The favorable transition from hominids to homo sapiens during evolution prompted changes in the physiological functions and immune competences (including survival to pathogens and infections) to adapt to the intake of high-energy containing foods, principally dietary fats. Today, the access to a variety of highly-caloric fatty foods is hardly balanced by energy consumption. As a consequence, the dominant genetic pathways evolved to favor the intake of calorie-rich diets and the storage of energy as fats in the adipose tissue are in some circumstances redundant, especially in affluent societies, giving rise to obesity, diabetes and cardiovascular disease (CVD)-comorbidities. Current guidelines recommend reducing the daily intake of dietary fats for the prevention of ischemic cardiovascular diseases (CVDs).
1. Introduction
The favorable transition from
hominids to
homo sapiens during evolution [
1] prompted changes in the physiological functions and immune competences (including survival to pathogens and infections) to adapt to the intake of high-energy containing foods, principally dietary fats [
2]. Today, the access to a variety of highly-caloric fatty foods is hardly balanced by energy consumption. As a consequence, the dominant genetic pathways evolved to favor the intake of calorie-rich diets and the storage of energy as fats in the adipose tissue are in some circumstances redundant, especially in affluent societies, giving rise to obesity, diabetes and cardiovascular disease (CVD)-comorbidities.
Currently, the Western lifestyle, including dietary habits, is believed to contribute a chronic state of low-grade inflammation [
3] that eventually prompts the development of atherosclerosis, the etiopathological factor of ischemic CVDs. Of note is that the connection between the Western dietary lifestyle and onset of CVDs has been demonstrated to impact morbidity and mortality worldwide [
4].
Dietary interventions are considered the first approach in preventing atherosclerotic CVDs. All guidelines, while recommending reduction of fat consumption, also advise avoidance of dietary trans-fats, reducing the intake of saturated fats, and preferring mono or poly-unsaturated long-chain fats [
5]. Achieving these goals remains a challenge for physicians and patients. Furthermore, the level of evidence for these recommendations is backed-up by single randomized clinical trials [
6] and mostly relies upon large non-randomized observational studies [
7], which suffer from confounding [
8] and difficulties in quantitatively measuring dietary intake [
9].
In addition, other factors linked to dietary consumption which are less likely to be captured in epidemiological studies have emerged as being associated with the risk of atherosclerotic CVD, and include the type of food availability, personal knowledge of the impact of diet on health, and socio-economic status [
10]. As an example, the availability of processed foods is associated with an increased risk of CVDs [
11]; this is the case of fat-rich processed meats, whose consumption increases the risk of CVD as compared to fat-rich unprocessed meats [
12], fatty fish, and poultry [
13], whose consumption is not considered a CVD risk modifier.
Furthermore, in modern societies, we are continuously exposed to postprandial lipemia (PPL) [
14], a condition that appears to be causally related to the risk of coronary artery disease [
15], myocardial infarction, ischemic heart disease, and ischemic stroke [
16]. The mechanisms by which an exaggerated PPL links to CVDs include the fostering of endothelial dysfunction [
17,
18,
19], arterial inflammation, and a pro-atherogenic activation of myeloid cells [
18]. In addition, the magnitude of PPL in response to high-fat- based meals in humans appears to be significantly affected by the taxonomic composition of intestinal microbiota [
20], which also cross-talk with hematopoietic niches [
21], ensuring the activity of the innate immune check-points in the intestine and lymphatics. Once absorbed in the intestine, the majority of dietary fats cross over a complex surveillance system (including the cells patrolling at the interface between enterocytes and lacteals like the mesenteric lymph node (MLN), as opposed to the carbohydrates, sugars, dietary amino acids, protein-rich foods and other dietary components that are believed to exert other pathophysiological mechanisms that do not engage these immune checkpoints [
22,
23,
24,
25].
2. Dietary Fats, Inflammation and Atherosclerosis
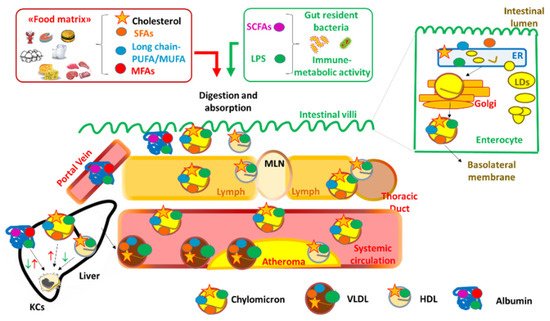
In the human body, dietary fats face a complex metabolic journey involving a number of cellular checkpoints (Figure 1).
