“Romantic love is a motivational state typically associated with a desire for long-term mating with a particular individual. It occurs across the lifespan and is associated with distinctive cognitive, emotional, behavioural, social, genetic, neural, and endocrine activity in both sexes. Throughout much of the life course, it serves mate choice, courtship, sex, and pair-bonding functions. It is a suite of adaptations and by-products that arose sometime during the recent evolutionary history of humans”.
Sleep is common in the animal kingdom, although it takes various forms. Sleep in humans is defined “on the basis of both behaviour of the person while asleep and the related physiologic changes that occur to the waking brain’s electrical rhythm in sleep”. Behavioural characteristics of sleep include lack of mobility or slight mobility, closed eyes, a characteristic species-specific sleeping posture, reduced response to external stimulation, quiescence, increased reaction time, elevated arousal threshold, impaired cognitive function, and a reversible unconscious state. It includes non-rapid eye movement (NREM) sleep and rapid eye movement (REM) sleep. Non-rapid eye movement sleep is characterised by synchronised electroencephalographic activity, mildly reduced muscle tone, and slow rolling eye movements. Rapid eye movement sleep is characterised by theta or saw tooth waves and desynchronised electroencephalographic activity, moderately to severely reduced or absent muscle tone, and rapid eye movements. There are three stages of NREM sleep (i.e., N1, N2, N3) and one stage of REM sleep.
- romantic love
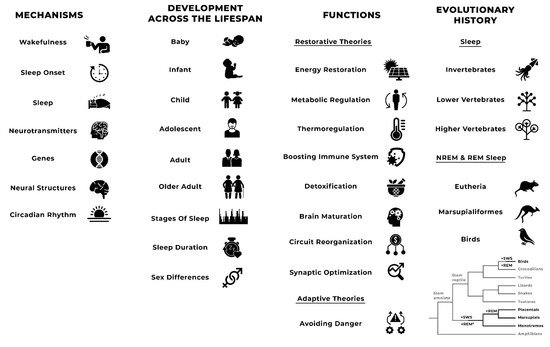
- sleep
- Tinbergen
- mechanisms
- functions
- evolution
1. Romantic Love
2. Sleep
2.1. Definition, Characteristics, and Measurement
2.2. Mechanisms
2.3. Development across the Lifespan
2.4. Functions
2.5. Evolutionary History
3. Romantic Love and Sleep Variations
| Adolescents | Young Adults | Studies | |
|---|---|---|---|
| Sleep onset latency | - | Shorter | [37][38]; see also [35][36][72][73] |
| Sleep duration | Shorter | - | [72][74] *; see also [35][36][37][38][73] |
| WASO | - | Fewer | [37][38]; see also [35][36] |
| Sleep quality | - | Better | [37][38]; see also [72] and [35][36][37][73][74] |
| Restoring sleep | Increased | [37][38] |
Psychopathological Symptoms Associated with Sleep Variations
This entry is adapted from the peer-reviewed paper 10.3390/biology10090923
References
- Bode, A.; Kushnick, G. Proximate and Ultimate Perspectives on Romantic Love. Front. Psychol. 2021, 12, 1088.
- Aron, A.; Dutton, D.G.; Aron, E.N.; Iverson, A. Experiences of falling in love. J. Soc. Pers. Relatsh. 1989, 6, 243–257.
- Pines, A.M. The Role of Gender and Culture in Romantic Attraction. Eur. Psychol. 2001, 6, 96–102.
- Riela, S.; Rodriguez, G.; Aron, A.; Xu, X.M.; Acevedo, B.P. Experiences of falling in love: Investigating culture, ethnicity, gender, and speed. J. Soc. Pers. Relatsh. 2010, 27, 473–493.
- Buss, D.M.; Abbott, M.; Angleitner, A.; Asherian, A.; Biaggio, A.; Blanco-Villasenor, A.; Bruchon-Schweitzer, M.; Ch’u, H.-Y.; Czapinski, J.; Deraad, B.; et al. Internaitonal preferences in selecting mates—A study of 37 cultures. J. Cross-Cult. Psychol. 1990, 21, 5–47.
