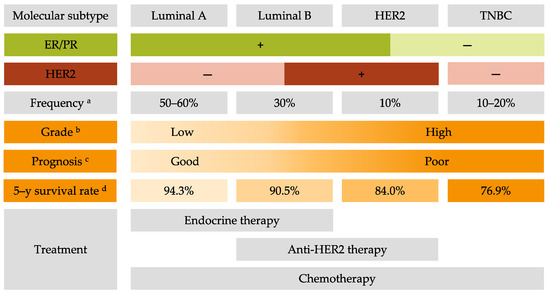
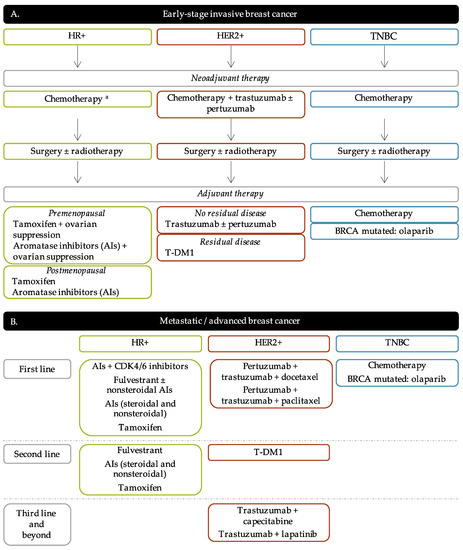
Breast cancer (BC) is the most frequent cancer diagnosed in women worldwide. This heterogeneous disease can be classified into four molecular subtypes (luminal A, luminal B, HER2 and triple-negative breast cancer (TNBC)) according to the expression of the estrogen receptor (ER) and the progesterone receptor (PR), and the overexpression of the human epidermal growth factor receptor 2 (HER2). Current BC treatments target these receptors (endocrine and anti-HER2 therapies) as a personalized treatment. Along with chemotherapy and radiotherapy, these therapies can have severe adverse effects and patients can develop resistance to these agents. Moreover, TNBC do not have standardized treatments. Hence it is essential to develop new treatments to target more effectively each BC subgroup.
- breast cancer
- personalized therapies
- molecular subtypes
- breast cancer treatment
- luminal
- HER2
- TNBC
1. Introduction
2. Common Treatments for All Breast Cancer Subtypes
2.1. Surgery
2.2. Radiotherapy
2.3. Chemotherapy
3. Current Personalized Treatments for Breast Cancer: Strengths and Weaknesses
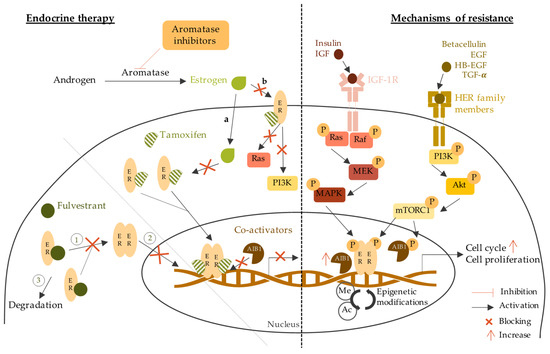
3.1. Endocrine Therapy
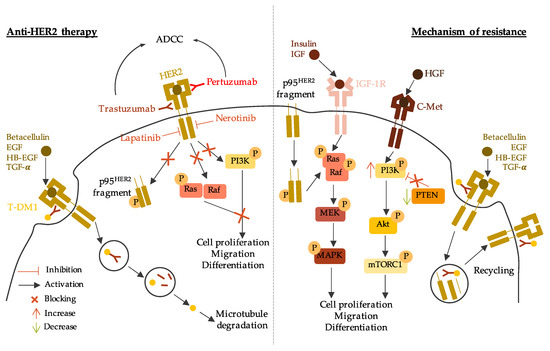
3.2. Anti-HER2 Therapy
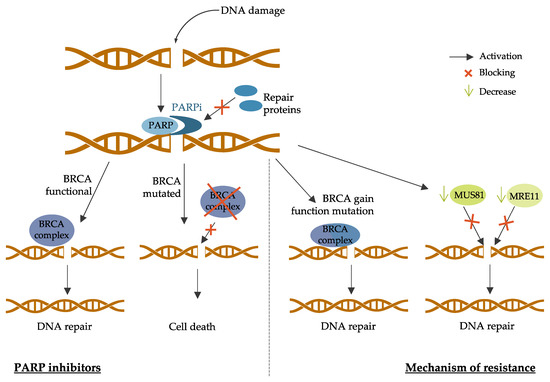
3.3. PARP Inhibitors
4. New Strategies and Challenges for Breast Cancer Treatment
4.1. Emerging Therapies for HR-Positive Breast Cancer
|
Targeted Therapy |
Drug Name |
Trial Number |
Patient Population |
Trial Arms |
Outcomes |
|---|---|---|---|---|---|
|
Pan-PI3K inhibitors |
Buparlisib |
BELLE-2 Phase III NCT01610284 [230] |
HR+/HER2- Postmenopausal Locally advanced or MBC Prior AI treatment |
Buparlisib + fulvestrant vs. placebo + fulvestrant |
PFS 6.9 months vs. 5.0 months (HR 0.78; p = 0.00021) PFS 6.8 months vs. 4.0 months in PI3K mutated (HR 0.76; p = 0.014) |
|
BELLE-3 Phase III NCT01633060 [231] |
HR+/HER2- Postmenopausal Locally advanced or MBC Prior endocrine therapy or mTOR inhibitors |
Buparlisib + fulvestrant vs. placebo + fulvestrant |
PFS 3.9 months vs. 1.8 months (HR 0.67; p = 0.0003) |
||
|
BELLE-4 Phase II/III NCT01572727 [232] |
HER2- Locally advanced or MBC No prior chemotherapy |
Buparlisib + pacliatxel vs. placebo + paclitaxel |
PFS 8.0 months vs. 9.2 months (HR 1.18, 95% CI 0.82–1.68) PFS 9.1 months vs. 9.2 months in PI3K mutated (HR 1.17, 95% 0.63–2.17) |
||
|
Pictilisib |
