Anemia is a common condition in preoperative period of peripheral arterial disease patients. Anemia has multifactorial causes, including: iron deficiency; vitamin deficiency and inflammation; and chronic kidney disease.
Some retrospective researches demonstrated, that preprocedural anemia is a predictor adverse outcomes in patients undergoing percutaneous transluminal angioplasty for vascular disease treatment. These outcomes are increase likelihood of: A) transfusion; B) amputation; C) and major adverse cardiovascular events.
It is not clear if preoperative anemia optimization with iron and/or erythropoietin, reduce major adverse outcomes in patients submitted to vascular peripheral surgeries.
- preoperative anemia
- peripheral vascular interventions
- anesthesia
- vascular surgery
- blood transfusion
1. Introduction
Anemia is a frequent condition among patients undergoing surgery for peripheral arterial disease (PAD) [1]. The World Health Organization defines anemia as a hemoglobin (Hb) level < 13 g/dL in men and <12 g/dL in women [2]. Anemia has multifactorial causes, including iron deficiency, vitamin deficiency, inflammation, and chronic kidney disease [3]. There is an association between preoperative anemia and adverse clinical outcomes, such as prolonged hospital length of stay and death [4][5]. However, preoperative anemia is frequently unrecognized as a risk factor and, therefore, not corrected before surgical procedures, particularly those associated with major bleeding.
Peripheral arterial disease has been reported to affect more than 200 million individuals worldwide [6], and perioperative data from these patients have demonstrated anemia prevalence rates ranging from 47 to 75% [1][2][3].
Patients with symptomatic PAD and critical limb ischemia (CLI) have an increased risk of death and cardiovascular events. Advances in medical, surgical, and endovascular techniques have improved these patients’ outcomes; however, an optimal management paradigm has not been established [7]. A large retrospective study demonstrated that anemia’s prevalence is high among patients undergoing percutaneous peripheral vascular intervention (PVI) and is associated with a significantly greater likelihood of amputation, adverse events, and major cardiovascular complications [8].
Patient Blood Management (PBM) program is a patient-centered interdisciplinary with the timely application of evidence-based medical and surgical concepts designed to maintain hemoglobin concentration, optimize hemostasis and minimize blood loss [9]. Strategies to improve anemia, such as PBM programs, are associated to improved outcomes in various surgical settings [9]. It remains to be determined whether the preoperative clinical optimization of anemic patients can decrease post-PVI adverse events [8][10].
2. Pre-Operative Anemia Optimization
Preoperative anemia is a risk predictor of perioperative transfusion of allogeneic blood products, which carries a significant risk of adverse events and mortality [11][12]. In critically ill and surgical patients, transfusion of a single unit of packed [11][12] red blood cells increased the multivariate risk of mortality, wound problems, pulmonary complications, postoperative renal dysfunction, systemic sepsis, composite morbidity, and prolonged postoperative LoS compared to propensity-matched patients who did not receive intraoperative ABT (Figure 1). Data from an observational cohort of total hip arthroplasties showed that ABT was independently associated with an extended length of hospital stay, increased costs, and worse surgical and medical outcomes without affecting the in-hospital mortality rate. Moreover, the adverse effects of blood loss, ABT, and preoperative anemia are synergistic [5]. Orthopedic patients, similarly to vascular disease patients, are, to a great extent, a frail population.
The European Society of Anaesthesiology recommends that patients at risk of bleeding should be assessed for anemia 3–8 weeks before surgery. Although it is possible to investigate and address anemia preoperatively, it should be noted that many surgical patients require urgent intervention. Therefore, the time available for the assessment and correction of anemia is limited at times [11][12]. Anemia prevalence due to iron or vitamin deficiency among patients with critical limb ischemia is high. Therefore, we recommend a systematic approach in preoperative management to measure biomarkers of iron deficiencies, such as ferritin, transferrin saturation, iron, iron-binding capacity, vitamin B12, and folate. The cause of anemia should be assessed and treated before the intervention, and therefore, blood transfusion might be minimized [13][14]. Advances in pharmaceutical technologies results newer iron formulations, which in turn decrease problems inherent with traditional approaches [15]. New oral preparations as effective as standard ferrous sulfate, but better tolerated, are in active research. In other hand, new preparations have entered the clinical scenario, which can be collectively named as “third generation” IV iron compounds. These preparations share common technical features conferring superiority over the older products, allowing giving the total replacement dose (usually 1-1.5 g) in just one or two infusions [15].
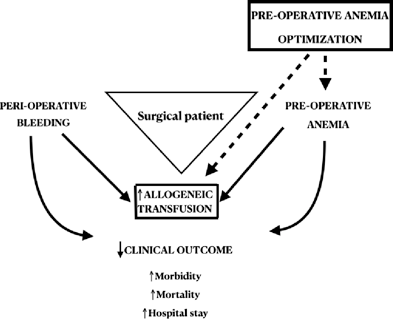
Figure 1. Effects of anemia, bleeding, and allogeneic transfusion on clinical outcomes in patients undergoing major surgery. Preoperative anemia optimization may have positive effects (dashed line). Adapted from Muñoz et al. [2].