- Fisher, H.E. Lust, attraction, and attachment in mammalian reproduction. Hum. Nat.-Interdiscip. Biosoc. Perspect. 1998, 9, 23–52.
- Diamond, L.M. Emerging perspectives on distinctions between romantic love and sexual desire. Curr. Dir. Psychol. Sci. 2004, 13, 116–119.
- Emanuele, E.; Brondino, N.; Pesent, S.; Re, S.; Geroldi, D. Genetic loading on human loving styles. Neuroendocrinol. Lett. 2007, 28, 815–821.
- Acevedo, B.P.; Poulin, M.J.; Collins, N.L.; Brown, L.L. After the Honeymoon: Neural and Genetic Correlates of Romantic Love in Newlywed Marriages. Front. Psychol. 2020, 11, 634.
- Xu, X.M.; Weng, X.C.; Aron, A. The mesolimbic dopamine pathway and romantic love. In Brain Mapping: An Encyclopedic Reference; Toga, A.W., Mesulam, M.M., Kastner, S., Eds.; Elsevier: Oxford, UK, 2015.
- Diamond, L.M.; Dickenson, J.A. The neuroimaging of love and desire: Review and future directions. Clin. Neuropsychiatry J. Treat. Eval. 2012, 9, 39–46.
- Cacioppo, S.; Bianchi-Demicheli, F.; Frum, C.; Pfaus, J.G.; Lewis, J.W. The Common Neural Bases Between Sexual Desire and Love: A Multilevel Kernel Density fMRI Analysis. J. Sex. Med. 2012, 9, 1048–1054.
- Cacioppo, S.; Bianchi-Demicheli, F.; Hatfield, E.; Rapson, R.L. Social Neuroscience of Love. Clin. Neuropsychiatry 2012, 9, 3–13.
- Marazziti, D.; Akiskal, H.S.; Rossi, A.; Cassano, G.B. Alteration of the platelet serotonin transporter in romantic love. Psychol. Med. 1999, 29, 741–745.
- Marazziti, D.; Canale, D. Hormonal changes when falling in love. Psychoneuroendocrinology 2004, 29, 931–936.
- Emanuele, E.; Politi, P.; Bianchi, M.; Minoretti, P.; Bertona, M.; Geroldi, D. Raised plasma nerve growth factor levels associated with early-stage romantic love. Psychoneuroendocrinology 2006, 31, 288–294.
- Langeslag, S.J.E.; van der Veen, F.M.; Fekkes, D. Blood Levels of Serotonin Are Differentially Affected by Romantic Love in Men and Women. J. Psychophysiol. 2012, 26, 92–98.
- Weisman, O.; Schneiderman, I.; Zagoory-Sharon, O.; Feldman, R. Early Stage Romantic Love is Associated with Reduced Daily Cortisol Production. Adapt. Hum. Behav. Physiol. 2015, 1, 41–53.
- Marazziti, D.; Baroni, S.; Giannaccini, G.; Piccinni, A.; Mucci, F.; Catena-Dell’Osso, M.; Rutigliano, G.; Massimetti, G.; Dell’Osso, L. Decreased lymphocyte dopamine transporter in romantic lovers. CNS Spectr. 2017, 22, 290–294.
- Sorokowski, P.; Żelaźniewicz, A.; Nowak, J.; Groyecka, A.; Kaleta, M.; Lech, W.; Samorek, S.; Stachowska, K.; Bocian, K.; Pulcer, A.; et al. Romantic Love and Reproductive Hormones in Women. Int. J. Environ. Res. Public Health 2019, 16, 4224.
- Renner, J.; Stanulla, M.; Walther, A.; Schindler, L. CortiLove: A pilot study on hair steroids in the context of being in love and separation. Compr. Psychoneuroendocrinol. 2021, 100061.
- Hatfield, E.; Schmitz, E.; Cornelius, J.; Rapson, R.L. Passionate Love: How Early Does it Begin? J. Psychol. Hum. Sex. 1988, 1, 35–51.
