Chronic obstructive pulmonary disease is one of the leading causes of morbidity and mortality worldwide and a growing healthcare problem. Several dietary options can be considered in terms of COPD prevention and/or progression. Although definitive data are lacking, the available scientific evidence indicates that some foods and nutrients, especially those nutraceuticals endowed with antioxidant and anti-inflammatory properties and when consumed in combinations in the form of balanced dietary patterns, are associated with better pulmonary function, less lung function decline, and reduced risk of COPD.
- antioxidant
- chronic obstructive pulmonary disease
- dietary pattern
- inflammation
- lung function
- Mediterranean diet
- nutrition
- oxidative stress
- polyphenol
- polyunsaturated fatty acid
1. Introduction
2. Pathophysiological Aspects in COPD
3. Epidemiological Studies on Diet and Pulmonary Function: Some Methodological Issues
4. Oxidant–Antioxidant Imbalance and Diet Quality in COPD
5. Individual Foods and Nutrients, Lung Function, and COPD
5.1. Role of Antioxidant and Anti-Inflammatory Foods: Fruits and Vegetables
5.2. Vitamin and Nonvitamin Antioxidants
5.3. Minerals
5.4. Wholegrains and Fibers
5.5. Alcohol and Wine
5.6. Vitamin D
5.7. Coffee and Its Components
5.8. Role of Fish and n-3 Polyunsaturated Fatty Acids
5.9. Foods with Potential Deleterious Effects on Lung Function and COPD
6. Dietary Patterns, Lung Function, and COPD
|
Dietary Patterns |
Country (Cohort) |
Design (Follow-Up) |
Population |
Sex (Age) |
Diet Assessment Method |
Outcome |
Outcome Assessment |
Main Results |
Ref |
|---|---|---|---|---|---|---|---|---|---|
|
Data-driven dietary patterns |
|||||||||
|
Meat–dim sum pattern and vegetable–fruit–soy pattern |
China (SCHS) |
P (5.3 year) |
General population n = 52,325 |
F, M (45–74 year) |
FFQ and PCA |
New onset of cough with phlegm |
Self-reported |
The meat-dim sum pattern was associated with increased incidence of cough with phlegm (fourth vs. first quartile, OR = 1.43, 95% CI: 1.08, 1.89, p for trend = 0.02)) |
[114] |
|
Prudent pattern and Western pattern |
USA (HPFS) |
P (12 year) |
Health professionals n = 42,917 |
M (40–75 year) |
FFQ and PCA |
COPD incidence |
Self-reported |
The prudent pattern was negatively (highest vs. lowest quintile, RR = 0.50, 95% CI: 0.25, 0.98), while the Western pattern was positively (highest vs. lowest quintile, RR = 4.56, 95% CI: 1.95, 10.69) associated with COPD risk |
[115] |
|
Prudent pattern and Western pattern |
USA (NHS) |
P (6 year) |
Nurses n = 72,043 |
F (30–55 year) |
FFQ and PCA |
COPD incidence |
Self-reported |
The prudent pattern was negatively (highest vs. lowest quintile, RR = 0.75, 95% CI: 0.58, 0.98), while the Western pattern was positively (highest vs. lowest quintile, RR = 1.31, 95% CI: 0.94, 1.82) associated with COPD risk |
[116] |
|
Prudent pattern and traditional pattern |
United Kingdom (HCS) |
C |
General population n = 1391 (F), n = 1551 (M) |
F, M (mean 66 year) |
FFQ and PCA |
Primary outcome: FEV1; Secondary outcomes: FVC, FEV1/FVC, COPD prevalence |
Spirometry |
The prudent pattern was positively associated with FEV1 in M and F (changes in FEV1 between highest vs. lowest quintiles, 180 mL in M, 95% CI: 0.00, 0.16, p for trend<0.001, and 80 mL in F, 95% CI: 0.26, 0.81, p for trend = 0.008), and negatively with COPD in M (top versus bottom quintile, OR = 0.46, 95% CI: 0.26, 0.81, p = 0.012) |
[117] |
|
Prudent pattern, high-CHO diet, Western pattern |
Swiss (SAPALDIA) |
C |
General population n = 2178 |
F, M (mean 58.6 year) |
FFQ and PCA |
FEV1, FEV1/FVC, FEF25-75, COPD prevalence |
Spirometry |
The prudent pattern was positively associated with lung function and negatively with COPD prevalence (NS) |
[118] |
|
Western pattern and prudent pattern |
USA (ARIC) |
C |
General population n = 15,256 |
F, M (mean 54.2 year) |
FFQ and PCA |
Respiratory symptoms (cough, phlegm, wheeze), FEV1, FEV1/FVC, COPD prevalence |
Spirometry |
The Western pattern was associated with higher prevalence of COPD (fifth vs. first quintile: OR = 1.62, 95% CI: 1.33, 1.97, p < 0.001), respiratory symptoms (wheeze OR = 1.37, 95% CI: 1.11, 1.69, p = 0.002; cough OR = 1.32, 95% CI: 1.10, 1.59, p = 0.001, phlegm OR = 1.27, 95% CI: 1.05, 1.54, p = 0.031), and worse lung function (e.g., percent predicted FEV1: fifth quintile 91.8 vs. first quintile 95.1, p < 0.001). The prudent pattern was associated with lower prevalence of COPD (OR = 0.82, 95% CI: 0.70, 0.95, p = 0.007), cough (OR = 0.77, 95% CI: 0.67, 0.89, p < 0.001), and higher lung function (e.g., percent predicted FEV1: fifth quintile 94.3 vs. first quintile 92.7, p < 0.001) |