FERGI Phase II NCT01437566 [233] |
HR+/HER2- Postmenopausal Prior AI treatment |
Pictilisib + fulvestrant vs. placebo + fulvestrant |
PFS 6.6 months vs. 5.1 months (HR 0.74; p = 0.096) PFS 6.5 months vs. 5.1 months in PI3K mutated (HR 0.74; p = 0.268) PFS 5.8 months vs. 3.6 months in non-PI3K mutated (HR 0.72; p = 0.23) |
|
|
PEGGY Phase II NCT01740336 [234] |
HR+/HER2- Locally recurrent or MBC |
Pictilisib + paclitaxel vs. placebo + paclitaxel |
PFS 8.2 months vs. 7.8 months (HR 0.95; p = 0.83) PFS 7.3 months vs. 5.8 months in PI3K mutated (HR 1.06; p = 0.88) |
||
|
Isoform-specific inhibitors |
Alpelisib |
Phase Ib NCT01791478 [235] |
HR+/HER2- Postmenopausal MBC Prior endocrine therapy |
Alpelisib + letrozole |
CBR 35% (44% in patients with PIK3CA mutated and 20% in PIK3CA wild-type tumors; 95% CI [17%; 56%]) |
|
SOLAR-1 Phase III NCT02437318 [236] |
HR+/HER2- Advanced BC Prior endocrine therapy |
Alpelisib + fulvestrant vs. placebo + fulvestrant |
PFS 7.4 months vs. 5.6 months in non-PI3K mutated (HR 0.85, 95% CI 0.58–1.25) PFS 11.0 months vs. 5.7 months in PI3K mutated (HR 0.65; p = 0.00065) |
||
|
NEO-ORB Phase II NCT01923168 [237] |
HR+/HER2- Postmenopausal Early-stage BC Neoadjuvant setting |
Alpelisib + letrozole vs. placebo + letrozole |
ORR 43% vs. 45% (PIK3CA mutant), 63% vs. 61% (PIK3CA wildtype) pCR rates low in all groups |
||
|
Taselisib |
SANDPIPER Phase III NCT02340221 [238] |
HR+/HER2- Postmenopausal Locally advanced or MBC PIK3CA-mutant Prior AI treatment |
Taselisib + fulvestrant vs. placebo + fulvestrant |
PFS 7.4 months vs. 5.4 months (HR 0.70; p = 0.0037) |
|
|
LORELEI Phase II NCT02273973 [239] |
HR+/HER2- Postmenopausal Early-stage BC Neoadjuvant setting |
Taselisib + letrozole vs. placebo + letrozole |
ORR 50% vs. 39.3% (OR 1.55; p = 0.049) ORR 56.2% vs. 38% in PI3K mutated (OR 2.03; p = 0.033) No significant difference in pCR |
||
|
mTOR inhibitors |
Everolimus |
BOLERO-2 Phase III NCT00863655 [240] |
HR+/HER2- Advanced BC Prior AI treatment |
Everolimus + exemestane vs. placebo + exemestane |
PFS 6.9 months vs. 2.8 months (HR 0.43; p < 0.001) |
|
TAMRAD Phase II NCT01298713 [241] |
HR+/HER2- Postmenopausal MBC Prior AI treatment |
Everolimus + tamoxifen vs. tamoxifen alone |
CBR 61% vs. 42% TTP 8.6 months vs. 4.5 months (HR 0.54) |
||
|
PrE0102 Phase II NCT01797120 [242] |
HR+/HER2- Postmenopausal MBC Prior AI treatment |
Everolimus + fulvestrant vs. placebo + fulvestrant |
PFS 10.3 months vs. 5.1 months (HR 0.61; p = 0.02) CBR 63.6% vs. 41.5% (p = 0.01) |