- Wang, A.Y.; Nguyen, H.T. Passionate love and anxiety—A cross-generational study. J. Soc. Psychol. 1995, 135, 459–470.
- Fisher, H.E.; Aron, A.; Brown, L.L. Romantic love: A mammalian brain system for mate choice. Philos. Trans. R. Soc. B-Biol. Sci. 2006, 361, 2173–2186.
- Meston, C.M.; Buss, D.M. Why humans have sex. Arch. Sex Behav. 2007, 36, 477–507.
- Fletcher, G.J.O.; Simpson, J.A.; Campbell, L.; Overall, N.C. Pair-Bonding, Romantic Love, and Evolution: The Curious Case of Homo sapiens. Perspect. Psychol. Sci. 2015, 10, 20–36.
- Siegel, J.M. Do all animals sleep? Trends Neurosci. 2008, 31, 208–213.
- Miyazaki, S.; Liu, C.Y.; Hayashi, Y. Sleep in vertebrate and invertebrate animals, and insights into the function and evolution of sleep. Neurosci. Res. 2017, 118, 3–12.
- Chokroverty, S. Overview of normal sleep. In Sleep Disorders Medicine: Basic Science, Technical Considerations and Clinical Aspects; Chokroverty, S., Sudhansu, S.M., Eds.; Springer: New York, NY, USA, 2017.
- American Academy of Sleep Medicine. The AASM Manual for the Scoring of Sleep and Associated Events—Rules, Terminology and Technical Specifications; American Academy of Sleep Medicine: Darien, IL, USA, 2007.
- Martoni, M.; Biagi, M. Sleep self-report measures: A literature review. Epidemiol. Psychiatr. Sci. 2007, 16, 316–329.
- Caffo, B.; Swihart, B.; Laffan, A.; Crainiceanu, C.; Punjabi, N. An overview of observational sleep research with application to sleep stage transitioning. Chance (N.Y.) 2009, 22, 10–15.
- Van de Water, A.T.; Holmes, A.; Hurley, D.A. Objective measurements of sleep for non-laboratory settings as alternatives to polysomnography—A systematic review. J. Sleep Res. 2011, 20 1Pt 2, 183–200.
- Buysse, D.J.; Reynolds, C.F., III; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213.
- Bajoghli, H.; Joshaghani, N.; Gerber, M.; Mohammadi, M.R.; Holsboer-Trachsler, E.; Brand, S. In Iranian female and male adolescents, romantic love is related to hypomania and low depressive symptoms, but also to higher state anxiety. Int. J. Psychiatry Clin. 2013, 17, 98–109.
- Bajoghli, H.; Joshaghani, N.; Mohammadi, M.R.; Holsboer-Trachsler, E.; Brand, S. In female adolescents, romantic love is related to hypomanic-like stages and increased physical activity, but not to sleep or depressive symptoms. Int. J. Psychiatry Clin. 2011, 15, 164–170.
- Bajoghli, H.; Keshavarzi, Z.; Mohammadi, M.-R.; Schmidt, N.B.; Norton, P.J.; Holsboer-Trachsler, E.; Brand, S. “I love you more than I can stand!”—Romantic love, symptoms of depression and anxiety, and sleep complaints are related among young adults. Int. J. Psychiatry Clin. 2014, 18, 169–174.
- Brand, S.; Foell, S.; Bajoghli, H.; Keshavarzi, Z.; Kalak, N.; Gerber, M.; Schmidt, N.B.; Norton, P.J.; Holsboer-Trachsler, E. “Tell me, how bright your hypomania is, and I tell you, if you are happily in love!”—Among young adults in love, bright side hypomania is related to reduced depression and anxiety, and better sleep quality. Int. J. Psychiatry Clin. 2015, 19, 24–31.
- Berry, R.B.; Brooks, R.; Gamaldo, C.E.; Harding, S.M.; Lloyd, R.; Marcus, C.L.; Vaughn, B.V. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications; American Academy of Sleep Medicine: Darien, IL, USA, 2020.