[119] |
|
Cosmopolitan pattern, traditional pattern, and refined food dietary pattern |
Netherlands (MORGEN-EPIC) |
C |
General population n = 12,648 |
F, M (mean 41 year) |
FFQ and PCA |
FEV1, wheeze, asthma, COPD prevalence |
Spirometry and self-reported symptoms |
The traditional pattern was associated with lower FEV1 (fifth vs. first quintile, −94.4 mL, 95% CI:−123.4, −65.5, p < 0.001) and increased prevalence of COPD (fifth vs. first quintile, OR = 1.60, 95% CI: 1.1, 2.3, p for trend = 0.001); the cosmopolitan pattern was associated with increased prevalence of asthma (fifth vs. first quintile, OR = 1.4; 95% CI: 1.0, 2.0; p for trend = 0.047) and wheeze (fifth vs. first quintile, OR = 1.3, 95% CI: 1.0, 1.5; p for trend = 0.001) |
[120] |
|
P (5 y) |
General population n = 2911 |
F, M (mean 45 year) |
FFQ and PCA |
FEV1 |
Spirometry |
The refined food pattern was associated with a nonsignificant greater decline in lung function (−48.5 mL, 95% CI: –80.7, −16.3; p for trend = 0.11) |
[120] |
||
|
Alcohol-consumption pattern, Westernized pattern, and MED-like pattern |
Spain |
C |
Smokers with no respiratory diseases n = 207 |
F, M (35–70 year) |
FFQ and PCA |
Impaired lung function |
Spirometry |
Alcohol-consumption pattern (OR = 4.56, 95% CI: 1.58, 13.18, p = 0.005) and Westernized pattern (in F) (OR = 5.62, 95% CI: 1.17, 27.02, p = 0.031) were associated with impaired lung function; a nonsignificant trend for preserved lung function was found for MED-like pattern (OR = 0.71, 95% CI: 0.28, 1.79, p > 0.05) |
[121] |
|
Diet quality scores |
|||||||||
|
Alternate Health Eating Index (AHEI) |
USA (NHS and HPFS) |
P (16 y NHS; 12 y HPFS) |
Nurses n = 73,228 (NHS) Health professionals n = 47,026 (HPFS) |
F (30–55 year), M (40–75) |
FFQ and diet quality index (AHEI-2010) |
COPD incidence |
Self-reported |
A higher AHEI-2010 diet score was associated with lower COPD risk (for the fourth fifth of the score, HR = 0.67, 95% CI: 0.53, 0.85, p for trend <0.001) |
[122] |
|
Health Eating Index (HEI) and MED diet score |
Iran |
C |
Stable COPD n = 121 |
F, M (mean 66.1 year) |
FFQ and diet quality index (HEI, and MED score) |
COPD severity |
Spirometry |
Higher MED score was associated with lower FEV1 and FCV. MED score and AHEI decreased as COPD severity increased (NS) |
[123] |
|
MED diet score |
Spain (ILERVAS) |
C |
General population n = 3020 |
F (50–70 year), M (45–65 year) |
FFQ and MED score |
FEV1, FVC, FEV1/FVC |
Spirometry |
A lower MED diet score was associated with impaired lung function in F (low vs. high adherence, OR = 2.07, 95% CI: 1.06, 4.06, p = 0.033) and the presence of obstructive ventilator defects in M (low vs. high adherence, OR = 4.14, 95% CI: 1.42, 12.1, p = 0.009) |
[124] |
This entry is adapted from the peer-reviewed paper 10.3390/nu11061357
References
- Adeloye, D.; Chua, S.; Lee, C.; Basquill, C.; Papana, A.; Theodoratou, E.; Nair, H.; Gasevic, D.; Sridhar, D.; Campbell, H.; et al. Global and regional estimates of COPD prevalence: Systematic review and meta-analysis. J. Glob. Health 2015, 5, 020415.
- Barnes, P.J.; Shapiro, S.D.; Pauwels, R.A. Chronic obstructive pulmonary disease: Molecular and cellular mechanisms. Eur. Respir. J. 2003, 22, 672–688.
- Vestbo, J.; Hurd, S.S.; Agusti, A.G.; Jones, P.W.; Vogelmeier, C.; Anzueto, A.; Barnes, P.J.; Fabbri, L.M.; Martinez, F.J.; Nishimura, M.; et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am. J. Respir. Crit. Care Med. 2013, 187, 347–365.
- Vestbo, J.; Edwards, L.D.; Scanlon, P.D.; Yates, J.C.; Agusti, A.; Bakke, P.; Calverley, P.M.; Celli, B.; Coxson, H.O.; Crim, C.; et al. Changes in forced expiratory volume in 1 second over time in COPD. N. Engl. J. Med. 2011, 365, 1184–1192.
- Agusti, A.; Edwards, L.D.; Rennard, S.I.; MacNee, W.; Tal-Singer, R.; Miller, B.E.; Vestbo, J.; Lomas, D.A.; Calverley, P.M.; Wouters, E.; et al. Persistent systemic inflammation is associated with poor clinical outcomes in COPD: A novel phenotype. PLoS ONE 2012, 7, e37483.
- Burgel, P.R.; Paillasseur, J.L.; Peene, B.; Dusser, D.; Roche, N.; Coolen, J.; Troosters, T.; Decramer, M.; Janssens, W. Two distinct chronic obstructive pulmonary disease (COPD) phenotypes are associated with high risk of mortality. PLoS ONE 2012, 7, e51048.
- Burgel, P.R.; Paillasseur, J.L.; Roche, N. Identification of clinical phenotypes using cluster analyses in COPD patients with multiple comorbidities. BioMed Res. Int. 2014, 2014.
