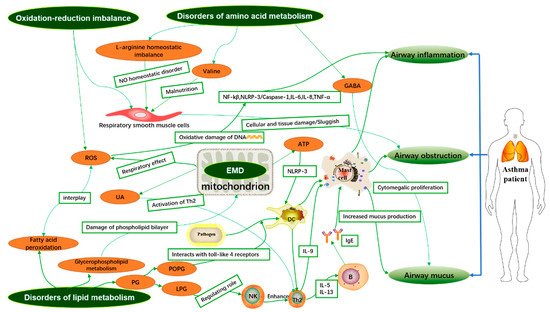
Asthma is a highly heterogeneous disease, but the pathogenesis of asthma is still unclear. It is well known that the airway inflammatory immune response is the pathological basis of asthma. Metabolomics is a systems biology method to analyze the difference of low molecular weight metabolites (<1.5 kDa) and explore the relationship between metabolic small molecules and pathophysiological changes of the organisms.
- metabolomics
- asthma
- inflammation
- pathogenesis
1. Introduction
2. Integrative Analysis of Asthma-Related Metabolites and Metabolic Pathways in Different Samples
| Author and Year | Subjects | Sample/Methods | Significant Metabolites | |
|---|---|---|---|---|
| Up | Down | |||
| Pang, Z. et al. (2018) [6] | eosinophilic asthmatics (EA, n = 13), noneosinophilic asthmatics (NEA, n = 16), and healthy controls (HC, n = 15) | Serum/UPLC-MS/MS | Monosaccharides, LysoPC(18:1), Retinyl ester, PC(18:1/2:0), LysoPC(o-18:0), Arachidonic acid, PE(18:3/14:0), PC(16:0/18:1) | Glycerophosphocholine, PS(18:0/22:5), Cholesterol glucuronide, Phytosphingosine, Sphinganine, LysoPC(p-18:1), Retinols, PC(20:4/16:1) |
| Guo, C. et al. (2021) [7] | 51 asthma patients and 9 healthy individuals | Serum/LC-MS | No report | SM 34:2, SM 38:1, SM 40:1 |
| Chiu, C.-Y. et al. (2020) [8] | Asthma (n = 28) and healthy controls (n = 26) | Plasma and urine/NMR | Histidine | 1-methylnicotinamide, trimethylamine N-oxide (TMAO) |
| Turi, K.N. et al. (2021) [9] | 600 infants from 3 independent cohorts | Plasma/LC-MS | Succinate, N-(2-furoyl)glycine | Iminodiacetate (IDA) |
| Jiang, T. et al. (2021) [10] | 28 healthy controls and 33 outpatients with asthma | Plasma/LC-MS/MS | Phosphatidylethanolamine (PE) (18:1p/22:6), PE (20:0/18:1), PE (38:1), sphingomyelin (SM) (d18:1/18:1), triglyceride (TG) (16:0/16:0/18:1) | Phosphatidylinositol (PI) (16:0/20:4), TG (17:0/18:1/18:1), phosphatidylglycerol (PG) (44:0), ceramide (Cer) (d16:0/27:2), lysophosphatidylcholine (LPC) (22:4) |
| Bian, X. et al. (2017) [11] | 15 healthy human and 15 asthma patients | Serum/UHPLC-Q-TOF-MS | Ursodeoxycholic acid, Deoxycholic acid, Isodeoxycholic acid, EPA | Palmitic acid, Lauric acid |
| Matysiak, J. et al. (2020) [12] | asthmatic children (n = 13) and the control group (n = 17) | Blood/LC-MS/MS | l-Arginine, Β-Alanine, Ƴ-Amino-N-Butyric Acid, l-Histidine, Hydroxy-l-Proline | d,l-Β-Aminoisobutyric Acid, Taurine, l-Tryptophan, l-Valine |
| Ghosh, N. et al. (2020) [13] | (i) controls = 33 (ii) asthma = 34 (iii) COPD = 30 and (iv) ACO = 35 | Serum/GC-MS | 2-palmitoylglycerol, cholesterol, serine, threonine, Ethanolamine, Glucose, Stearic acid, Linoleic acid, d-Mannose, Succinic acid | Lactic acid, 2-palmitoylglycerol |
| Liang, Y. et al. (2019) [14] | A total of 17 patients with mildly persistent asthma, 17 patients with stable COPD, and 15 healthy subjects | Serum/LC-MS | Hypoxanthine, P-chlorophenylalanine, Inosine, Theophylline, Bilirubin, Palmitic acid | l-Glutamine, Glycerophosphocholine, Succinate, Xanthine, Arachidonic Acid, l-Pyroglutamic acid, Indoxyl sulfate, l-Valine, l-Norleucine, l-Leucine, l-Phenylalanine |
| Chiu, C.-Y. et al. (2018) [15] | Asthma (n = 30) and healthy controls (n = 30) | Urine/NMR | Guanidoacetic acid | 1-methylnicotinamide, allantoin |
| Li, S. et al. (2020) [16] | Asthmatic children (n = 30) and healthy controls (n = 30) | Urine/GC-MS | l-allothreonine 1, stearic acid, succinic acid, 2-hydroxybutanoic acid, azelaic acid, gentiobiose 2, tyramine, leucine, d-altrose 1, d-erythrosphingosine 1, citraconic acid 4 | Valine, uric acid, methionine 1, 3,4-dihydroxycinnamic acid, purine riboside, malonic acid 1, cysteine, erythrose 1, lactamide 1 |
