Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Pathology
Coronary artery disease is one of the leading causes of morbidity and mortality, and its prevalence increases with age. The growing number of older patients and their differential characteristics make its management a challenge in clinical practice.
- elderly
- acute coronary syndrome
- myocardial infarction
1. Introduction
Coronary artery disease is one of the leading causes of mortality and morbidity worldwide, and its prevalence increases with age [1][2][3]. The lengthening of life expectancy has caused the proportion of older patients admitted for acute coronary syndrome (ACS) to rise significantly, with one in every three patients presenting with ACS being over 75 years old [4].
The older patient has clinical peculiarities that pose a higher risk in this setting, such as comorbidities and geriatric syndromes. Diagnosis and therapeutic approach are also more challenging in this age group due to a higher prevalence of atypical features and an increased vulnerability to side effects and complications [5][6]. Moreover, older patients are often underrepresented in large clinical trials, and there is a paucity of specific evidence.
2. Diagnostic Approach in the Older Patient
The ACS diagnostic pathway is the same as recommended for the general population. However, some peculiarities and challenges should be noted. Atypical symptoms are more frequent, and, together with communication difficulties, may lead to delays or misdiagnoses [7]. Another source of diagnostic uncertainties is the higher frequency of baseline electrocardiogram changes, such as bundle branch block or pacemaker rhythm [7].
Even more challenging may be the interpretation of troponin elevations in the older patient. Elevated basal troponin levels have been described, and it is known that age > 60 years is associated to higher 99th percentile upper reference limit [8][9][10]. Boeddinghaus et al. analyzed the diagnostic performance of the 0/1 h algorithm recommended by the European Society of Cardiology in three age groups (<55 years, young; 55–70 years, middle age; ≥70 years, old) [11]. They found similar rule-out safety (sensitivity) while decreased rule-in accuracy (specificity), 93% for young, 80% for middle-age, and 55% for old (p < 0.001). Using slightly higher cut-off troponin concentrations specific for older patients resulted in increased specificity while maintaining a high sensitivity, especially when using troponin-I [11]. However, the main consensus documents and clinical practice guidelines do not currently support the use of age-specific thresholds [12][13]. Further research is warranted to clarify the best approach.
3. ST-Segment Elevation Myocardial Infarction (STEMI) Patients
Emergent reperfusion, especially primary percutaneous coronary intervention (PCI), is the standard of care in STEMI, and its widespread use has improved both short and long-term prognosis [14][15]. This applies equally to the older patient, but some peculiarities must be noted.
Regarding diagnosis, atypical clinical presentation and communication difficulties (derived from confusional states or cognitive impairment) are more frequent in the elderly and may delay diagnosis [16][17]. Baseline electrocardiogram alterations may also make diagnosis difficult in older patients, since some findings, including history of previous myocardial infarction, pacemaker stimulation, or the presence of left bundle branch block, are common [14][16].
According to current guidelines, primary PCI performed <120 min since the first medical contact is the treatment of choice, irrespective of age. PCI is superior to fibrinolysis in reducing mortality, reinfarction, or stroke [18]. It is recommended to use radial access and stenting with new-generation drug-eluting stents, since this strategy is associated with fewer events [18][19]. Otherwise, and in the absence of contraindications, fibrinolytic therapy is recommended, always within the first 12 h since symptom onset, and providing the highest benefit when administered within the first two hours. Afterwards, the patient must be transferred to a center with a PCI-capable facility (Figure 1) [18]. Thus, if reperfusion is not achieved (ST-segment resolution < 50% within 60–90 min of fibrinolytic administration) or in the presence of persistent chest pain, worsening ischemia, or hemodynamic or electrical instability, rescue PCI is indicated. In other cases, routine early (2–24 h after fibrinolysis) PCI is indicated. Age should not be considered a contraindication to fibrinolysis, since several studies including elderly patients with STEMI receiving this therapy did not find significant differences in the number of major bleedings requiring transfusion compared to PCI or even no reperfusion [20]. On the other hand, the incidence of intracranial bleeding increases with age. Nevertheless, in the STREAM trial, the risk of intracranial hemorrhage was reduced after adjusting the fibrinolytic dose of tenecteplase to 50% in patients older than 75 years of age [21].