- Burgel, P.R.; Roche, N.; Paillasseur, J.L.; Tillie-Leblond, I.; Chanez, P.; Escamilla, R.; Court-Fortune, I.; Perez, T.; Carre, P.; Caillaud, D.; et al. Clinical COPD phenotypes identified by cluster analysis: Validation with mortality. Eur. Respir. J. 2012, 40, 495–496.
- Miravitlles, M.; Calle, M.; Soler-Cataluna, J.J. Clinical phenotypes of COPD: Identification, definition and implications for guidelines. Arch. Bronconeumol. 2012, 48, 86–98.
- Postma, D.S.; Bush, A.; van den Berge, M. Risk factors and early origins of chronic obstructive pulmonary disease. Lancet 2015, 385, 899–909.
- Rabe, K.F.; Watz, H. Chronic obstructive pulmonary disease. Lancet 2017, 389, 1931–1940.
- Schulze, M.B.; Martinez-Gonzalez, M.A.; Fung, T.T.; Lichtenstein, A.H.; Forouhi, N.G. Food based dietary patterns and chronic disease prevention. BMJ 2018, 361, k2396.
- Berthon, B.S.; Wood, L.G. Nutrition and respiratory health—Feature review. Nutrients 2015, 7, 1618–1643.
- Zheng, P.F.; Shu, L.; Si, C.J.; Zhang, X.Y.; Yu, X.L.; Gao, W. Dietary Patterns and Chronic Obstructive Pulmonary Disease: A Meta-analysis. COPD 2016, 13, 515–522.
- Vasankari, T.; Harkanen, T.; Kainu, A.; Saaksjarvi, K.; Mattila, T.; Jousilahti, P.; Laitinen, T. Predictors of New Airway Obstruction—An 11 Year’s Population-Based Follow-Up Study. COPD 2019, 16, 45–50.
- Whyand, T.; Hurst, J.R.; Beckles, M.; Caplin, M.E. Pollution and respiratory disease: Can diet or supplements help? A review. Respir. Res. 2018, 19, 79.
- Smit, H.A. Chronic obstructive pulmonary disease, asthma and protective effects of food intake: From hypothesis to evidence? Respir. Res. 2001, 2, 261–264.
- Zhai, T.; Li, S.; Hu, W.; Li, D.; Leng, S. Potential Micronutrients and Phytochemicals against the Pathogenesis of Chronic Obstructive Pulmonary Disease and Lung Cancer. Nutrients 2018, 10.
- Carraro, S.; Scheltema, N.; Bont, L.; Baraldi, E. Early-life origins of chronic respiratory diseases: Understanding and promoting healthy ageing. Eur. Respir. J. 2014, 44, 1682–1696.
- Schols, A.M.; Ferreira, I.M.; Franssen, F.M.; Gosker, H.R.; Janssens, W.; Muscaritoli, M.; Pison, C.; Rutten-van Molken, M.; Slinde, F.; Steiner, M.C.; et al. Nutritional assessment and therapy in COPD: A European Respiratory Society statement. Eur. Respir. J. 2014, 44, 1504–1520.
- van den Borst, B.; Gosker, H.R.; Wesseling, G.; de Jager, W.; Hellwig, V.A.; Snepvangers, F.J.; Schols, A.M. Low-grade adipose tissue inflammation in patients with mild-to-moderate chronic obstructive pulmonary disease. Am. J. Clin. Nutr. 2011, 94, 1504–1512.
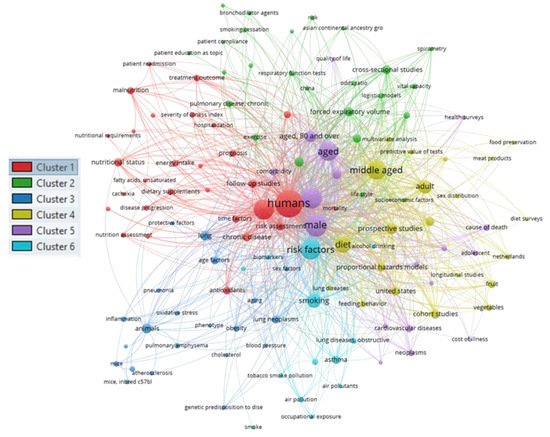
- van Eck, N.J.; Waltman, L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics 2010, 84, 523–538.
- Yao, H.; Rahman, I. Current concepts on oxidative/carbonyl stress, inflammation and epigenetics in pathogenesis of chronic obstructive pulmonary disease. Toxicol. Appl. Pharmacol. 2011, 254, 72–85.
- Di Stefano, A.; Caramori, G.; Oates, T.; Capelli, A.; Lusuardi, M.; Gnemmi, I.; Ioli, F.; Chung, K.F.; Donner, C.F.; Barnes, P.J.; et al. Increased expression of nuclear factor-kappaB in bronchial biopsies from smokers and patients with COPD. Eur. Respir. J. 2002, 20, 556–563.
- Brassington, K.; Selemidis, S.; Bozinovski, S.; Vlahos, R. New frontiers in the treatment of comorbid cardiovascular disease in chronic obstructive pulmonary disease. Clin. Sci. (Lond.) 2019, 133, 885–904.
- Sin, D.D.; Wu, L.; Man, S.F. The relationship between reduced lung function and cardiovascular mortality: A population-based study and a systematic review of the literature. Chest 2005, 127, 1952–1959.
- Gut-Gobert, C.; Cavailles, A.; Dixmier, A.; Guillot, S.; Jouneau, S.; Leroyer, C.; Marchand-Adam, S.; Marquette, D.; Meurice, J.C.; Desvigne, N.; et al. Women and COPD: Do we need more evidence? Eur. Respir. Rev. 2019, 28.
