Human exposure to lead can occur in a variety of ways, all of which involve exposure to potentially toxic elements as environmental pollutants. Lead enters the body via ingestion and inhalation from sources such as soil, food, lead dust and lead in products of everyday use and in the workplace. The aim of this review is to describe the toxic effects of lead on the human body from conception to adulthood, and to review the situation regarding lead toxicity in Poland. Results: Pb is very dangerous when it is absorbed and accumulates in the main organs of the body, where it can cause a range of symptoms that vary from person to person, the time of exposure and dose. Lead in adults can cause an increase in blood pressure, slow nerve conduction, fatigue, mood swings, drowsiness, impaired concentration, fertility disorders, decreased sex drive, headaches, constipation and, in severe cases, encephalopathy or death. Conclusions: Exposure to lead in Poland remains an important public health problem. This review will cover the range of lead exposures, from mild to heavy. Public health interventions and policies also are needed to reduce occupational and environmental exposure to this element.
- lead absorption
- lead poisoning
- lead’s effects
- lead exposure
1. Definition
Lead (Pb) is a potentially toxic element that, when absorbed by the body, accumulates in blood and bones, as well as in organs such as the liver, kidneys, brain and skin. Its negative health effects can be both acute and chronic, because the human body poorly excretes Pb. In humans, lead has been shown to affect the function of the reproductive, hepatic, endocrine, immune and gastrointestinal systems[1]. There is limited evidence of a carcinogenic effect of lead and its inorganic compounds on humans[2].
2. Introduction
Human exposure to lead can occur in a variety of ways, all of which involve environmental pollution. Lead enters the body via ingestion or inhalation from sources such as soil, food, lead dust and contact with lead in products of everyday use and in the workplace. In the work environment, the main route of absorption of Pb and its compounds is through the respiratory system, although lead is also absorbed via the digestive system (atsdr.cdc.gov)[3][4][5][6][7]. Lead has had many different industrial applications in the past, and is currently used for a range of purposes. Currently, Pb is used in battery plates and equipment for the production of sulfuric acid, cable covers, soldering materials, shields in atomic reactors, aprons and containers for radioactive materials, in the paint and ceramics, and chemical and construction industries, and in the production of bearings and printing fonts, and aviation gasoline, etc. Until recently, lead-based house paint and tetraethyl lead in gasoline were major sources of environmental lead[2][3][4]. Toxic exposure to lead in Poland remains an important public health problem. Constantly expanding knowledge in the field of pollution by toxic elements, including lead, is particularly important, because they are broadly harmful to health and even human life. In the case of Pb, it is necessary to determine the levels of exposure as well as absorption, as the effects of Pb poisoning are often visible only after a few years.
3. Lead’s Effects
3.1. Metabolic and Genetic Effects
Lead impairs multiple biochemical processes, including inhibiting calcium and reacting with proteins. Upon entering the body, Pb takes the place of calcium and then interacts with biological molecules, interfering with their normal function. Lead reduces the activity of various enzymes, causing changes in their structure, and inhibits their activity by competing with the necessary cations for binding sites. Oxidative stress caused by lead is the main mechanism responsible for its toxicity, causing changes in the composition of fatty acids in membranes (affecting processes such as exocytosis and endocytosis, and signal transduction processes). Pb can also cause gene expression alterations. Some research has investigated the effects of Pb on the activity of glucose-6-phosphate dehydrogenase (G6PD). It has been shown that by causing anemia, it may interfere with the integrity of the RBC membrane, making it more fragile. Pb can also inhibit the enzyme ferrochelatase, reducing iron (Fe) incorporation into heme. Lead inhibits the δ-aminolevulinic acid dehydratase (δ-ALAD) enzyme, leading to increased blood levels of δ-aminolevulinic acid (δ-ALA). Pb-induced oxidative damage is the result of a disturbance in the balance of glutathione (GSH) to glutathione disulfide (GSSG). The presence of lead in the body can cause rapid depletion of antioxidants in the body, and can increase the production of reactive oxygen, as well as reactive forms of nitrogen. Thus, increased oxidative stress causes a reduction in the levels of glutathione reductase, leading to a reduction in the concentration of the antioxidant glutathione[8][9][10].