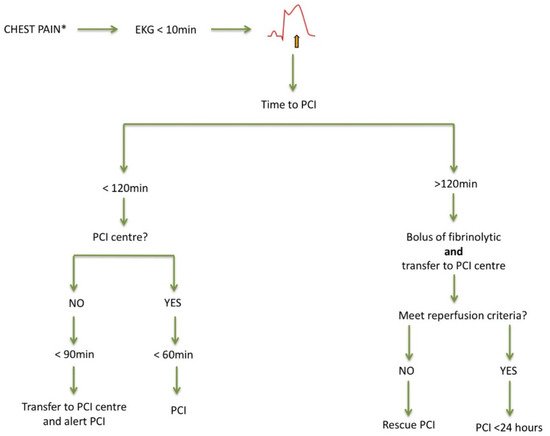
Figure 1. Management of acute ST-segment elevation myocardial infarction. Adapted from [16]. EKG: electrocardiogram; PCI: percutaneous coronary intervention. * Atypical presentation is common.
Despite current evidence and recommendations, older patients are still less likely to receive reperfusion treatment when compared with their younger counterparts [3][16][19][22]. Efforts should be made to improve this picture, as invasive strategies in STEMI associate greater survival in elderly patients, and there is no upper age limit for urgent reperfusion [3][19][22][23].
Regarding prognostic medication in the elderly, current recommendations are not different from those made in younger patients. They improve prognosis [15], though titration may often be slower [14][18]. Moreover, elderly patients should participate in a complete rehabilitation program whenever possible, adapted to age conditions, and addressing comorbidities and geriatric syndromes, which in turn improves both prognosis and quality of life [18]. Unfortunately, these patients are, by far, the least enrolled in these programs [24].
4. Non-STEMI (NSTEMI) Patients: Invasive Versus Conservative Treatment?
Balancing the benefit/risk of harm is crucial in elderly patients with ACS because they have higher risk of mortality but, also, higher risk of bleeding or other side effects of currently recommended treatments. Compared to younger patients, older patients are admitted more frequently with NSTEMI and medical treatments or revascularization are commonly underused [25][26]. Current NSTEMI guidelines clearly state that interventional procedures for revascularization should be applied at any age [13]. Nonetheless, age is frequently reported as the variable most closely related to lower revascularization rates [27]. Of all the reasons postulated for the underuse of revascularization, the leading limitations might be the excess of bleeding complications or the lack of long-term benefit [28]. Bleeding complications have certainly increased in recent decades due to the incorporation of more potent antiplatelet and anticoagulant strategies [29]. In contrast, vascular access complications have decreased substantially with the generalization of radial access, especially in the elderly and high-bleeding risk patients [30][31]. The largest clinical trial involving elderly patients with NSTEMI, or unstable angina, was the After Eighty study that included 457 patients who were randomized to either an invasive or conservative treatment strategy [32]. After 1.5 years of follow-up, the invasive strategy was superior to a conservative strategy in reducing the primary endpoint, namely, a composite of myocardial infarction, urgent revascularization, stroke, or death. The primary endpoint was reduced by 47% using the invasive strategy (hazard ratio 0.53, 95% CI 0.41–0.69; p = 0.0001), although the benefit was lower in patients aged >85, and no differences in terms of bleeding complications were noted. It should be noted that in this trial, a strict conservative strategy was applied instead of a selective invasive strategy, with no coronary angiography performed in any patient assigned to this group. In 2020, the SENIOR-NSTEMI study was published, which was an observational study with 1976 NSTEMI patients aged >80 [33]. After propensity score matching, it showed that revascularization within the first 3 days of admission was associated to 32% reduction in all-cause mortality (hazard ratio: 0.68, 95% CI 0.55–0.84). This study had several limitations because it did not assess the effect of heart failure of index hospitalization on post-discharge prognosis, and heart failure incidence was not assessed taking all-cause mortality as a competing event [34][35].
