Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Pediatrics
|
Health Policy & Services
Home-based records are paper or electronic records retained and used by mothers or caregivers to document the health services received for maternal, newborn, and child health. Little has been studied about the roles of these records on newborn and child health outcomes.
- home-based records
- MCH handbook
- newborn health
- child health
1. Introduction
Home-based records have been used in over 163 countries worldwide to improve maternal, newborn, and child health (MNCH) [1]. The records varied greatly in design and content across countries and regions. Home-based records are paper or electronic health records retained and used by mothers or caregivers in the household to document the health services received for MNCH [1]. They ranged from maternity case notes or vaccination-only cards to child health books or integrated maternal and child health handbooks. The record is intended to be integrated into the routine health information system and complement records maintained by health facilities [1].
Traditionally, MNCH programs have developed their own program-specific, home-based records. In many countries, the maternal health card continues to be a stand-alone record independent from child records [2]. The difference in target groups has prompted policy debates on whether home-based records should be developed and distributed separately for the mother and child [2]. The lack of integration and having no standardized format and design of home-based records might impact health reporting, health outcomes, scaling up, and evaluation between health systems worldwide [3].
The first integrated home-based record was made in Japan in 1948. The Ministry of Health, Labor and Welfare of Japan introduced the Maternal and Child Health (MCH) handbook to improve the health of both mothers and children [4]. The initial MCH handbook covered the entire spectrum of pregnancy, childbirth, postpartum, and newborn care, through childhood until six years old. In 1991, municipalities and towns/villages in Japan started distributing the MCH handbook following decentralization [4]. Local governments could add more information from the national version (consisted of 48 pages) based on their local needs [4]. Due to Japan’s success in reducing its infant mortality rate, the MCH handbook was adapted worldwide. To date, more than 50 countries used the integrated MCH handbook [4] and is particularly useful when access to health services is restricted [5].
The full integration has several advantages. It includes greater assurance of a continuum of MCH care [6][7][8][9] and sizable cost savings in the record’s operation (e.g., production and distribution) [10]. Healthcare providers can enter medical records into the handbooks and share their knowledge and information on maternal health and child growth [4]. Furthermore, parents can obtain appropriate information easily and rely on the continuous guidance of the handbook from pregnancy to childhood [4]. The MCH handbook can be a valuable tool for promoting a life-course approach to healthcare. Such an approach might help achieve Sustainable Development Goal (SDG) 3—to “ensure healthy lives and promote well-being for all at all ages” [11].
Despite substantial progress over the past two decades, in 2019 alone, the World Health Organization (WHO) reported that approximately 7.4 million children, adolescents, and youth mainly died from preventable or treatable causes [12]. Of these deaths, children under five account for 5.2 million, and the leading causes of their death include preterm birth complications, pneumonia, neonatal sepsis, diarrhea, and malaria [13]. These deaths can be prevented or treated with access to affordable and straightforward interventions, such as immunization, adequate nutrition, safe water, and quality care by a trained healthcare provider [13]. While proven and cost-effective interventions are available to reduce deaths for children under five [14][15][16][17][18], review studies that explored the roles of home-based records in promoting healthcare service delivery among this population are limited.
One study systematically reviewed the effectiveness of home-based records on MNCH [3], which was used as a basis for the WHO’s recommendations concerning home-based records. However, this review article did not comprehensively examine the roles of home-based records on newborn and child health. As defined in the WHO guideline [1], newborn and child health outcomes include newborn/child morbidity and mortality, care seeking, care practices, and health services utilization. Magwood et al. [3] included only two studies for newborn health and seven studies for child health outcomes. They reported no significant effects on newborn health outcomes (e.g., neonatal death or stillbirths, immediate breastfeeding). For child health outcomes, they reported that home-based records might positively impact immunization rates, growth, and development. However, they covered only original research articles with randomized controlled study designs and that were written in English. They might have missed valuable information derived from observational studies. Observational studies may provide more evidence on the roles of home-based records on newborn and child health. They provide information on actual adherence to home-based records, bringing evidence on real-life outcomes of records. In addition, since Japan is a proponent of the MCH handbook, it would be worthy of including Japanese articles in the analysis. By doing so, we could capture more evidence on the roles of home-based records on newborn and child health.