- Han, M.K.; Postma, D.; Mannino, D.M.; Giardino, N.D.; Buist, S.; Curtis, J.L.; Martinez, F.J. Gender and chronic obstructive pulmonary disease: Why it matters. Am. J. Respir. Crit. Care Med. 2007, 176, 1179–1184.
- O’Doherty Jensen, K.; Holm, L. Preferences, quantities and concerns: Socio-cultural perspectives on the gendered consumption of foods. Eur. J. Clin. Nutr. 1999, 53, 351–359.
- Osler, M.; Tjonneland, A.; Suntum, M.; Thomsen, B.L.; Stripp, C.; Gronbaek, M.; Overvad, K. Does the association between smoking status and selected healthy foods depend on gender? A population-based study of 54 417 middle-aged Danes. Eur. J. Clin. Nutr. 2002, 56, 57–63.
- Tavilani, H.; Nadi, E.; Karimi, J.; Goodarzi, M.T. Oxidative stress in COPD patients, smokers, and non-smokers. Respir. Care 2012, 57, 2090–2094.
- Ochs-Balcom, H.M.; Grant, B.J.; Muti, P.; Sempos, C.T.; Freudenheim, J.L.; Browne, R.W.; McCann, S.E.; Trevisan, M.; Cassano, P.A.; Iacoviello, L.; et al. Antioxidants, oxidative stress, and pulmonary function in individuals diagnosed with asthma or COPD. Eur. J. Clin. Nutr. 2006, 60, 991–999.
- Rodriguez-Rodriguez, E.; Ortega, R.M.; Andres, P.; Aparicio, A.; Gonzalez-Rodriguez, L.G.; Lopez-Sobaler, A.M.; Navia, B.; Perea, J.M.; Rodriguez-Rodriguez, P. Antioxidant status in a group of institutionalised elderly people with chronic obstructive pulmonary disease. Br. J. Nutr. 2016, 115, 1740–1747.
- Louhelainen, N.; Rytila, P.; Haahtela, T.; Kinnula, V.L.; Djukanovic, R. Persistence of oxidant and protease burden in the airways after smoking cessation. BMC Pulm. Med. 2009, 9, 25.
- Sargeant, L.A.; Jaeckel, A.; Wareham, N.J. Interaction of vitamin C with the relation between smoking and obstructive airways disease in EPIC Norfolk. European Prospective Investigation into Cancer and Nutrition. Eur. Respir. J. 2000, 16, 397–403.
- Bartoli, M.L.; Novelli, F.; Costa, F.; Malagrino, L.; Melosini, L.; Bacci, E.; Cianchetti, S.; Dente, F.L.; Di Franco, A.; Vagaggini, B.; et al. Malondialdehyde in exhaled breath condensate as a marker of oxidative stress in different pulmonary diseases. Mediat. Inflamm. 2011, 2011, 891752.
- Arja, C.; Surapaneni, K.M.; Raya, P.; Adimoolam, C.; Balisetty, B.; Kanala, K.R. Oxidative stress and antioxidant enzyme activity in South Indian male smokers with chronic obstructive pulmonary disease. Respirology 2013, 18, 1069–1075.
- Ahmad, A.; Shameem, M.; Husain, Q. Altered oxidant-antioxidant levels in the disease prognosis of chronic obstructive pulmonary disease. Int. J. Tuberc. Lung Dis. 2013, 17, 1104–1109.
- Guenegou, A.; Leynaert, B.; Pin, I.; Le Moel, G.; Zureik, M.; Neukirch, F. Serum carotenoids, vitamins A and E, and 8 year lung function decline in a general population. Thorax 2006, 61, 320–326.
- McKeever, T.M.; Lewis, S.A.; Smit, H.A.; Burney, P.; Cassano, P.A.; Britton, J. A multivariate analysis of serum nutrient levels and lung function. Respir. Res. 2008, 9, 67.
- Lin, Y.C.; Wu, T.C.; Chen, P.Y.; Hsieh, L.Y.; Yeh, S.L. Comparison of plasma and intake levels of antioxidant nutrients in patients with chronic obstructive pulmonary disease and healthy people in Taiwan: A case-control study. Asia Pac. J. Clin. Nutr. 2010, 19, 393–401.
- Laudisio, A.; Costanzo, L.; Di Gioia, C.; Delussu, A.S.; Traballesi, M.; Gemma, A.; Antonelli Incalzi, R. Dietary intake of elderly outpatients with chronic obstructive pulmonary disease. Arch. Gerontol. Geriatr. 2016, 64, 75–81.
- van de Bool, C.; Mattijssen-Verdonschot, C.; van Melick, P.P.; Spruit, M.A.; Franssen, F.M.; Wouters, E.F.; Schols, A.M.; Rutten, E.P. Quality of dietary intake in relation to body composition in patients with chronic obstructive pulmonary disease eligible for pulmonary rehabilitation. Eur. J. Clin. Nutr. 2014, 68, 159–165.
- Gronberg, A.M.; Slinde, F.; Engstrom, C.P.; Hulthen, L.; Larsson, S. Dietary problems in patients with severe chronic obstructive pulmonary disease. J. Hum. Nutr. Diet. 2005, 18, 445–452.
- Tabak, C.; Smit, H.A.; Rasanen, L.; Fidanza, F.; Menotti, A.; Nissinen, A.; Feskens, E.J.; Heederik, D.; Kromhout, D. Dietary factors and pulmonary function: A cross sectional study in middle aged men from three European countries. Thorax 1999, 54, 1021–1026.
- Butland, B.K.; Fehily, A.M.; Elwood, P.C. Diet, lung function, and lung function decline in a cohort of 2512 middle aged men. Thorax 2000, 55, 102–108.