||
|
Akt inhibitors |
Capivasertib |
FAKTION Phase II NCT01992952 [243] |
HR+/HER2- Postmenopausal Locally advanced or MBC Prior AI treatment |
Capivasertib + fulvestrant vs. placebo + fulvestrant |
PFS 10.3 months vs. 4.8 months (HR 0.57; p = 0.0035) |
|
Phase I NCT01226316 [244] |
ER+ AKT1E17K-mutant MBC Prior endocrine treatment |
Capivasertib + fulvestrant vs. Capivasertib alone |
CBR 50% vs. 47% ORR 6% (fulvestrant-pretreated) and 20% (fulvestrant-naïve) vs. 20% |
||
|
CDK4/6 inhibitors |
Palcociclib |
PALOMA-1 Phase II NCT00721409 [126] |
HR+/HER2- Postmenopausal Advanced BC No prior systemic treatment |
Palbocilib + letrozole vs. letrozole alone |
PFS 20.2 months vs. 10.2 months (HR 0.488; p = 0.0004) PFS 26.1 months vs. 5.7 months (HR 0.299; p < 0.0001) in non-Cyclin D1 amplified PFS 18.1 months vs. 11.1 months (HR 0.508; p = 0.0046) in Cyclin D1 amplified |
|
PALOMA-2 Phase III NCT01740427 [245] |
HR+/HER2- Postmenopausal Advanced BC No prior systemic treatment |
Palbocilib + letrozole vs. placebo + letrozole |
PFS 24.8 months vs. 14.5 months (HR 0.58; p < 0.001) |
||
|
PALOMA-3 Phase III NCT01942135 [246] |
HR+/HER2- MBC Prior endocrine therapy |
Palbociclib + fulvestrant vs. placebo + fulvestrant |
PFS 9.5 months vs. 4.6 months (HR 0.46; p < 0.0001) |
||
|
Ribociclib |
MONALEESA-2 Phase III NCT01958021 [247] |
HR+/HER2- Postmenopausal Advanced or MBC |
Ribociclib + letrozole vs. placebo + letrozole |
PFS 25.3 months vs. 16.0 months (HR 0.568; p < 0.0001) |
|
|
MONALEESA-3 Phase III NCT02422615 [248] |
HR+/HER2- Advanced BC No prior treatment or prior endocrine therapy |
Ribociclib + fulvestrant vs. placebo + fulvestrant |
PFS 20.5 months vs. 12.8 months (HR 0.593; p < 0.001) |
||
|
Abemaciclib |
MONARCH-2 Phase III NCT02107703 [249] |
HR+/HER2- Advanced or MBC Prior endocrine treatment |
Abemaciclib + fulvestrant vs. fulvestrant alone |
PFS 16.4 months vs. 9.3 months (HR 0.553; p < 0.001) |
|
|
MONARCH-3 Phase III NCT02246621 [250] |
HR+/HER2- Advanced or MBC Prior endocrine treatment |
Abemaciclib + anastrozole or letrozole vs. placebo + anastrozole or letrozole |
PFS 28.18 months vs. 14.76 months (HR 0.546; p < 0.0001) |
HR+: hormone receptors positive; HER2-: human epidermal growth factor receptor 2 negative; MBC: metastatic breast cancer; BC: breast cancer; PFS: progression free survival; CBR: clinical benefit rate; ORR: objective response rate; pCR: pathologic complete response; HR: hazard ratio.