- Rundo, J.V.; Downey, R., III. Polysomnography. Handb. Clin. Neurol. 2019, 160, 381–392.
- Tinbergen, N. On aims and methods of Ethology. Z. Tierpsychol. 1963, 20, 410–433.
- Lesku, J.A.; Martinez-Gonzalez, D.; Rattenborg, N.C. Phylogeny and ontogeny of sleep. In The Neuroscience of Sleep; Stickgold, R., Walker, M., Eds.; Academic Press: Cambridge, MA, USA, 2009.
- Zielinski, M.R.; McKenna, J.T.; McCarley, R.W. Functions and Mechanisms of Sleep. AIMS Neurosci. 2016, 3, 67–104.
- Eban-Rothschild, A.; Appelbaum, L.; de Lecea, L. Neuronal Mechanisms for Sleep/Wake Regulation and Modulatory Drive. Neuropsychopharmacology 2018, 43, 937–952.
- Murillo-Rodriguez, E.; Arias-Carrion, O.; Zavala-Garcia, A.; Sarro-Ramirez, A.; Huitron-Resendiz, S.; Arankowsky-Sandoval, G. Basic sleep mechanisms: An integrative review. Cent. Nerv. Syst. Agents Med. Chem. 2012, 12, 38–54.
- Bollinger, T.; Schibler, U. Circadian rhythms-from genes to physiology and disease. Swiss Med. Wkly. 2014, 144, w13984.
- Kleitman, N. The nature of sleep. In The Nature of Dreaming; Wolstenholme, G.E.W., O’Connor, M., Eds.; Churchill: London, UK, 1961; pp. 349–364.
- D’Ambrosio, C.; Redline, S. Sleep across the lifespan. In Impact of Sleep and Sleep Disturbances on Obesity and Cancer; Redline, S., Berger, N.A., Eds.; Springer: New York, NY, USA, 2014; pp. 1–23.
- Grigg-Damberger, M.M. Ontogeny of Sleep and Its Functions in Infancy, Childhood, and Adolescence. In Sleep Disorders in Children; Nevšímalová, S., Bruni, O., Eds.; Springer International Publishing: Cham, Switzerland, 2017; pp. 3–29.
- Grandner, M.A.; Martin, J.L.; Patel, N.P.; Jackson, N.J.; Gehrman, P.R.; Pien, G.; Perlis, M.L.; Xie, D.; Sha, D.; Weaver, T.; et al. Age and sleep disturbances among American men and women: Data from the U.S. Behavioral Risk Factor Surveillance System. Sleep 2012, 35, 395–406.
- Li, J.; Gooneratne, N.S. Sleep and health in older adults. In Sleep and Health; Grandner, M.A., Ed.; Academic Press: London, UK, 2019; pp. 21–29.
- Blume, C.; Garbazza, C.; Spitschan, M. Effects of light on human circadian rhythms, sleep and mood. Somnologie 2019, 23, 147–156.
- Tähkämö, L.; Partonen, T.; Pesonen, A.K. Systematic review of light exposure impact on human circadian rhythm. Chronobiol. Int. 2019, 36, 151–170.
- Krishnan, V.; Collop, N.A. Gender differences in sleep disorders. Curr. Opin. Pulm. Med. 2006, 12, 383–389.
- Bao, A.-M.; Swaab, D.F. Sex Differences in the Brain, Behavior, and Neuropsychiatric Disorders. Neuroscientist 2010, 16, 550–565.
- Meers, J.; Stout-Aguilar, J.; Nowakowski, S. Sex differences in sleep health. In Sleep and Health; Grandner, M.A., Ed.; Academic Press: London, UK, 2019; pp. 21–29.
- Freiberg, A.S. Why We Sleep: A Hypothesis for an Ultimate or Evolutionary Origin for Sleep and Other Physiological Rhythms. J. Circadian Rhythm 2020, 18, 2.
- Vibha, M.J.; Sushil, K.J. Sleep: Evolution and Functions; Springer: Singapore, 2020.