- Tabak, C.; Arts, I.C.; Smit, H.A.; Heederik, D.; Kromhout, D. Chronic obstructive pulmonary disease and intake of catechins, flavonols, and flavones: The MORGEN Study. Am. J. Respir. Crit. Care Med. 2001, 164, 61–64.
- Tabak, C.; Smit, H.A.; Heederik, D.; Ocke, M.C.; Kromhout, D. Diet and chronic obstructive pulmonary disease: Independent beneficial effects of fruits, whole grains, and alcohol (the MORGEN study). Clin. Exp. Allergy 2001, 31, 747–755.
- Miedema, I.; Feskens, E.J.; Heederik, D.; Kromhout, D. Dietary determinants of long-term incidence of chronic nonspecific lung diseases. The Zutphen Study. Am. J. Epidemiol. 1993, 138, 37–45.
- Walda, I.C.; Tabak, C.; Smit, H.A.; Rasanen, L.; Fidanza, F.; Menotti, A.; Nissinen, A.; Feskens, E.J.; Kromhout, D. Diet and 20-year chronic obstructive pulmonary disease mortality in middle-aged men from three European countries. Eur. J. Clin. Nutr. 2002, 56, 638–643.
- Kaluza, J.; Larsson, S.C.; Orsini, N.; Linden, A.; Wolk, A. Fruit and vegetable consumption and risk of COPD: A prospective cohort study of men. Thorax 2017, 72, 500–509.
- Kaluza, J.; Harris, H.R.; Linden, A.; Wolk, A. Long-term consumption of fruits and vegetables and risk of chronic obstructive pulmonary disease: A prospective cohort study of women. Int. J. Epidemiol. 2018, 47, 1897–1909.
- Carey, I.M.; Strachan, D.P.; Cook, D.G. Effects of changes in fresh fruit consumption on ventilatory function in healthy British adults. Am. J. Respir. Crit. Care Med. 1998, 158, 728–733.
- Holt, E.M.; Steffen, L.M.; Moran, A.; Basu, S.; Steinberger, J.; Ross, J.A.; Hong, C.P.; Sinaiko, A.R. Fruit and vegetable consumption and its relation to markers of inflammation and oxidative stress in adolescents. J. Am. Diet. Assoc. 2009, 109, 414–421.
- Rink, S.M.; Mendola, P.; Mumford, S.L.; Poudrier, J.K.; Browne, R.W.; Wactawski-Wende, J.; Perkins, N.J.; Schisterman, E.F. Self-report of fruit and vegetable intake that meets the 5 a day recommendation is associated with reduced levels of oxidative stress biomarkers and increased levels of antioxidant defense in premenopausal women. J. Acad. Nutr. Diet. 2013, 113, 776–785.
- McKeever, T.M.; Scrivener, S.; Broadfield, E.; Jones, Z.; Britton, J.; Lewis, S.A. Prospective study of diet and decline in lung function in a general population. Am. J. Respir. Crit. Care Med. 2002, 165, 1299–1303.
- Tug, T.; Karatas, F.; Terzi, S.M. Antioxidant vitamins (A, C and E) and malondialdehyde levels in acute exacerbation and stable periods of patients with chronic obstructive pulmonary disease. Clin. Investig. Med. 2004, 27, 123–128.
- Agler, A.H.; Kurth, T.; Gaziano, J.M.; Buring, J.E.; Cassano, P.A. Randomised vitamin E supplementation and risk of chronic lung disease in the Women’s Health Study. Thorax 2011, 66, 320–325.
- Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of antioxidant vitamin supplementation in 20,536 high-risk individuals: A randomised placebo-controlled trial. Lancet 2002, 360, 7–22.
- Andersson, I.; Gronberg, A.; Slinde, F.; Bosaeus, I.; Larsson, S. Vitamin and mineral status in elderly patients with chronic obstructive pulmonary disease. Clin. Respir. J. 2007, 1, 23–29.
- Hirayama, F.; Lee, A.H.; Oura, A.; Mori, M.; Hiramatsu, N.; Taniguchi, H. Dietary intake of six minerals in relation to the risk of chronic obstructive pulmonary disease. Asia Pac. J. Clin. Nutr. 2010, 19, 572–577.
- Pearson, P.; Britton, J.; McKeever, T.; Lewis, S.A.; Weiss, S.; Pavord, I.; Fogarty, A. Lung function and blood levels of copper, selenium, vitamin C and vitamin E in the general population. Eur. J. Clin. Nutr. 2005, 59, 1043–1048.
- Cassano, P.A.; Guertin, K.A.; Kristal, A.R.; Ritchie, K.E.; Bertoia, M.L.; Arnold, K.B.; Crowley, J.J.; Hartline, J.; Goodman, P.J.; Tangen, C.M.; et al. A randomized controlled trial of vitamin E and selenium on rate of decline in lung function. Respir. Res. 2015, 16, 35.
- Root, M.M.; Houser, S.M.; Anderson, J.J.; Dawson, H.R. Healthy Eating Index 2005 and selected macronutrients are correlated with improved lung function in humans. Nutr. Res. 2014, 34, 277–284.
- Jacobs, D.R., Jr.; Andersen, L.F.; Blomhoff, R. Whole-grain consumption is associated with a reduced risk of noncardiovascular, noncancer death attributed to inflammatory diseases in the Iowa Women’s Health Study. Am. J. Clin. Nutr. 2007, 85, 1606–1614.
- Fonseca Wald, E.L.A.; van den Borst, B.; Gosker, H.R.; Schols, A. Dietary fibre and fatty acids in chronic obstructive pulmonary disease risk and progression: A systematic review. Respirology 2014, 19, 176–184.