4.2. New Strategic Therapies for HER2-Positive Breast Cancer
|
Targeted Therapy |
Drug Name |
Trial Number |
Patient Population |
Trial Arms |
Outcomes |
|---|---|---|---|---|---|
|
Antibodies drug conjugate (ADC) |
Trastuzumab-deruxtcan (DS-8201a) |
DESTINY-Breast01 Phase II NCT03248492 [264] |
HER2+ MBC Prior trastuzumab-emtansine treatment |
Trastuzumab-deruxtcan monotherapy |
PFS 16.4 months |
|
Trastuzumab-duocarmycin (SYD985) |
Phase I dose-escalation and dose-expansion NCT02277717 [265] |
HER2+ Locally advanced or metastatic solid tumors |
Trastuzumab-duocarmycin monotherapy |
ORR 33% |
|
|
Modified antibodies |
Margetuxumab (MGAH22) |
SOPHIA Phase III NCT02492711 [266] |
HER2+ Advanced or MBC Prior anti-HER2 therapies |
Margetuximab + chemotherapy vs. trastuzumab + chemotherapy |
PFS 5.8 months vs. 4.9 months (HR 0.76; p = 0.03) OS 21.6 months vs. 19.8 months (HR 0.89; p = 0.33) ORR 25% vs. 14% (p < 0.001) |
|
Tyrosine kinase inhibitors |
Tucatinib |
HER2CLIMB Phase II NCT02614794 [267] |
HER2+ Locally advanced or MBC Prior anti-HER2 therapies |
Tucatinib + trastuzumab and capecitabine vs. placebo + trastuzumab and capecitabine |
PFS 33.1% (7.8 months) vs. 12.3% (5.6 months) (HR 0.54; p < 0.001) PFS 24.9% vs. 0% (HR 0.48; p < 0.001) in brain metastases patients OS 44.9% vs. 26.6% (HR 0.66; p = 0.005) |
|
Poziotinib |
NOV120101-203 Phase II NCT02418689 [268] |
HER2+ MBC Prior chemotherapy and trastuzumab |
Poziotinib monotherapy |
PFS 4.04 months |
|
|
HER2-derived peptide vaccine |
E75 (NeuVax) |
Phase I/II NCT00841399 NCT00854789 [269] |
HER2+ Node-positive or high-risk node-negative BC HLA2/3+ |
E75 vaccination vs. non-vaccination |
DFS 89.7% vs. 80.2% (p = 0.008) DFS 94.6% in optimal dosed patients (p = 0.005 vs. non-vaccination) |
|
GP2 |
Phase II NCT00524277 [270] |
HER2 (IHC 1-3+) Disease free Node-positive or high-risk node-negative BC HLA2+ |
GP2 + GM-CSF vs. GM-CSF alone |
DFS 94% vs. 85% (p = 0.17) DFS 100% vs. 89% in HER2-IHC3+ (p = 0.08) |
|
|
AE37 |
Phase II NCT00524277 [271] |
HER2 (IHC 1-3+) Node-positive or high-risk node-negative BC |
AE37 + GM-CSF vs. GM-CSF alone |
DFS 80.8% vs. 79.5% (p = 0.70) DFS 77.2% vs. 65.7% (p = 0.21) HER2-low DFS 77.7% vs. 49.0% (p = 0.12) TNBC |
|
|
PI3K inhibitors |
Alpelisib |