Lastly, revascularization procedures could also be discussed. The use of drug-eluting stents has been generalized in percutaneous revascularization, and several trials have demonstrated their superiority compared to bare-metal stents also in the elderly [36]. Polymer-free drug-eluting stents have demonstrated to have a very low risk of stent thrombosis with short-term dual antiplatelet treatments [37], and this has also been demonstrated in second and third generations of drug-eluting stents [38]. Another important aspect is the relevance of the complete revascularization in this age group. Agra-Bermejo et al. observed in a propensity-score analysis of an observational cohort a long-term benefit in terms of mortality of complete vs. culprit-only revascularization in older patients with NSTEMI [39]. However, other studies showed controversial results [40][41]. Further randomized evidence is warranted to clarify the better strategy regarding complete revascularization in the older patient.
In conclusion, an invasive strategy with currently available technologies (radial access and newer generation drug-eluting stents) is safe and effective to improve outcomes in elderly patients with NSTEMI and, therefore, it should not be denied in this patient group.
This entry is adapted from the peer-reviewed paper 10.3390/jcm10184132
References
- Benjamin, E.J.; Blaha, M.J.; Chiuve, S.E.; Cushman, M.; Das, S.R.; Deo, R.; de Ferranti, S.D.; Floyd, J.; Fornage, M.; Gillespie, C.; et al. Heart Disease and Stroke Statistics—2017 Update: A Report from the American Heart Association. Circulation 2017, 135, e146–e603.
- Townsend, N.; Nichols, M.; Scarborough, P.; Rayner, M. Cardiovascular disease in Europe-epidemiological update 2015. Eur. Heart J. 2015, 36, 2696–2705.
- Topaz, G.; Finkelstein, A.; Flint, N.; Shacham, Y.; Banai, S.; Steinvil, A.; Arbel, Y.; Keren, G.; Yankelson, L. Comparison of 30-day and long-term outcomes and hospital complications among patients aged <75 versus ≥75 years with ST-elevation myocardial infarction undergoing percutaneous coronary intervention. Am. J. Cardiol. 2017, 119, 1897–1901.
- Ariza-Solé, A.; Alegre, O.; Elola, F.J.; Fernández, C.; Formiga, F.; Martínez-Sellés, M.; Bernal, J.L.; Segura, J.V.; Iñíguez, A.; Bertomeu, V.; et al. Management of myocardial infarction in the elderly. Insights from Spanish Minimum Basic Data Set. Eur. Heart J. Acute Cardiovasc. Care 2019, 8, 242–251.
- Alvarez Alvarez, B.; Cid Alvarez, A.B.; Redondo Dieguez, A.; Sanmartin Pena, X.; Lopez Otero, D.; Avila Carrillo, A.; Gomez Peña, F.; Trillo Nouche, R.; Martinez Selles, M.; Gonzalez-Juanatey, J. Short-term and long-term validation of the fastest score in patients with ST-elevation myocardial infarction after primary angioplasty. Int. J. Cardiol. 2018, 269, 19–22.
- Díez-Villanueva, P.; Ariza-Solé, A.; Bonanad, C.; Martínez-Sellés, M. Síndrome Coronario Agudo en el Paciente Anciano, 1st ed.; International Marketing & Communication, S.A.: Madrid, Spain, 2019.
- Madhavan, M.V.; Gersh, B.J.; Alexander, K.P.; Granger, C.B.; Stone, G.W. Coronary artery disease in patients ≥80 years of age. J. Am. Coll. Cardiol. 2018, 71, 2015–2040.
- Welsh, P.; Preiss, D.; Shah, A.; McAllister, D.; Briggs, A.; Boachie, C.; McConnachie, A.; Hayward, C.; Padmanabhan, S.; Welsh, C.; et al. Comparison between high-sensitivity cardiac troponin T and cardiac troponin I in a large general population cohort. Clin. Chem. 2018, 64, 1607–1616.
- Eggers, K.M.; Lind, L.; Venge, P.; Lindahl, B. Factors influencing the 99th percentile of cardiac troponin I evaluated in community-dwelling individuals at 70 and 75 years of age. Clin. Chem. 2013, 59, 1068–1073.
- Gore, M.O.; Seliger, S.L.; Defilippi, C.R.; Nambi, V.; Christenson, R.H.; Hashim, I.A.; Hoogeveen, R.C.; Ayers, C.R.; Sun, W.; McGuire, D.K.; et al. Age- and sex-dependent upper reference limits for the high-sensitivity cardiac troponin T assay. J. Am. Coll. Cardiol. 2014, 63, 1441–1448.