- Esposito, K.; Giugliano, D. Whole-grain intake cools down inflammation. Am. J. Clin. Nutr. 2006, 83, 1440–1441.
- Kan, H.; Stevens, J.; Heiss, G.; Rose, K.M.; London, S.J. Dietary fiber, lung function, and chronic obstructive pulmonary disease in the atherosclerosis risk in communities study. Am. J. Epidemiol. 2008, 167, 570–578.
- Varraso, R.; Willett, W.C.; Camargo, C.A., Jr. Prospective study of dietary fiber and risk of chronic obstructive pulmonary disease among US women and men. Am. J. Epidemiol. 2010, 171, 776–784.
- Kaluza, J.; Harris, H.; Wallin, A.; Linden, A.; Wolk, A. Dietary Fiber Intake and Risk of Chronic Obstructive Pulmonary Disease: A Prospective Cohort Study of Men. Epidemiology 2018, 29, 254–260.
- Frantz, S.; Wollmer, P.; Dencker, M.; Engstrom, G.; Nihlen, U. Associations between lung function and alcohol consumption–Assessed by both a questionnaire and a blood marker. Respir. Med. 2014, 108, 114–121.
- Schunemann, H.J.; Grant, B.J.; Freudenheim, J.L.; Muti, P.; McCann, S.E.; Kudalkar, D.; Ram, M.; Nochajski, T.; Russell, M.; Trevisan, M. Beverage specific alcohol intake in a population-based study: Evidence for a positive association between pulmonary function and wine intake. BMC Pulm. Med. 2002, 2, 3.
- Siedlinski, M.; Boer, J.M.; Smit, H.A.; Postma, D.S.; Boezen, H.M. Dietary factors and lung function in the general population: Wine and resveratrol intake. Eur. Respir. J. 2012, 39, 385–391.
- Sisson, J.H. Alcohol and airways function in health and disease. Alcohol 2007, 41, 293–307.
- Donnelly, L.E.; Newton, R.; Kennedy, G.E.; Fenwick, P.S.; Leung, R.H.; Ito, K.; Russell, R.E.; Barnes, P.J. Anti-inflammatory effects of resveratrol in lung epithelial cells: Molecular mechanisms. Am. J. Physiol. Lung Cell. Mol. Physiol. 2004, 287, L774–L783.
- Culpitt, S.V.; Rogers, D.F.; Fenwick, P.S.; Shah, P.; De Matos, C.; Russell, R.E.; Barnes, P.J.; Donnelly, L.E. Inhibition by red wine extract, resveratrol, of cytokine release by alveolar macrophages in COPD. Thorax 2003, 58, 942–946.
- Knobloch, J.; Sibbing, B.; Jungck, D.; Lin, Y.; Urban, K.; Stoelben, E.; Strauch, J.; Koch, A. Resveratrol impairs the release of steroid-resistant inflammatory cytokines from human airway smooth muscle cells in chronic obstructive pulmonary disease. J. Pharmacol. Exp. Ther. 2010, 335, 788–798.
- Farazuddin, M.; Mishra, R.; Jing, Y.; Srivastava, V.; Comstock, A.T.; Sajjan, U.S. Quercetin prevents rhinovirus-induced progression of lung disease in mice with COPD phenotype. PLoS ONE 2018, 13, e0199612.
- Hanson, C.; Sayles, H.; Rutten, E.; Wouters, E.F.M.; MacNee, W.; Calverley, P.; Meza, J.L.; Rennard, S. The Association Between Dietary Intake and Phenotypical Characteristics of COPD in the ECLIPSE Cohort. Chronic Obstr. Pulm. Dis. 2014, 1, 115–124.
- Black, P.N.; Scragg, R. Relationship between serum 25-hydroxyvitamin d and pulmonary function in the third national health and nutrition examination survey. Chest 2005, 128, 3792–3798.
- Afzal, S.; Lange, P.; Bojesen, S.E.; Freiberg, J.J.; Nordestgaard, B.G. Plasma 25-hydroxyvitamin D, lung function and risk of chronic obstructive pulmonary disease. Thorax 2014, 69, 24–31.
- Mulrennan, S.; Knuiman, M.; Walsh, J.P.; Hui, J.; Hunter, M.; Divitini, M.; Zhu, K.; Cooke, B.R.; Musk, A.W.B.; James, A.; et al. Vitamin D and respiratory health in the Busselton Healthy Ageing Study. Respirology 2018, 23, 576–582.
- Janssens, W.; Bouillon, R.; Claes, B.; Carremans, C.; Lehouck, A.; Buysschaert, I.; Coolen, J.; Mathieu, C.; Decramer, M.; Lambrechts, D.; et al. Vitamin D deficiency is highly prevalent in COPD and correlates with variants in the vitamin D-binding gene. Thorax 2010, 65, 215–220.
- Jolliffe, D.A.; Greenberg, L.; Hooper, R.L.; Mathyssen, C.; Rafiq, R.; de Jongh, R.T.; Camargo, C.A.; Griffiths, C.J.; Janssens, W.; Martineau, A.R.; et al. Vitamin D to prevent exacerbations of COPD: Systematic review and meta-analysis of individual participant data from randomised controlled trials. Thorax 2019, 74, 337–345.
- Alfaro, T.M.; Monteiro, R.A.; Cunha, R.A.; Cordeiro, C.R. Chronic coffee consumption and respiratory disease: A systematic review. Clin. Respir. J. 2018, 12, 1283–1294.
- Simopoulos, A.P. The importance of the omega-6/omega-3 fatty acid ratio in cardiovascular disease and other chronic diseases. Exp. Biol. Med. (Maywood) 2008, 233, 674–688.