- Mogavero, M.P.; DelRosso, L.M.; Fanfulla, F.; Bruni, O.; Ferri, R. Sleep disorders and cancer: State of the art and future perspectives. Sleep Med. Rev. 2021, 56, 101409.
- Research IoMUCoSMa. Extent and Health Consequences of Chronic Sleep Loss and Sleep Disorders. In Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem; Colten, H.R., Altevogt, B.M., Eds.; National Academies Press: Washington, DC, USA, 2006.
- American Academy of Sleep Medicine. International Classification of Sleep Disorders; American Academy of Sleep Medicine: Darien, IL, USA, 2014.
- Besedovsky, L.; Lange, T.; Born, J. Sleep and immune function. Pflugers Arch. 2012, 463, 121–137.
- Irwin, M.R. Sleep and inflammation: Partners in sickness and in health. Nat. Rev. Immunol. 2019, 19, 702–715.
- Vyazovskiy, V.V.; Delogu, A. NREM and REM Sleep: Complementary Roles in Recovery after Wakefulness. Neuroscientist 2014, 20, 203–219.
- McNamara, P. (Ed.) Characteristics of REM and NREM Sleep; Cambridge University Press: Cambridge, UK, 2019; pp. 60–77.
- Siegel, J.M. REM sleep: A biological and psychological paradox. Sleep Med. Rev. 2011, 15, 139–142.
- Laland, K.N.; Brown, G.R. Sense and Nonsense: Evolutionary Perspectives on Human Behaviour, 2nd ed.; Oxford University Press: Oxford, UK, 2011.
- Field, J.M.; Bonsall, M.B. The evolution of sleep is inevitable in a periodic world. PLoS ONE 2018, 13, e0201615.
- Siegel, J.M.; Manger, P.R.; Nienhuis, R.; Fahringer, H.M.; Pettigrew, J.D. The Echidna Tachyglossus aculeatus Combines REM and Non-REM Aspects in a Single Sleep State: Implications for the Evolution of Sleep. J. Neurosci. 1996, 16, 3500.
- Siegel, J.M.; Manger, P.R.; Nienhuis, R.; Fahringer, H.M.; Pettigrew, J.D. Monotremes and the evolution of rapid eye movement sleep. Philos. Trans. R. Soc. Lond. B Biol. Sci. 1998, 353, 1147–1157.
- Yamazaki, R.; Toda, H.; Libourel, P.-A.; Hayashi, Y.; Vogt, K.; Sakurai, T. Evolutionary Origin of Distinct NREM and REM Sleep. Front. Psychol. 2020, 11, 3599.
- Brand, S.; Luethi, M.; von Planta, A.; Hatzinger, M.; Holsboer-Trachsler, E. Romantic love, hypomania, and sleep pattern in adolescents. J. Adolesc. Health 2007, 41, 69–76.
- Bajoghli, H.; Farnia, V.; Joshaghani, N.; Haghighi, M.; Jahangard, L.; Ahmadpanah, M.; Sadeghi Bahmani, D.; Holsboer-Trachsler, E.; Brand, S. “I love you forever (more or less)”-stability and change in adolescents’ romantic love status and associations with mood states. Rev. Bras. Psiquiatr. 2017, 39, 323–329.
- Kuula, L.; Partonen, T.; Pesonen, A.K. Emotions relating to romantic love-further disruptors of adolescent sleep. Sleep Health 2020, 6, 159–165.
- Goodman, W.K.; Price, L.H.; Rasmussen, S.A.; Mazure, C.; Fleischmann, R.L.; Hill, C.L.; Heninger, G.R.; Charney, D.S. The Yale-Brown obsessive compulsive scale: I. Development, use, and reliability. Arch. Gen. Psychiatry 1989, 46, 1006–1011.
- Bastien, C.H.; Vallières, A.; Morin, C.M. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001, 2, 297–307.
- Hatfield, E.; Brinton, C.; Cornelius, J. Passioante love and anxiety in young adolescents. Motiv. Emot. 1989, 13, 271–289.