Phase I NCT02167854 [272] |
HER2+ MBC with a PIK3CA mutation Prior ado-trastuzumab emtansine and pertuzumab |
Alpelisib + Trastuzumab + LJM716 |
Toxicities limited drug delivery 72% for alpelisib 83% for LJM716 |
|
Phase I NCT02038010 [273] |
HER2+ MBC Prior trastuzumab-based therapy |
Alpelisib + T-DM1 |
PFS 8.1 months ORR 43% CBR 71% and 60% in prior T-DM1 patients |
||
|
Copanlisib |
PantHER Phase Ib NCT02705859 [274] |
HER2+ Advanced BC Prior anti-HER2 therapies |
Copanlisib + trastuzumab |
Stable disease 50% |
|
|
mTOR inhibitors |
Everolimus |
BOLERO-1 Phase III NCT00876395 [275] |
HER2+ Locally advanced BC No prior treatment |
Everolimus + trastuzumab vs. placebo + trastuzumab |
PFS 14.95 months vs. 14.49 months (HR 0.89; p = 0.1166) PFS 20.27 months vs. 13.03 months (HR 0.66; p = 0.0049) |
|
BOLERO-3 Phase III NCT01007942 [276] |
HER2+ Advanced BC Trastuzumab-resistant Prior taxane therapy |
Everolimus + trastuzumab and vinorelbine vs. placebo + trastuzumab and vinorelbine |
PFS 7.00 months vs. 5.78 months (HR 0.78; p = 0.0067) |
||
|
CDK4/6 inhibitors |
Palbociclib |
SOLTI-1303 PATRICIA Phase II NCT02448420 [277] |
HER2+ ER+ or ER- MBC Prior standard therapy including trastuzumab |
Palbociclib + trastuzumab |
PFS 10.6 months (luminal) vs. 4.2 months (non-luminal) (HR 0.40; p = 0.003) |
|
Ribociclib |
Phase Ib/II NCT02657343 [278] |
HER2+ Advanced BC Prior treatment with trastuzumab, pertuzumab, and trastuzumab emtansine |
Ribociclib + trastuzumab |
PFS 1.33 months No dose-limiting toxicities |
|
|
Abemaciclib |
MonarcHER Phase II NCT02675231 [279] |
HER2+ Locally advanced or MBC Prior anti-HER2 therapies |
Abemaciclib + trastuzumab and fulvestrant (A) vs. abemaciclib + trastuzumab (B) vs. standard-of-care chemotherapy + trastuzumab (C) |
PFS 8.3 months (A) vs. 5.7 months (C) (HR 0.67; p = 0.051) PFS 5.7 months (B) vs. 5.7 months (C) (HR 0.97; p = 0.77) |
HER2+: human epidermal growth factor receptor 2 positive; ER+: estrogen receptor positive; HLA2/3: human leucocyte antigen 2/3; MBC: metastatic breast cancer; BC: breast cancer; PFS: progression free survival; CBR: clinical benefit rate; ORR: objective response rate; DFS: disease-free survival OS: overall survival GM-CSF: granulocyte macrophage colony-stimulated factor; HR: hazard ratio.