- Massaro, M.; Scoditti, E.; Carluccio, M.A.; De Caterina, R. Basic mechanisms behind the effects of n-3 fatty acids on cardiovascular disease. Prostaglandins Leukot. Essent. Fatty Acids 2008, 79, 109–115.
- Micha, R.; Wallace, S.K.; Mozaffarian, D. Red and processed meat consumption and risk of incident coronary heart disease, stroke, and diabetes mellitus: A systematic review and meta-analysis. Circulation 2010, 121, 2271–2283.
- Johnson, I.T. The cancer risk related to meat and meat products. Br. Med. Bull. 2017, 121, 73–81.
- Larsson, S.C.; Orsini, N. Red meat and processed meat consumption and all-cause mortality: A meta-analysis. Am. J. Epidemiol. 2014, 179, 282–289.
- Jiang, R.; Paik, D.C.; Hankinson, J.L.; Barr, R.G. Cured meat consumption, lung function, and chronic obstructive pulmonary disease among United States adults. Am. J. Respir. Crit. Care Med. 2007, 175, 798–804.
- Varraso, R.; Jiang, R.; Barr, R.G.; Willett, W.C.; Camargo, C.A., Jr. Prospective study of cured meats consumption and risk of chronic obstructive pulmonary disease in men. Am. J. Epidemiol. 2007, 166, 1438–1445.
- Jiang, R.; Camargo, C.A., Jr.; Varraso, R.; Paik, D.C.; Willett, W.C.; Barr, R.G. Consumption of cured meats and prospective risk of chronic obstructive pulmonary disease in women. Am. J. Clin. Nutr. 2008, 87, 1002–1008.
- Kaluza, J.; Larsson, S.C.; Linden, A.; Wolk, A. Consumption of Unprocessed and Processed Red Meat and the Risk of Chronic Obstructive Pulmonary Disease: A Prospective Cohort Study of Men. Am. J. Epidemiol. 2016, 184, 829–836.
- Kaluza, J.; Harris, H.; Linden, A.; Wolk, A. Long-term unprocessed and processed red meat consumption and risk of chronic obstructive pulmonary disease: A prospective cohort study of women. Eur. J. Nutr. 2019, 58, 665–672.
- de Batlle, J.; Mendez, M.; Romieu, I.; Balcells, E.; Benet, M.; Donaire-Gonzalez, D.; Ferrer, J.J.; Orozco-Levi, M.; Anto, J.M.; Garcia-Aymerich, J.; et al. Cured meat consumption increases risk of readmission in COPD patients. Eur. Respir. J. 2012, 40, 555–560.
- Salari-Moghaddam, A.; Milajerdi, A.; Larijani, B.; Esmaillzadeh, A. Processed red meat intake and risk of COPD: A systematic review and dose-response meta-analysis of prospective cohort studies. Clin. Nutr. 2018, 38, 1109–1116.
- Ricciardolo, F.L.; Caramori, G.; Ito, K.; Capelli, A.; Brun, P.; Abatangelo, G.; Papi, A.; Chung, K.F.; Adcock, I.; Barnes, P.J.; et al. Nitrosative stress in the bronchial mucosa of severe chronic obstructive pulmonary disease. J. Allergy Clin. Immunol. 2005, 116, 1028–1035.
- Shuval, H.I.; Gruener, N. Epidemiological and toxicological aspects of nitrates and nitrites in the environment. Am. J. Public Health 1972, 62, 1045–1052.
- Yi, B.; Titze, J.; Rykova, M.; Feuerecker, M.; Vassilieva, G.; Nichiporuk, I.; Schelling, G.; Morukov, B.; Chouker, A. Effects of dietary salt levels on monocytic cells and immune responses in healthy human subjects: A longitudinal study. Transl. Res. 2015, 166, 103–110.
- Tashiro, H.; Takahashi, K.; Sadamatsu, H.; Kato, G.; Kurata, K.; Kimura, S.; Sueoka-Aragane, N. Saturated Fatty Acid Increases Lung Macrophages and Augments House Dust Mite-Induced Airway Inflammation in Mice Fed with High-Fat Diet. Inflammation 2017, 40, 1072–1086.
- Wood, L.G.; Attia, J.; McElduff, P.; McEvoy, M.; Gibson, P.G. Assessment of dietary fat intake and innate immune activation as risk factors for impaired lung function. Eur. J. Clin. Nutr. 2010, 64, 818–825.
- Zong, G.; Li, Y.; Wanders, A.J.; Alssema, M.; Zock, P.L.; Willett, W.C.; Hu, F.B.; Sun, Q. Intake of individual saturated fatty acids and risk of coronary heart disease in US men and women: Two prospective longitudinal cohort studies. BMJ 2016, 355, i5796.
- Jiang, R.; Jacobs, D.R.; He, K.; Hoffman, E.; Hankinson, J.; Nettleton, J.A.; Barr, R.G. Associations of dairy intake with CT lung density and lung function. J. Am. Coll. Nutr. 2010, 29, 494–502.
- Cornell, K.; Alam, M.; Lyden, E.; Wood, L.; LeVan, T.D.; Nordgren, T.M.; Bailey, K.; Hanson, C. Saturated Fat Intake Is Associated with Lung Function in Individuals with Airflow Obstruction: Results from NHANES 2007(-)2012. Nutrients 2019, 11.
- Esposito, K.; Nappo, F.; Marfella, R.; Giugliano, G.; Giugliano, F.; Ciotola, M.; Quagliaro, L.; Ceriello, A.; Giugliano, D. Inflammatory cytokine concentrations are acutely increased by hyperglycemia in humans: Role of oxidative stress. Circulation 2002, 106, 2067–2072.