3. Conclusions
Screening and clinical evaluation of anemia should be considered a key objective in patients with peripheral arterial vascular disease during the preoperative period. Preoperative anemia, blood transfusion requirement, and adverse outcomes have a strong association in this setting. There is a scarcity of data regarding anemia correction and outcome in patients submitted to lower limb revascularization. Thus, large multicenter randomized controlled trials are necessary to provide consistent evidence about anemia correction in patients with peripheral vascular disease submitted to percutaneous vascular interventions.
References
- Esteban, C.; Rodríguez, P.; Escudero, J.R.; Clarà, A.; Fernández, A.; Fernández, S.; Agúndez, I. Anaemia in patients who underwent vascular surgery: A significant predictor of amputation and death. Clín. 2019, 152, 6–12.
- Muñoz, M.; Acheson, A.G.; Auerbach, M.; Besser, M.; Habler, O.; Kehlet, H.; Liumbruno, G.M.; Lasocki, S.; Meybohm, P.; Baikady, R.R.; et al. International consensus statement on the peri-operative management of anaemia and iron deficiency. Anaesthesia 2016, 72, 233–247.
- Desormais, I.; Aboyans, V.; Bura, A.; Constans, J.; Cambou, J.-P.; Messas, E.; Labrunie, A.; Lacroix, P. Anemia, an Independent Predictive Factor for Amputation and Mortality in Patients Hospitalized for Peripheral Artery Disease. J. Vasc. Endovasc. Surg. 2014, 48, 202–207.
- Leal-Noval, S.R.; Muñoz-Gómez, M.; Jiménez-Sánchez, M.; Cayuela, A.; Leal-Romero, M.; Puppo-Moreno, A.; Enamorado, J.; Arellano-Orden, V. Red blood cell transfusion in non-bleeding critically ill patients with moderate anemia: Is there a benefit? Intensive Care Med. 2013, 39, 445–453.
- Muñoz, M.; Gómez-Ramírez, S.; Campos, A.; Ruiz, J.; Liumbruno, G.M. Pre-operative anaemia: Prevalence, consequences and approaches to management. Blood Transfus. 2015, 13, 370–379.
- Klein, A.J.; Ross, C.B. Endovascular treatment of lower extremity peripheral arterial disease. Trends Cardiovasc. Med. 2016, 26, 495–512.
- Dua, A.; Lee, C.J. Epidemiology of Peripheral Arterial Disease and Critical Limb Ischemia. Vasc. Interv. Radiol. 2016, 19, 91–95.
- Ambulgekar, N.V.; Grey, S.F.; Rosman, H.S.; Othman, H.; Davis, T.P.; Nypaver, T.J.; Schreiber, T.; Yamasaki, H.; Lalonde, T.; Henke, P.K.; et al. Association of Anemia with Outcomes in Patients Undergoing Percutaneous Peripheral Vascular Intervention: Insights From the Blue Cross Blue Shield of Michigan Cardiovascular Consortium (BMC2 VIC). Invasive Cardiol. 2018, 30, 35–42.
- Althoff, F.C.; Neb, H.; Herrmann, E.; Trentino, K.M.; Vernich, L.; Füllenbach, C.; Freedman, J.; Waters, J.H.; Farmer, S.; Leahy, M.F.; et al. Multimodal Patient Blood Management Program Based on a Three-pillar Strategy: A Systematic Review and Me-ta-analysis. Surg. 2019, 269, 794–804.
- Toor, I.S.; Jaumdally, R.J.; Moss, M.S.; Babu, S.B. Preprocedural hemoglobin predicts outcome in peripheral vascular disease patients undergoing percutaneous transluminal angioplasty. J. Vasc. Surg. 2009, 50, 317–321.
- Kozek-Langenecker, S.A.; Ahmed, A.B.; Afshari, A.; Albaladejo, P.; Aldecoa, C.; Barauskas, G.; De Robertis, E.; Faraoni, D.; Filipescu, D.C.; Fries, D.; et al. Management of severe perioperative bleeding: Guidelines from the European Society of Anaesthesiology: First update 2016. J. Anaesthesiol. 2017, 34, 332–395.
- Oshin, O.A.; Torella, F. Low Hemoglobin Concentration Is Associated with Poor Outcome After Peripheral Arterial Surgery. Endovasc. Surg. 2013, 47, 449–453.
- Burton, B.; A’Court, A.M.; Brovman, E.Y.; Scott, M.J.; Urman, R.D.; Gabriel, R.A. Optimizing Preoperative Anemia to Improve Patient Outcomes. Clin. 2018, 36, 701–713.
- De Céniga, M.V.; Bravo, E.; Izagirre, M.; Casco, C.; Estallo, L.; Esteban, M.; Barba, A. Anaemia, Iron and Vitamin Deficits in Patients with Peripheral Arterial Disease. J. Vasc. Endovasc. Surg. 2011, 41, 828–830.
- Girelli, D.; Ugolini, S.; Busti, F.; Marchi, G.; Castagna, A. Modern iron replacement therapy: Clinical and pathophysiological insights. J. Hematol. 2017, 107, 16–30.