| Chawes, B.L. et al.(2018) [17] | 171 and 161 healthy neonates born from mothers with asthma | Urine/UPLC-MS | bile acid taurochenodeoxycholate-3-sulfate, fatty acid 3-hydroxytetradecanedioic acid | glucoronidated steroid compound |
| Carraro, S. et al. (2018) [18] | Children for transient wheezing (n = 16) and early-onset asthma (n = 16) | Urine/UPLC-MS | 4-(4-deoxy-α-d-gluc-4-enuronosyl)-d-galacturonate, Glutaric acid, 4-hydroxynonenal, Phosphatidyl glycerol, 3-methyluridine, Steroid O-sulfate, 5-hydroxy-l-tryptophan, 3-indoleacetic acid, Tiglylglycine, Indole, Cytosine, N-acetylputrescine, Indole-3-acetamide, 6-methyladenine, 5-methylcytosine, N-acryloylglycine, Hydroxyphenyllactic acid | Oxoadipic acid, (-)-epinephrine, l-tyrosine, 3-hydroxyhippuric acid, Benzoic acid,3-hydroxy-sebacic acid, Dihydroferulic acid 4-sulfate, p-cresol, Indolelactic acid, N-acetyl-l-phenylalanine, N2-acetyl-ornithine |
| Tao, J.-L. et al. (2019) [19] | Children for healthy control (n = 29), uncontrolled asthma (n = 37) or controlled asthma (n = 43) | Urine/GC-MS | Aspartic acid, Xanthosine, Hypoxanthine, N-acetylgalactosamine |
Stearic acid, Heptadecanoic acid, Uric acid, d-threitol |
| Adamko, D.J. et al. (2015) [20] | Adults with asthma (n = 58) and COPD (n = 24) | Urine/NMR | Glutamine, succinate, uracil, pantothenate | Arginine, dimethylamine, 3-Hydroxyisovalerate, betaine, choline, glucose, 1-methylnicotinamide |
| Ravi, A. et al. (2021) [21] | Healthy controls (n = 7) and patients with severe asthma (n = 9) | BECs/UPLC-MS | Phosphatidylcholines, lysophosphatidylcholines, lysophosphatidylethanolamines, bis(monoacylglycero)phosphates | No report |
| Chang-Chien, J. et al.(2020) [22] | stable asthma (n = 92) and non-asthmatic controls (n = 73) | EBC/NMR | lactate, formate, butyric acid, isobutyrate | No report |
| Ferraro, V.A. et al. (2020) [23] | asthmatic children (n = 26) and healthy children (n = 16) | EBC/UPLC-MS | 9-amino-nonanoic acid, 12-amino-dodecanoic acid, lactone of PGF-MUM, N-linoleoyl taurine, 17-phenoxy trinor PGF2α ethyl amide, lysoPC (18:2(9Z,12Z)) | No report |
| Kang, Y.P. et al. (2014) [24] | 38 asthma patients and 13 healthy subjects | BALF/HPLC-QTOF-MS | lysophosphatidylcholine (LPC), phosphatidylcholine (PC), phosphatidylglycerol (PG), phosphatidylserine (PS), sphingomyelin (SM), triglyceride (TG) | No report |
| Tian, M. et al. (2017) [25] | 15 healthy controls and 20 asthma patients | Sputum/UHPLC-QTOF-MS | Glycerol 1-stearate_1, 1-Hexadecanoyl-sn-glycerol_1, Cytidine 2′,3′-cyclic phosphate, 1-Hexadecanoyl-2-(9Z-octadecenoyl)-sn-glycero-3-phospho-(1′-rac-glycerol), 1-Octadecanoyl-2-(9Z-octadecenoyl)-sn-glycero-3-phosphoserine | His-Pro, Thr-Phe_1, Arg-Phe_1, Adenine_1, Phe-Tyr_1, Phe-Gln_1, Tyr-Ala_2, Phe-Ser_1, Urocanic acid |
Up: metabolites are higher in asthmatics than in normal people; Down: metabolites are lower in asthmatics than in normal people. UPLC-MS/MS: ultra-performance liquid chromatography-tandem mass spectrometry; LC-MS: liquid chromatography-mass spectrometry; NMR: nuclear magnetic resonance; LC-MS/MS: liquid chromatography-tandem mass spectrometry; GC-MS: Gas chromatography-mass spectrometry; UPLC-MS: ultra-performance liquid chromatography-mass spectrometry; HPLC-QTOF-MS: high performance liquid chromatography tandem quadrupole time-of-flight mass spectrometry; UHPLC-QTOF-MS: ultra-performance liquid chromatography tandem quadrupole time-of-flight mass spectrometry.
2.1. Analysis of Biomarkers Associated with Asthma in Blood/Serum/Plasma Samples
2.1.1. Phenotypic Identification and Treatment of Asthma
2.1.2. Diagnosis of Asthma
This entry is adapted from the peer-reviewed paper 10.3390/metabo11090567