4.3. Emerging Therapies for Triple Negative Breast Cancer (TNBC)
|
Targeted Therapy |
Drug Name |
Trial Number |
Patient Population |
Trial Arms |
Outcomes |
|---|---|---|---|---|---|
|
Antibodies Drug Conjugate |
Sacituzumab govitecan |
ASCENT Phase III NCT02574455 [309] |
TNBC MBC Prior standard treatment |
Sacituzumab govitecan vs. single-agent chemotherapy |
PFS 5.6 months vs. 1.7 months (HR 0.41; p < 0.001) PFS 12.1 months vs. 6.7 months (HR 0.48; p < 0.001) |
|
VEGF inhibitors |
Bevacizumab |
BEATRICE Phase III NCT00528567 [310] |
Early TNBC Surgery |
Bevacizumab + chemotherapy vs. chemotherapy alone |
IDFS 80% vs. 77% OS 88% vs. 88% |
|
CALGB 40603 Phase II NCT00861705 [311] |
TNBC Stage II to III |
Bevacizumab + chemotherapy vs. chemotherapy alone or Carboplatin + chemotherapy vs. chemotherapy alone |
pCR 59% vs. 48% (p = 0.0089) (Bevacizumab) pCR 60% vs. 44% (p = 0.0018) (Carboplatin) |
||
|
EGFR inhibitors |
Cetuximab |
TBCRC 001 Phase II NCT00232505 [312] |
TNBC MBC |
Cetuximab + carboplatin |
Response < 20% TTP 2.1 months |
|
Phase II NCT00463788 [313] |
TNBC MBC Prior chemotherapy treatment |
Cetuximab + cisplatin vs. cisplatin alone |
ORR 20% vs. 10% (p = 0.11) PFS 3.7 months vs. 1.7 months (HR 0.67; p = 0.032) OS 12.9 months vs. 9.4 months (HR 0.82; p = 0.31) |
||
|
mTORC1 inhibitors |
Everolimus |
Phase II NCT00930930 [314] |
TNBC Stage II or III Neoadjuvant treatment |
Everolimus + cisplatin and paclitaxel vs. placebo + cisplatin and paclitaxel |
pCR 36% vs. 49% |
|
Akt inhibitors |
Ipatasertib |
LOTUS Phase II NCT02162719 [315] |
TNBC Locally advanced or MBC No prior sytemic therapy |
Ipatasertib + paclitaxel vs. placebo + paclitaxel |
PFS 6.2 months vs. 4.9 months (HR 0.60; p = 0.037) PFS 6.2 months vs. 3.7 moths (HR 0.58; p = 0.18) in PTEN-low patients |
|
FAIRLANE Phase II NCT02301988 [316] |
Early TNBC Neoadjuvant treatment |
Ipatasertib + paclitaxel vs. placebo + paclitaxel |
pCR 17% vs. 13% pCR 16% vs. 13% PTEN-low patients pCR 18% vs. 12% PIK3CA/AKT1/PTEN-altered patients |
||
|
Capivasertib |
PAKT Phase II NCT02423603 [317] |
TNBC MBC No prior chemotherapy treatment |
Capivasertib + paclitaxel vs. placebo + paclitaxel |
PFS 5.9 months vs. 12.6 months (HR 0.61; p = 0.04) |
|
|
Androgen receptor inhibitors |
Bicalutamide |
Phase II NCT00468715 [318] |
HR- AR+ or AR- MBC |
Bicalutamide monotherapy |
CBR 19% PFS 12 weeks |
|
Enzalutamide |
Phase II NCT01889238 [319] |
TNBC AR+ Locally advanced or MBC |
Enzalutamide monotherapy |
CBR 25% OS 12.7 months |
|
|
CYP17 inhibitors |
Abiraterone acetate |
UCBG 12-1 Phase II NCT01842321 [320] |
TNBC AR+ Locally advanced or MBC Centrally reviewed Prior chemotherapy |
Abiraterone acetate + prednisone |
CBR 20% ORR 6.7% PFS 2.8 months |
|
Anti-PDL1 antibodies |
Atezolizumab |
Impassion 130 Phase III NCT02425891 [321] |
TNBC Locally advanced or MBC No prior treatment |
Atezolizumab + nab-paclitaxel vs. placebo + nab-paclitaxel |