- Walter, R.E.; Beiser, A.; Givelber, R.J.; O’Connor, G.T.; Gottlieb, D.J. Association between glycemic state and lung function: The Framingham Heart Study. Am. J. Respir. Crit. Care Med. 2003, 167, 911–916.
- Baker, E.H.; Janaway, C.H.; Philips, B.J.; Brennan, A.L.; Baines, D.L.; Wood, D.M.; Jones, P.W. Hyperglycaemia is associated with poor outcomes in patients admitted to hospital with acute exacerbations of chronic obstructive pulmonary disease. Thorax 2006, 61, 284–289.
- Mallia, P.; Webber, J.; Gill, S.K.; Trujillo-Torralbo, M.B.; Calderazzo, M.A.; Finney, L.; Bakhsoliani, E.; Farne, H.; Singanayagam, A.; Footitt, J.; et al. Role of airway glucose in bacterial infections in patients with chronic obstructive pulmonary disease. J. Allergy Clin. Immunol. 2018, 142, 815–823.
- Wu, L.; Ma, L.; Nicholson, L.F.; Black, P.N. Advanced glycation end products and its receptor (RAGE) are increased in patients with COPD. Respir. Med. 2011, 105, 329–336.
- Shi, Z.; Dal Grande, E.; Taylor, A.W.; Gill, T.K.; Adams, R.; Wittert, G.A. Association between soft drink consumption and asthma and chronic obstructive pulmonary disease among adults in Australia. Respirology 2012, 17, 363–369.
- DeChristopher, L.R.; Uribarri, J.; Tucker, K.L. Intake of high fructose corn syrup sweetened soft drinks is associated with prevalent chronic bronchitis in U.S. Adults, ages 20–55 y. Nutr. J. 2015, 14, 107.
- DeChristopher, L.R.; Uribarri, J.; Tucker, K.L. Intakes of apple juice, fruit drinks and soda are associated with prevalent asthma in US children aged 2–9 years. Public Health Nutr. 2016, 19, 123–130.
- Butler, L.M.; Koh, W.P.; Lee, H.P.; Tseng, M.; Yu, M.C.; London, S.J. Singapore Chinese Health Study. Prospective study of dietary patterns and persistent cough with phlegm among Chinese Singaporeans. Am. J. Respir. Crit. Care Med. 2006, 173, 264–270.
- Varraso, R.; Fung, T.T.; Hu, F.B.; Willett, W.; Camargo, C.A. Prospective study of dietary patterns and chronic obstructive pulmonary disease among US men. Thorax 2007, 62, 786–791.
- Varraso, R.; Fung, T.T.; Barr, R.G.; Hu, F.B.; Willett, W.; Camargo, C.A., Jr. Prospective study of dietary patterns and chronic obstructive pulmonary disease among US women. Am. J. Clin. Nutr. 2007, 86, 488–495.
- Shaheen, S.O.; Jameson, K.A.; Syddall, H.E.; Aihie Sayer, A.; Dennison, E.M.; Cooper, C.; Robinson, S.M. Hertfordshire Cohort Study Group. The relationship of dietary patterns with adult lung function and COPD. Eur. Respir. J. 2010, 36, 277–284.
- Steinemann, N.; Grize, L.; Pons, M.; Rothe, T.; Stolz, D.; Turk, A.; Schindler, C.; Brombach, C.; Probst-Hensch, N. Associations between Dietary Patterns and Post-Bronchodilation Lung Function in the SAPALDIA Cohort. Respiration 2018, 95, 454–463.
- Brigham, E.P.; Steffen, L.M.; London, S.J.; Boyce, D.; Diette, G.B.; Hansel, N.N.; Rice, J.; McCormack, M.C. Diet Pattern and Respiratory Morbidity in the Atherosclerosis Risk in Communities Study. Ann. Am. Thorac. Soc. 2018, 15, 675–682.
- McKeever, T.M.; Lewis, S.A.; Cassano, P.A.; Ocke, M.; Burney, P.; Britton, J.; Smit, H.A. Patterns of dietary intake and relation to respiratory disease, forced expiratory volume in 1 s, and decline in 5-y forced expiratory volume. Am. J. Clin. Nutr. 2010, 92, 408–415.
- Sorli-Aguilar, M.; Martin-Lujan, F.; Flores-Mateo, G.; Arija-Val, V.; Basora-Gallisa, J.; Sola-Alberich, R.; RESET Study Group Investigators. Dietary patterns are associated with lung function among Spanish smokers without respiratory disease. BMC Pulm. Med. 2016, 16, 162.
- Varraso, R.; Chiuve, S.E.; Fung, T.T.; Barr, R.G.; Hu, F.B.; Willett, W.C.; Camargo, C.A. Alternate Healthy Eating Index 2010 and risk of chronic obstructive pulmonary disease among US women and men: Prospective study. BMJ 2015, 350, h286.
- Yazdanpanah, L.; Paknahad, Z.; Moosavi, A.J.; Maracy, M.R.; Zaker, M.M. The relationship between different diet quality indices and severity of airflow obstruction among COPD patients. Med. J. Islam. Repub. Iran 2016, 30, 380.
- Gutierrez-Carrasquilla, L.; Sanchez, E.; Hernandez, M.; Polanco, D.; Salas-Salvado, J.; Betriu, A.; Gaeta, A.M.; Carmona, P.; Purroy, F.; Pamplona, R.; et al. Effects of Mediterranean Diet and Physical Activity on Pulmonary Function: A Cross-Sectional Analysis in the ILERVAS Project. Nutrients 2019, 11.