- Boeddinghaus, J.; Nestelberger, T.; Twerenbold, R.; Neumann, J.T.; Lindahl, B.; Giannitsis, E.; Sörensen, N.A.; Badertscher, P.; Jann, J.E.; Wussler, D.; et al. Impact of age on the performance of the ESC 0/1h-algorithms for early diagnosis of myocardial infarction. Eur. Heart J. 2018, 39, 3780–3794.
- Wu, A.; Christenson, R.H.; Greene, D.N.; Jaffe, A.S.; Kavsak, P.A.; Ordonez-Llanos, J.; Apple, F.S. Clinical laboratory practice recommendations for the use of cardiac troponin in acute coronary syndrome: Expert opinion from the academy of the american association for clinical chemistry and the task force on clinical applications of cardiac bio-markers of the international federation of clinical chemistry and laboratory medicine. Clin. Chem. 2018, 64, 645–655.
- Collet, J.P.; Thiele, H.; Barbato, E.; Barthélémy, O.; Bauersachs, J.; Bhatt, D.L.; Dendale, P.; Dorobantu, M.; Edvardsen, T.; Folliguet, T.; et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur. Heart J. 2021, 42, 1289–1367.
- Puerto, E.; Viana-Tejedor, A.; Martínez-Sellés, M.; Domínguez-Pérez, L.; Moreno, G.; Martín-Asenjo, R.; Bueno, H. Temporal trends in mechanical complications of acute myocardial infarction in the elderly. J. Am. Coll. Cardiol. 2018, 72, 959–966.
- Bastante, T.; Rivero, F.; Cuesta, J.; García, M.; Antuña, P.; Díez-Villanueva, P. Síndrome Coronario Agudo con Elevación del Segmento ST. Díez-Villanueva, P. Manual de Cardiopatía en el Paciente Anciano, 1st ed.; International Marketing & Communication, S.A.: Madrid, Spain, 2018; pp. 89–95.
- Alexander, K.P.; Newby, L.K.; Armstrong, P.W.; Cannon, C.P.; Gibler, W.B.; Rich, M.W.; Van de Werf, F.; White, H.D.; Weaver, W.D.; Naylor, M.D.; et al. Acute coronary care in the elderly, Part II ST-segment–elevation myocardial infarction. A scientific statement for healthcare professionals from the american heart association council on clinical cardiology. Circulation 2007, 115, 2570–2589.
- Rivero, F.; Bastante, T.; Cuesta, J.; Benedicto, A.; Salamanca, J.; Restrepo, J.A.; Aguilar, R.; Gordo, F.; Batlle, M.; Alfonso, F. Factors associated with delays in seeking medical attention in patients with ST-segment elevation acute coronary syndrome. Rev. Esp. Cardiol. 2016, 69, 279–285.
- de la Torre Hernández, J.M.; Brugaletta, S.; Gómez Hospital, J.A.; Baz, J.A.; Pérez de Prado, A.; López Palop, R.; Cid, B.; García Camarero, T.; Diego, A.; Gimeno de Carlos, F.; et al. Primary angioplasty in patients older than 75 years. Profile of patients and procedures, outcomes, and predictors of prognosis in the ESTROFA IM + 75 Registry. Rev. Esp. Cardiol. 2017, 70, 81–87.
- Ibanez, B.; James, S.; Agewall, S.; Antunes, M.J.; Bucciarelli-Ducci, C.; Bueno, H.; Caforio, A.; Crea, F.; Goudevenos, J.A.; Halvorsen, S.; et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur. Heart J. 2018, 39, 119–177.
- Toleva, O.; Ibrahim, Q.; Brass, N.; Sookram, S.; Welsh, R. Treatment choices in elderly patients with ST: Elevation myocardial infarction-insights from the Vital Heart Response registry. Open Heart 2015, 2, e000235.
- Armstrong, P.W.; Gershlick, A.H.; Goldstein, P.; Wilcox, R.; Danays, T.; Lambert, Y.; Sulimov, V.; Rosell Ortiz, F.; Ostojic, M.; Welsh, R.C.; et al. Fibrinolysis or primary PCI in ST-segment elevation myocardial infarction. N. Engl. J. Med. 2013, 368, 1379–1387.