3.2. Location of Lead in the Body
Most lead is stored in the bones[11][12], where it is not uniformly distributed. It tends to accumulate in bone regions undergoing the most active calcification at the time of exposure. The rates of development and accumulation suggest that accumulation will occur mainly in the trabecular bone during childhood, and in the cortical bone in adulthood. Bone-to-blood lead mobilization increases with age, broken bones, chronic disease, hyperthyroidism, kidney disease, pregnancy and lactation, menopause and physiologic stress. Calcium deficiency exacerbates bone-to-blood lead mobilization in all of the above instances[1][3]. Recently, research in southern Spain identified elevated lead levels in adipose tissue, although the authors noted that further research is needed on this subject[13].
3.3. Children
WHO experts stress the importance of Pb control among children, because research consistently shows that it adversely affects the central nervous system and development[14]. Pb is especially harmful to children under the age of six, most likely because of the rapid brain growth and development with associated periods of heightened vulnerability, and because of high demand for nutrients[2][15][14]. Pb can interfere with the ability to learn, impair memory, lower IQ and interfere with growth and development. Pb has documented effects on speech, hearing, hyperactivity, nerve conduction, intestinal discomfort, constipation, vomiting, weight loss and muscle aches. At high blood concentrations (Table 1), lead poisoning can lead to anemia, nephropathy, paralysis, convulsions or death[4][8].
Table 1. Symptoms of poisoning according to the degree of exposure in children and adults (Adopted from[4]).
|
Blood Lead Level (µg/L) |
Degrees of Lead Poisoning |
Symptoms |
|
|
Adults |
Children |
||
|
<10 |
low |
passing through the placenta into the fetal bloodstream |
IQ reduction, learning and memory disabilities, growth disorders, reduced development, motor coordination, hearing, speech and verbal skills, symptoms of hyperactivity |
|
10–40 |
mild |
elevated blood pressure, slowed nerve conduction |
deceleration of nerve conduction and vitamin D metabolism, impaired hemoglobin synthesis, sporadic intestinal discomfort, muscle pain, irritability, fatigue, apathy |
|
40–70 |
moderate |
drowsiness, fatigue, mood swings, reduced mental abilities, impaired fertility, chronic hypertension, impaired hemoglobin synthesis |
difficulty concentrating, trembling, fatigue, muscular weakness, headache, vomiting, constipation, weight loss |
|
70–100 |
serious |
metallic taste in the mouth, constipation, headaches, abdominal pain, insomnia, memory loss, decreased sex drive, nephropathy |
colic (severe intestinal musculoskeletal contractions), lead limbs (dark teeth and/or gums), anemia, nephropathy, encephalopathy, paralysis |
|
>100 |
acute poisoning |
encephalopathy, anemia, death (> 150 µg/L) |
convulsions, death (usually below 150 µg/L) |
Damage to the child due to lead can begin as early as pregnancy. Maternal lead can be passed through the placenta to the developing fetus[8][16]. The Pb content in the placenta is the result of many complex biochemical reactions and various factors related to the mother’s body. The concentration of Pb in umbilical cord blood can be up to 85% of that in the mother’s blood. When a woman becomes pregnant, the lead stored in her bones can be released and transferred through the blood to the fetus, especially if the mother’s calcium intake is low. Therefore, fetal development can be influenced by both current and past maternal exposure to Pb via lead stored in the mother’s bones[17][18].
Research has found that even slight Pb exposure is associated with increased the risk of miscarriage, stillbirth, low birth weight and underdeveloped children. It is still not known what Pb levels can cause mutations and congenital abnormalities in the fetus, as well as the exact mechanisms of these changes. Based on current evidence, the WHO has targeted blood Pb concentrations of 5 μg/dL or less for children. Damage from lead exposure can occur at levels below this value[2][15][14][17][18]. Research on children’s blood pressure and prenatal lead exposure in Mexico City (assessed by lead concentration in mothers’ tibia) found an association between lead and higher blood pressure in girls, but not in boys[19].
Severe lead poisoning in children can cause dementia, irritability, headaches, muscle twitches, hallucinations, memory disorders, learning or behavioral problems, concentration and attention issues, a reduction in IQ, hearing loss, restlessness or hyperactivity. Acute poisoning can lead to convulsions, paralysis and coma. In fatal cases, brain damage can occur due to edema and changes in the blood vessels[4][20][8].
