.; Turković, V.; Dörfelt, R. ; Heatstroke in dogs in southern Germany. A retrospective study over a 5.5-year period.. Tierärztliche Praxis Ausgabe K: Kleintiere / Heimtiere 2014, 42, 213-22.
- Drobatz, K.J.; Macintire, D.K.; Heat-induced illness in dogs: 42 cases (1976-1993). Journal of the American Veterinary Medical Association 1996, 209, 1894-9.
- Bartlett, P. C., Van Buren, J. W., Neterer, M. & Zhou, C.; Disease surveillance and referral bias in the veterinary medical database. Preventive Veterinary Medicine 2010, 94, 264-271, 10.1016/j.prevetmed.2010.01.007.
- Hall, E.J.; Carter, A.J.; O’Neill, D.G.; Incidence and risk factors for heat-related illness (heatstroke) in UK dogs under primary veterinary care in 2016. Scientific Reports 2020, 10, 9128, 10.1038/s41598-020-66015-8.
- Gaudio, F.G.; Grissom, C.K.; Cooling Methods in Heat Stroke. The Journal of Emergency Medicine 2016, 50, 607-616, 10.1016/j.jemermed.2015.09.014.