- Puymirat, E.; Aissaoui, N.; Cayla, G.; Lafont, A.; Riant, E.; Mennuni, M.; Saint-Jean, O.; Blanchard, D.; Jourdain, P.; Elbaz, M.; et al. Changes in one-year mortality in elderly patients admitted with acute myocardial infarction in relation with early management. Am. J. Med. 2017, 130, 555–563.
- Fernández-Bergés, D.; Degano, I.R.; Gonzalez Fernandez, R.; Subirana, I.; Vila, J.; Jiménez-Navarro, M.; Perez-Fernandez, S.; Roqué, M.; Bayes-Genis, A.; Fernandez-Aviles, F.; et al. Benefit of primary percutaneous coronary interventions in the elderly with ST segment elevation myocardial infarction. Open Heart 2020, 7, e001169.
- O’Neill, D.; Forman, D.E. Never too old for cardiac rehabilitation. Clin. Geriatr. Med. 2019, 35, 407.
- Bueno, H.; Rossello, X.; Pocock, S.J.; Van de Werf, F.; Chin, C.T.; Danchin, N.; Lee, S.W.; Medina, J.; Huo, Y. In-hospital coronary revascularization rates and post-discharge mortality risk in non–ST-segment elevation acute coronary syndrome. J. Am. Coll. Cardiol. 2019, 74, 1454–1461.
- Gabaldon-Perez, A.; Bonanad, C.; Garcia-Blas, S.; Gavara, J.; Rios-Navarro, C.; Perez-Sole, N.; de Dios, E.; Marcos-Garces, V.; Merenciano-Gonzalez, H.; Monmeneu, J.V.; et al. Stress cardiac magnetic resonance for mortality prediction and decision-making: Registry of 2496 elderly patients with chronic coronary syndrome. Rev. Esp. Cardiol. 2021, 66, 603–605.
- Alvarez-Alvarez, B.; Abou Jokh Casas, C.; Garcia Acuña, J.M.; Cid Alvarez, B.; Agra Bermejo, R.M.; Cordero Fort, A.; Rodríguez Mañero, M.; Gude Sampedro, F.; González-Juanatey, J.R. Temporal trends between association of evidence-based treatment and outcomes in patients with non-ST-elevation myocardial infarction. Int. J. Cardiol. 2018, 260, 1–6.
- Cordero, A.; Escribano, D.; García-Acuña, J.M.; Rodriguez-Mañero, M.; Agra-Bermejo, R.; Bertomeu-González, V.; Cid-Alvarez, B.; Alvarez-Alvarez, B.; Zuazola, P.; González-Juanatey, J.R. Long-term bleeding risk vs. mortality risk in acute coronary syndrome patients according to the 2019 ARC-HBR definition. Thromb. Res. 2020, 196, 516–518.
- Simonsson, M.; Wallentin, L.; Alfredsson, J.; Erlinge, D.; Hellström Ängerud, K.; Hofmann, R.; Kellerth, T.; Lindhagen, L.; Ravn-Fischer, A.; Szummer, K.; et al. Temporal trends in bleeding events in acute myocardial infarction: Insights from the SWEDEHEART registry. Eur. Heart J. 2019, 41, 833–843.
- Gargiulo, G.; Valgimigli, M.; Sunnåker, M.; Vranckx, P.; Frigoli, E.; Leonardi, S.; Spirito, A.; Gragnano, F.; Manavifar, N.; Galea, R.; et al. Choice of access site and type of anticoagulant in acute coronary syndromes with advanced Killip class or out-of-hospital cardiac arrest. Rev. Esp. Cardiol. 2020, 73, 893–901.
- Cesaro, A.; Moscarella, E.; Gragnano, F.; Perrotta, R.; Diana, V.; Pariggiano, I.; Concilio, C.; Alfieri, A.; Cesaro, F.; Mercone, G.; et al. Transradial access versus transfemoral access: A comparison of outcomes and efficacy in reducing hemorrhagic events. Expert Rev. Cardiovasc. Ther. 2019, 17, 435–447.