Children are exposed to environmental lead via inhalation and ingestion. Inhalation contributes to higher blood levels in children than in adults. Dirt, dust and food are the largest sources of Pb in children, while ingestion from water is generally a less significant source (Figure 1). The exposure of young children to lead is substantially enhanced by the common infant and toddler behavior of tasting objects, putting hands into the mouth immediately after playing, etc.[2][8]. When young children live in environments with Pb contamination, the ingestion of potentially toxic elements is likely. Increased risk of lead poisoning occurs in families where one parent works in an environment with high levels of lead. Parents who are exposed to Pb in the workplace often bring lead dust into the home on their clothes or skin, thereby increasing the risk of exposure for their children to workplace lead. The monitoring of Pb concentrations in children’s blood is recommended (atsdr.cdc.gov) because of their vulnerability[2][5][6][15].
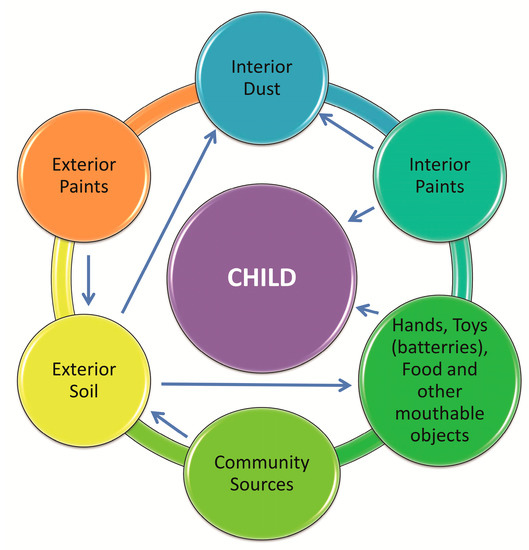
Figure 1. Possible sources of lead poisoning among children in the home environment (Adopted from:[2]).
3.4. Adults
The effects of lead exposure in adults are underappreciated. High lead concentrations can result in serious morphological and functional changes in some organs[2][18]. Lead in adults can cause changes in the nervous system (causing slow nerve conduction, fatigue, mood swings, drowsiness, concentration disorders, headaches, coma), in the circulatory system (increasing blood pressure, and in severe cases, encephalopathy), in the gastrointestinal system (colic/pain, nausea, vomiting, diarrhea and constipation), and hormones (fertility disorders, decreased libido); other effects include astringency of the mouth, metallic taste, and thirst or even death[2]. Additionally, Pb can seriously affect the cardiovascular system. People exposed to very high doses of Pb (blood lead concentrations between 500–870 μg/L blood) can experience sinus node dysfunction, atrioventricular conduction disturbances and atrioventricular block[21]. Pb exposure can also lead to morphological changes in the heart, e.g., visible changes in the electrocardiographic picture, impaired systolic and diastolic function, changes in repolarization dispersion and increased blood pressure[21][10][22].
The relationship between lead concentrations in blood and blood pressure has been widely studied; many researchers have observed a positive relationship, whilst others have not. Any effect of lead on blood pressure would be dependent on the exposure dose and the time of exposure[2]. Even low lead exposure can cause cardiovascular disease[23], is associated with oxidative stress and deficiency of the enzyme catalase, and may contribute to hypertension. Increasing the level of lead in the body causes greater cardiovascular responses to acute stressors. Increased cardiovascular reactivity predicts higher baseline blood pressure, increased left ventricle mass and atherosclerosis in adults. Consequently, increased blood pressure reactions to acute stressors are one of the possible mechanisms by which lead might affect resting blood pressure. Also, lead levels in the blood may affect cardiac output or the total resistance of peripheral vessels, and thus increase the blood pressure response to acute stressors[3][24][25]. Another adverse effect of lead exposure is the effect on the myocytes of the muscular layer of blood vessels. Many researchers have pointed to vasoconstrictor effects in chronic lead intoxication, but this is not firmly established[21]. There is a need to determine the precise role of lead in the pathogenesis of hypertension[22]. A literature review by Navas-Acien et al. concluded that there are causal relationships of lead exposure with hypertension and heart rate variability[26].
Lead compounds can adversely affect blood and the metabolism of blood cells. This red blood cell (RBC) effect manifests in a disorder of cell metabolism of the red blood cell line in the bone marrow or mature erythrocytes. Pb impairs the integrity of the permeability of the membrane, to which RBCs are more susceptible. Heme synthesis is also disturbed by Pb exposure[8].