OS 21.0 months vs. 18.7 months (HR 0.86; p = 0.078) OS 25.0 months vs. 18.0 months (HR 0.71, 95% CI 0.54–0.94)) in PDL-1+ patients |
|
Impassion 031 Phase III NCT03197935 [322] |
TNBC Stage II to III No prior treatment |
Atezolizumab + chemotherapy vs. placebo + chemotherapy |
pCR 95% vs. 69% p = 0.0044 |
||
|
Durvalumab |
GeparNuevo Phase II NCT02685059 [323] |
TNBC MBC Stromal tumor-infiltrating lymphocyte (sTILs) |
Durvalumab vs. placebo |
pCR 53.4% vs. 44.2% pCR 61.0% vs. 41.4% in window cohort |
|
|
SAFIRO BREAST-IMMUNO Phase II NCT02299999 [324] |
HER2- MBC Prior chemotherapy |
Durvalumab vs. maintenance chemotherapy |
HR of death 0.37 for PDL-1+ patients HR of death 0.49 for PDL-1- patients |
||
|
Phase I NCT02484404 [325] |
Recurrent women’s cancers including TNBC |
Durvalumab + cediranib + olaparib |
Partial response 44% CBR 67% |
||
|
Avelumab |
JAVELIN Phase Ib NCT01772004 [326] |
MBC Prior standard-of-care therapy |
Avelumab monotherapy |
ORR 3.0% overall ORR 5.2% in TNBC ORR 16.7% in PDL-1+ vs. 1.6% in PDL-1- overall ORR 22.2.% in PDL-1+ vs. 2.6% in PDL-1- in TNBC |
|
|
Anti-PD1 antibodies |
Pembrolizumab |
KEYNOTE-086 Phase II NCT02447003 [327] |
TNBC MBC Prior or no prior systemic therapy |
Pembrolizumab monotherapy |
Previously treated patients: ORR 5.3% overall ORR 5.7% PDL-1+ patients PFS 2.0 months OS 9.0 months Non-previously pretreated: ORR 21.4% PFS 2.1 months OS 18.0 months |
|
KEYNOTE-119 Phase III NCT02555657 [328] |
TNBC MBC Prior systemic therapy |
Pembrolizumab vs. chemotherapy |
OS 12.7 months vs. 11.6 months (HR 0.78; p = 0.057) in PDL1+ patients OS 9.9 months vs. 10.8 months (HR 0.97, 95% CI 0.81–1.15) |
||
|
KEYNOTE-355 Phase III NCT02819518 [329] |
TNBC MBC No prior systemic therapy |
Pembrolizumab + chemotherapy vs. placebo + chemotherapy |
PFS 9.7 months vs. 5.6 months (HR 0.65; p = 0.0012) in PDL-1+ patients PFS 7.6 months vs. 5.6 months (HR 0.74; p = 0.0014) |
||
|
KEYNOTE-522 Phase III NCT03036488 [330] |
Early TNBC Stage II to III No prior treatment |
Pembrolizumab + paclitaxel and carboplatin vs. placebo + paclitaxel and carboplatin |
pCR 64.8% vs. 51.2 % (p < 0.001) |
||
|
Anti-CDL4 antibodies |
Tremelimumab |
Phase I [331] |
Incurable MBC |
Tremelimumab + radiotherapy |
OS 50.8 months |
|
Vaccines |
PPV |
Phase II UMIN000001844 [332] |
TNBC MBC Prior systemic therapy |
PPV vaccine |
PFS 7.5 months OS 11.1 months |
|
STn-KLH |
Phase III NCT00003638 [333] |
MBC Prior chemotherapy Partial or complete response |
STn-KLH vaccine vs. non-vaccine |
TTP 3.4 months vs. 3.0 months |
TNBC: triple negative breast cancer; HER2: human epidermal growth factor receptor; HR: hormonal receptor; MBC: metastatic breast cancer; BC: breast cancer; AR: androgen receptor; PPV: personalized peptide vaccine; PFS: progression free survival; CBR: clinical benefit rate; ORR: objective response rate; IDFS: invasive disease-free survival; OS: overall survival; TTP: time to progression; pCR: pathologic complete response; HR: hazard ratio.
This entry is adapted from the peer-reviewed paper 10.3390/jpm11080808