- Tegn, N.; Abdelnoor, M.; Aaberge, L.; Endresen, K.; Smith, P.; Aakhus, S.; Gjertsen, E.; Dahl-Hofseth, O.; Ranhoff, A.H.; Gullestad, L.; et al. Invasive versus conservative strategy in patients aged 80 years or older with non-ST-elevation myocardial infarction or unstable angina pectoris (After Eighty study): An open-label randomised controlled trial. Lancet 2016, 387, 1057–1065.
- Kaura, A.; Sterne, J.; Trickey, A.; Abbott, S.; Mulla, A.; Glampson, B.; Panoulas, V.; Davies, J.; Woods, K.; Omigie, J.; et al. Invasive versus non-invasive management of older patients with non-ST elevation myocardial infarction (SENIOR-NSTEMI): A cohort study based on routine clinical data. Lancet 2020, 396, 623–634.
- Cordero, A.; Rodríguez-Mañero, M.; Bertomeu-González, V.; Gonzalez-Juanatey, J.R. Managing NSTEMI in older patients. Lancet 2021, 397, 370–371.
- Sanchis, J.; García Acuña, J.M.; Raposeiras, S.; Barrabés, J.A.; Cordero, A.; Martínez-Sellés, M.; Bardají, A.; Díez-Villanueva, P.; Marín, F.; Ruiz-Nodar, J.M.; et al. Comorbidity burden and revascularization benefit in elderly patients with acute coronary syndrome. Rev. Esp. Cardiol. 2020, 74, 765–772.
- de Belder, A.; de la Torre Hernandez, J.M.; Lopez-Palop, R.; O’Kane, P.; Hernandez Hernandez, F.; Strange, J.; Gimeno, F.; Cotton, J.; Diaz Fernandez, J.F.; Carrillo Saez, P.; et al. A prospective randomized trial of everolimus-eluting stents versus bare-metal stents in octogenarians: The XIMA Trial (Xience or Vision Stents for the Management of Angina in the Elderly). J. Am. Coll. Cardiol. 2014, 63, 1371–1375.
- Urban, P.; Meredith, I.T.; Abizaid, A.; Pocock, S.J.; Carrié, D.; Naber, C.; Lipiecki, J.; Richardt, G.; Iñiguez, A.; Brunel, P.; et al. Polymer-free drug-coated coronary stents in patients at high bleeding risk. N. Engl. J. Med. 2015, 373, 2038–2047.
- Windecker, S.; Latib, A.; Kedhi, E.; Kirtane, A.J.; Kandzari, D.E.; Mehran, R.; Price, M.J.; Abizaid, A.; Simon, D.I.; Worthley, S.G.; et al. Polymer-based or polymer-free stents in patients at high bleeding risk. N. Engl. J. Med. 2020, 382, 1208–1218.
- Agra-Bermejo, R.; Cordero, A.; Veloso, P.R.; Álvarez, D.I.; Álvarez, B.Á.; Díaz, B.; Rodríguez, L.A.; Abou-Jokh, C.; Álvarez, B.C.; González-Juanatey, J.R.; et al. Long term prognostic benefit of complete revascularization in elderly presenting with NSTEMI: Real world evidence. Rev. Cardiovasc. Med. 2021, 22, 475–482.
- Rumiz, E.; Berenguer, A.; Vilar, J.V.; Valero, E.; Facila, L.; Cubillos, A.; Sanmiguel, D.; Almela, P.; Morell, S. Long-term outcomes and predictors of morbi-mortality according to age in stemi patients with multivessel disease: Impact of an incomplete revascularization. Catheter. Cardiovasc. Interv. 2018, 92, E512–E517.
- Harada, M.; Miura, T.; Kobayashi, T.; Kobayashi, H.; Kobayashi, M.; Nakajima, H.; Kimura, H.; Akanuma, H.; Mawatari, E.; Sato, T.; et al. Clinical impact of complete revascularization in elderly patients with multi-vessel coronary artery disease undergoing percutaneous coronary intervention: A sub-analysis of the SHINANO registry. Int. J. Cardiol. 2017, 230, 413–419.
This entry is offline, you can click here to edit this entry!