Lead exposure has been associated with cancer. A meta-analysis assessed the relationship between brain tumors and occupational exposure in several countries (USA, Finland, Sweden, Australia and Russia)[27]. Subsequent research in Finland and the United Kingdom confirmed a relationship between blood lead concentrations and some cancers (brain and lung)[28].
As in children, lead exposure can have adverse effects on the adult nervous system. The blood Pb concentration threshold for asymptomatic CNS function disturbances has been set at 400–600 μg/L (atsdr.cdc.gov)[11]. Adverse effects include impaired visual intelligence, eye-hand coordination and memory, decreased learning ability, impairment of the ability to praise, and potentially, visual and auditory disturbances.
In men who have been exposed to Pb, there can be a reduction in sperm count (> 40 μg/dL) and motility, reduced semen quality, morphological disorders, longer time to pregnancy, sterility/impotency and endocrine disorders.
In women, toxic lead levels can lead to miscarriage[16], low birth weight, premature delivery and developmental problems in children. Lead in the mother’s blood passes to the fetus through the placenta and through breast milk[2]. The symptoms of poisoning according to the degree of exposure in children and adults are shown in Table 1.
Lead colic is a frequent result of short-term exposure to large doses of Pb. At onset of symptoms, the person is hungry, and has indigestion and constipation. Following this comes extensive paroxysmal abdominal pain, pale skin and bradycardia. Acute coronary encephalopathy is rare in adults, but when it has occurred, the blood lead concentrations were 800–1000 to 3000 μg/L (atsdr.cdc.gov)[11].
Studies in an adult Chinese population in Wuhan identified associations between lead in urine and diabetes. However, the authors emphasized that more research is needed to confirm this relationship[29].
A summary of the biological effects of lead is provided in Table 2.
Table 2. The effects of Lead—a summary.
|
Lead’s Effects |
Summary |
|
|
Metabolic and Genetic Effects |
Impairs multiple biochemical processes |
|
|
Interacts with biological molecules |
||
|
Reduces the activity of various enzymes |
||
|
Causes oxidative stress |
||
|
Causes gene expression alterations |
||
|
Inhibits the enzyme ferrochelatase |
||
|
Can causes rapid depletion of antioxidants in the body |
||
|
Can increase the production of reactive oxygen, as well as reactive forms of nitrogen |
||
|
Location of Lead in the Body |
Most lead is stored in the bones |
|
|
Bone-to-blood lead mobilization increases during advanced age |
||
|
Calcium deficiency is exacerbated, bone-to-blood lead mobilization |
||
|
Children |
Adversely affects the central nervous system and development of children |
|
|
Can interfere with the ability to learn, impair memory, lower IQ and interfere with growth and development |
||
|
Can affect speech and hearing, cause hyperactivity, nerve conduction, intestinal discomfort, constipation |
||
|
Vomiting, weight loss muscle aches |
||
|
Can lead to anemia, nephropathy, paralysis, convulsions or death |
||
|
Damage can begin as early as pregnancy |
||
|
Increases the risk of miscarriage, stillbirth, low birth weight and underdeveloped children |
||
|
Children are lead exposed via inhalation and ingestion |
||
|
Increased risk occurs in families where one parent works in an environment where high levels of lead are present |
||
|
Adults |
Can result in serious morphological and functional changes in some organs |
|
|
Can cause changes in the nervous system, the circulatory system, the gastrointestinal system |
||
|
Hormonal, astringency of the mouth, metallic taste in the mouth, and thirst or death |
||
|
Affects myocytes of the muscular layer of blood vessels |
||
|
Can result in an increase in blood pressure (not firmly established) |
||
|
Can adversely affect blood and the metabolism of blood cells |
||
|
Can have adverse effects on the nervous system, fertility, miscarriages |
This entry is adapted from the peer-reviewed paper 10.3390/ijerph17124385
References
- Inga Krzywy; Edward Krzywy; Magdalena Pastuszak-Gabinowska; Andrzej Brodkiewicz; [Lead--is there something to be afraid of?].. Annales Academiae Medicae Stetinensis 2010, 56, 118–128, .
- Ab Latif Wani; Anjum Ara; Jawed Ahmad Usmani; Lead toxicity: a review. Interdisciplinary Toxicology 2015, 8, 55-64, 10.1515/intox-2015-0009.