Figure 1. The routes for the absorption and the principal immune-inflammatory engagements of dietary lipids in intestinal villi, in the lacteals, MLN up to the liver. MLN = mesenteric lymph node; LDs: lipid droplets; SFAs: saturated fats; MUFA: mono-unsaturated fats; PUFA: poly-unsaturated fats; SCFAs: short chain fatty acids; MFA = medium chain fatty acids; LPS: lipopolysaccharide; ER: endoplasmic reticulum; LDs = lipid droplets; CM: chylomicrons; VLDL = very low density lipoproteins; HDL = high density lipoproteins; DC = dendritic cells; KCs = Kuppfer cells. Upward red arrows indicate activation of a cell or a pathway; downward green arrows indicate inhibition or regulation of a cell or a pathway. Both upward red and downward green arrows for SCFAs and MFAs carried by albumin in the liver indicate contrasting evidence depending on the type of dietary fat.
Dietary fats (triglycerides, phospholipids and cholesterol) are digested in the upper part of the small intestine by the activity of multiple lipases and then absorbed by the enterocytes [
27,
28]. In addition, gut resident bacteria can contribute to circulating fats principally by producing short-chain fatty acids (SCFAs) from fibers/complex carbohydrates. For example,
Faecalibacterium prausnitzii ferments fibers present in the food matrices of fatty foods (e.g., avocados, tree-nuts and peanuts, where over a third of carbohydrates are fibers) [
29] and is the major producer of butyrate. Butyrate is known to regulate hematopoietic activity [
21] and to control myeloid pro-inflammatory skewing [
30], exerting anti-atherogenic properties [
31]. Vice versa,
Ruminococcus bromii, which is reduced in subjects with atherosclerosis [
32], metabolizes complex carbohydrates (that are present in low-fat foods, including pinto beans, whole grains, and nuts with considerable proportion of fats) into propionate. This SCFA promotes insulin sensitivity and reduces the atherosclerotic burden in mice [
33]. Beside the production of SCFAs, other gut microbial species express enzymatic systems that metabolize dietary lipids into inflammatory molecules. Among them, trimethylamine (TMA) lyase, an enzyme that converts dietary phosphatidycholine and choline into TMA, is peculiarly expressed by
Eggerthella lenta and
Eggerthella timonensis [
34,
35]. Finally, gut resident Gram-negative commensals (e.g.,
Escherichia coli, Salmonella minnesota, Salmonella typhimurium) synthetize lipid-containing molecules, such as lipopolysaccharide (LPS), which promote apoptotic signaling and trigger systemic immune-metabolic derangement and inflammation [
36,
37,
38].
Once within the enterocytes, SCFAs directly reach the portal system and the liver where they are readily metabolized, while the majority of absorbed dietary fats are released into the lymphatic tree in large lipoproteins (chylomicrons and very-low density lipoproteins, VLDL) [
39] (
Figure 1). Fatty acids deriving from the hydrolysis of dietary triglycerides and phospholipids in the intestinal lumen are chaperoned to the intracellular endoplasmic reticulum (ER); there, diacylglycerol O-acyltransferase 1 (DGAT1) promotes their re-incorporation in triglycerides which are then transferred by the microsomial triglyceride transfer protein (MTTP) to nascent apolipoprotein B. In this way, chylomicrons are released by the enterocytes in their basolateral membrane. A small fraction of absorbed cholesterol is esterified by acyl CoA-transferase (ACAT) and packaged into chylomicrons. In the Golgi, other apolipoproteins, including apoCIII, apoCII, apoAV, and apoAIV, are added to chylomicrons, which then enter the bloodstream via the thoracic duct and will be eventually taken up by liver (
Figure 1).
In addition to chylomicrons, the intestine also produces a small fraction of high density lipoproteins (HDL), through the activities of ATP binding cassette transporter A-1 (ABCA1) and phospholipid transfer protein (PLTP), which transfer cholesterol and phospholipids to apolipoprotein A-I [
40]. It has been proposed that a fraction of HDL produced by the intestine moves to the liver through the portal system and antagonizes the binding of LPS to toll-like receptor 4 (TLR4) on the membrane of Kuppfer cells, liver-resident macrophages involved in the defense against gut-derived exogenous molecules [
41], thus preventing the recruitment of pro-inflammatory myeloid cells [
42] (
Figure 1). Although further investigations are required, these findings are in line with the known anti-inflammatory function of HDL [
43].