- Spivey, A. The Weight of Lead: Effects Add Up in Adults. Environ. Health Perspect. 2007, 115, 30–36.
- Giel-Pietraszuk, M.; Hybza, K.; Chełchowska, M.; Barciszewski, J. Mechanisms of lead toxicity. Adv. Cell Biol. 2012, 39, 17–248.
- ATSDR. Lead Toxicity: What Is the biological Fate of Lead in the Body? Environmental Health and Medicine Education. 2017. Available online: https://www.atsdr.cdc.gov/csem/csem.asp?csem=34&po=9 (accessed on 12 June 2017).
- ATSDR. Lead Toxicity: Case Studies in Environmental Medicine (CSEM). Environmental Health and Medicine Education. 2017. Available online: https://www.atsdr.cdc.gov/csem/lead/docs/CSEM-Lead_toxicity_508.pdf (accessed on 12 June 2019).
- Drop, B.; Janiszewska, M.; Barańska, A.; Kanecki, K.; Nitsch-Osuch, A.; Bogdan, M. Satisfaction with Life and Adaptive Reactions in People Treated for Chronic Obstructive Pulmonary Disease. In Clinical Pulmonary Research. Advances in Experimental Medicine and Biology; Pokorski, M., Ed.; Springer International Publishing: Cham, Switzerland, 2018; Volume 1114, pp. 41–47.
- Kanwal Rehman; Fiza Fatima; Iqra Waheed; Muhammad Sajid Hamid Akash; Prevalence of exposure of heavy metals and their impact on health consequences. Journal of Cellular Biochemistry 2017, 119, 157-184, 10.1002/jcb.26234.
- Pinon-Lataillade, G.; Thoreux-Manlay, A.; Coffigny, H.; Monchaux, G.; Masse, R.; Soufir, J.C. Effect of ingestion and inhalation of lead on the reproductive system and fertility of adult male rats and their progeny. Hum. Exp. Toxicol. 1993, 12, 165–172.
- Zhushan, F.; Shuhua, X. The effects of heavy metals on human metabolism. Toxicol. Mech. Meth. 2020, 30, 167–176
- Jakubowski, M.; Lead and its inorganic compounds, other than lead arsenate and lead chromate as Pb, inhalable fraction. Documentation of suggested occupational exposure limits (OELs). Princ. Meth. Assess. 2014, 2, 111–144, .
- Fernando Barbosa; José Eduardo Tanus-Santos; Raquel Fernanda Gerlach; Patrick J. Parsons; A Critical Review of Biomarkers Used for Monitoring Human Exposure to Lead: Advantages, Limitations, and Future Needs. Environmental Health Perspectives 2005, 113, 1669-1674, 10.1289/ehp.7917.
- Carmen Freire; Petra Vrhovnik; Željka Fiket; Inmaculada Salcedo-Bellido; Ruth Echeverría; Piedad Martín-Olmedo; Goran Kniewald; Mariana F. Fernández; Juan Pedro Arrebola; Adipose tissue concentrations of arsenic, nickel, lead, tin, and titanium in adults from GraMo cohort in Southern Spain: An exploratory study. Science of The Total Environment 2020, 719, 137458, 10.1016/j.scitotenv.2020.137458.
- WHO. Expert Consultation. Available Evidence for the Future Update of the WHO Global Air Quality Guidelines (AQGs) (2016). Available online: https://www.euro.who.int/__data/assets/pdf_file/0013/301720/Evidence-future-update-AQGs-mtg-report-Bonn-sept-oct-15.pdf (accessed on 1 December 2015)
- Staniak, S.; Sources and levels of lead in food. Pol. J. Agron. 2014, 19, 36–45, .
- Wioleta Omeljaniuk; Katarzyna Socha; Jolanta Soroczyńska; Angelika Charkiewicz; Tadeusz Laudański; Marek Kulikowski; Edward Kobylec; Maria Borawska; Cadmium and Lead in Women Who Miscarried. Clinical Laboratory 2018, 64, 59-67, 10.7754/clin.lab.2017.170611.
- Centers for Disease Control and Prevention (CDC). Guidelines for the Identification and Management of Lead Exposure in Pregnant and Lactating Women. Atlanta. 2010. Available online: https://www.cdc.gov/nceh/lead/publications/leadandpregnancy2010.pdf (accessed on 27 July 2012).