3. Data Linking Intake of Dietary Fats, Markers of Inflammation, and Risk of CVD
The evidence about the molecular and cellular mechanisms by which dietary fats participate in atherogenesis built up the rationale to unveil the connections between different dietary fats, the markers of systemic inflammation, and the risk of CVDs. Despite this aspect having been extensively discussed, data from both epidemiological studies and interventional clinical trials are, however, scarce and heterogeneous.
3.1. Epidemiological Studies
An overall summary of the results from epidemiological studies on the relationship between the pro- or anti-inflammatory effects of dietary fats and CVD risk is reported in Table 1.
Table 1. Summary of the data from epidemiological studies on the association between dietary intake of fats, circulating markers of systemic inflammation and risk of CVD. ↑: Indicates data showing a positive association between the dietary fat intake and the outcome (either inflammatory markers or CVD risk factors); ↓ indicates data showing a positive association between the dietary fat intake and the outcome (either inflammatory markers or CVD risk factors). ↔ indicates that there are missing or contrasting data regarding association between the dietary fat intake and the outcome (either inflammatory markers or CVD risk factors).
|
EPIDEMIOLOGICAL STUDIES
|
|
Dietary fats
|
Prevalent Effects on Inflammatory Markers
|
Effects on CVD Risk/Risk Factors
|
|
Trans fats
|
↑ [116] [117] [118]
↓
↔ [119,120] [121] [122]
|
↑ [116,119,120,121] [117] [118,123]
↓
↔ [122]
|
|
Saturated fats
|
↔ [119,120] [121] [124,125]
|
↑ [119]
↔ [120] [121] [123,124]
|
|
Monounsaturated fats
|
↓ [119] [126,127]
|
↓ [119] [126,127]
↔ [121] [128] [123]
|
|
Polyunsaturated fats
|
↔ [119] [121] [126] [129]
|
↓ [119] [121] [123] [126] [130,131] [129]
|
|
n-3 and derivates
|
↓ [129] [132,133,134,135]
↔ [136]
|
↓ [132,137] [134]
↔ [136]
|
|
n-6 and derivates
|
↔ [119]
|
↓ [119]
|
|
Cholesterol
|
↑ [125]
↔ [138,139,140,141]
|
↑ [138]
↔ [139,140,141,142]
|
3.2. Interventional Clinical Trials
Table 2 reports a summary of the results from clinical trials, testing the impact of dietary fat consumption on markers of inflammation and CVD risk factors.
Table 2. Summary of data from interventional studies about the association between dietary intake of lipids, circulating markers of systemic inflammation and risk of cardiovascular diseases. ↑: Indicates data showing a positive association between the dietary intervention and the outcome (either inflammatory markers or CVD risk factors); ↓ indicates data showing a positive association between the dietary intervention and the outcome (either inflammatory markers or CVD risk factors). ↔ indicates that there are missing or contrasting data regarding association between the dietary intervention and the outcome (either inflammatory markers or CVD risk factors).
|
INTERVENTIONAL TRIALS
|
|
Dietary Lipids
|
Prevalent Effects on Inflammatory Markers
|
Effects on CVD Risk/Risk Factors
|
|
Trans fats
|
↑ [156]
↔ [157]
|
↑ [155] [156]
|
|
Saturated fats
|
↑ [158] [159] [160]
↔ [156] [161,162] [163]
|
↑ [156] [158,161] [159,160,163]
↔ [162]
|
|
Monounsaturated fats
|
↓ [156] [158]
↔ [161,162] [163] [164] [165]
|
↓ [156] [158,161,162] [163] [164]
|
|
Polyunsaturated fats
|
↓ [159]
↔ [161] [163]
|
↓ [161] [159,163] [166]
|
|
Ω-3 and derivates
|
↓ [167,168,169,170,171] [165]
↔ [160] [172] [173,174] [175,176]
|
↓ [160] [168,169,170,171,173]
↔ [167,172] [165,174,175,176]
|
|
Ω-6 and derivates
|
↔ [160] [167]
|
↔ [160] [167]
|
|
Cholesterol
|
↓ [177]
↑ [178]
↔ [179]
|
↓ [180]
↑ [179]
|
This entry is adapted from the peer-reviewed paper 10.3390/nu13113768