- Bellinger, D.C. Prenatal exposures to environmental chemicals and children’s Neurodevelopment: An update. Saf. Health Work 2013, 4, 1–11.
- Aimin Zhang; Howard Hu; Brisa N. Sánchez; Adrienne S. Ettinger; Sung Kyun Park; David Cantonwine; Lourdes Schnaas; Robert O. Wright; Héctor Lamadrid-Figueroa; Martha Maria Tellez-Rojo; et al. Association between Prenatal Lead Exposure and Blood Pressure in Children. Environmental Health Perspectives 2011, 120, 445-450, 10.1289/ehp.1103736.
- Marcela Tamayo Y Ortiz; Martha María Téllez Rojo; Howard Hu; Mauricio Hernández-Ávila; Robert O. Wright; Chitra J. Amarasiriwardena; Nicola Lupoli; Adriana Mercado García; Ivan Pantic; Hector Lamadrid-Figueroa; et al. Lead in candy consumed and blood lead levels of children living in Mexico City. Environmental Research 2016, 147, 497-502, 10.1016/j.envres.2016.03.007.
- Marcin Zawadzki; Rafał Poręba; Paweł Gać; [Mechanisms and toxic effects of lead on the cardiovascular system].. Medycyna Pracy 2006, 57, 543–549, .
- Rafał Poręba; Paweł Gać; Małgorzata Poreba; Arkadiusz Derkacz; Witold Pilecki; Jolanta Antonowicz-Juchniewicz; Ryszard Andrzejak; [Relationship between chronic exposure to lead, cadmium and manganese, blood pressure values and incidence of arterial hypertension].. Medycyna Pracy 2010, 61, 5–14, .
- Bruce P. Lanphear; Stephen Rauch; Peggy Auinger; Ryan W Allen; Richard W Hornung; Low-level lead exposure and mortality in US adults: a population-based cohort study. The Lancet Public Health 2018, 3, e177-e184, 10.1016/s2468-2667(18)30025-2.
- Jintana Sirivarasai; Sukhumpun Kaojarern; Suwannee Chanprasertyothin; Pachara Panpunuan; Krittaya Petchpoung; Aninthita Tatsaneeyapant; Krongtong Yoovathaworn; Thunyachai Sura; Sming Kaojarern; Piyamit Sritara; et al. Environmental Lead Exposure, Catalase Gene, and Markers of Antioxidant and Oxidative Stress Relation to Hypertension: An Analysis Based on the EGAT Study. BioMed Research International 2015, 2015, 1-9, 10.1155/2015/856319.
- Brooks B. Gump; Paul Stewart; Jacki Reihman; Ed Lonky; Tom Darvill; Karen A. Matthews; Patrick J. Parsons; Prenatal and early childhood blood lead levels and cardiovascular functioning in 9½ year old children. Neurotoxicology and Teratology 2005, 27, 655-665, 10.1016/j.ntt.2005.04.002.
- Ana Navas-Acien; Eliseo Guallar; Ellen K. Silbergeld; Stephen J. Rothenberg; Lead Exposure and Cardiovascular Disease—A Systematic Review. Environmental Health Perspectives 2007, 115, 472-482, 10.1289/ehp.9785.
- JoonHo Ahn; Mi Yeon Park; Mo-Yeol Kang; In-Soo Shin; SungJae An; Hyoung-Ryoul Kim; Occupational Lead Exposure and Brain Tumors: Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health 2020, 17, 3975, 10.3390/ijerph17113975.
- Kyle Steenland; Vaughn Barry; Ahti Anttila; Markku Sallmen; William Mueller; Peter Ritchie; Damien Martin McElvenny; Kurt Straif; Cancer incidence among workers with blood lead measurements in two countries. Occupational and Environmental Medicine 2019, 76, 603-610, 10.1136/oemed-2019-105786.
- Wei Feng; Xiuqing Cui; Bing Liu; Chuanyao Liu; Yang Xiao; Wei Lu; Huan Guo; Meian He; Xiaomin Zhang; Jing Yuan; et al. Association of Urinary Metal Profiles with Altered Glucose Levels and Diabetes Risk: A Population-Based Study in China. PLOS ONE 2015, 10, e0123742, 10.1371/journal.pone.0123742.