2. Characteristics of Included Studies
Of the 55 studies included in this review, there were 10 RCTs, four cohort studies, seven quasi-experimental (open, nonrandomized trial), 27 cross-sectional, five mixed-methods (pre-and post-intervention with qualitative component), and two qualitative studies. We used the World Bank income level classification to categorize the countries where the study was conducted [19]. Thirty-four studies were conducted in high-income countries (HIC): United Kingdom (n = 3), United States (n = 5), Australia (n = 3), Norway (n = 1), and Japan (n = 22). Twenty-one studies were conducted in low- and middle-income countries (LMIC): Indonesia (n = 3), Kenya (n = 3), Mongolia (n = 2), Pakistan (n = 2), and one study in Vietnam, South Africa, Brazil, Bangladesh, Palestine, Burundi, Uganda, Dominican Republic, Cambodia, Bosnia and Herzegovina, and one multi-country study.
We noted differences in the inclusion criteria of the study populations. Mothers’ enrollment period varied across the studies, from any time during pregnancy, childbirth, and the postpartum period. One study was conducted in 13 centers in eight countries and targeted both literate and illiterate mothers living in different geographical and cultural conditions and communities with low or easy access to health services [20]. In this review, most studies were conducted in health facilities, and a few were conducted in community settings.
We also noted differences in the type of interventions. Of 55 studies, 34 focused on the MCH handbook, and the remaining 21 focused on other home-based records, such as maternity case notes, road to health (RTH) booklet, personal child health record, among others. Some studies did not have a comparison group, while others were compared to standard care or non-users of home-based records. Hence, the results were reported considering home-based records as a single intervention. Overall, the studies were heterogeneous, and the sample sizes mainly varied (range: 5–5,940,204).
3. Risk of Bias in Included Studies
We noted differences in the risk of bias across the studies. Figure 2 shows the risk of bias assessment for the 10 RCTs included in this review [21]. Following the RoB 2 algorithm, all selected studies had a high overall risk of bias, mainly owing to bias from the randomization process, blinding/masking not described or not possible for the said intervention, and selective outcome reporting. We found some methodological considerations and critical potential confounding variables neither measured nor adjusted statistically.
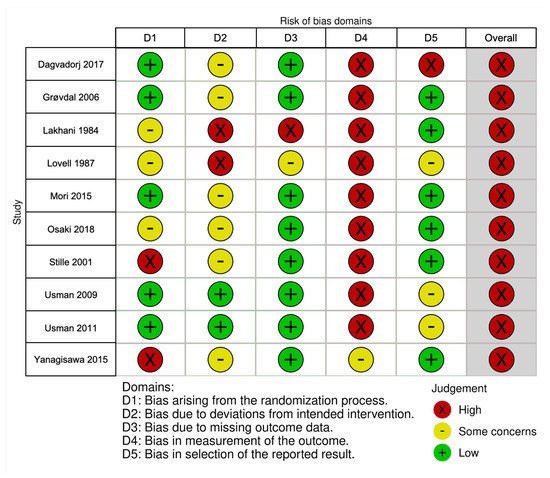
Figure 2. Risk of bias summary for randomized controlled trials based on authors’ judgments (low, some concerns, high) about each risk of bias item for each included study.
4. Roles of Home-Based Records on Newborn Health
Eight studies assessed the roles of home-based records on newborn health [6][7][20][22][23][24][25][26] (Table 1). Findings suggested a positive effect of home-based records on newborn care seeking (n = 2) and newborn care knowledge (n = 2). In Burundi, the proportion of mothers who sought postnatal care (PNC) from health personnel after delivery significantly increased from 35.9% to 64.2% after using the MCH handbook (p < 0.05, 95% CI: 59.2–69.3%) [22]. In South Africa, the proportion of HIV PCR birth tests registered with the RTH booklet identifier reached > 50% after only six months, suggesting that the RTH booklet can successfully be leveraged to provide infants with a unique patient identifier at birth [23]. In Indonesia, the mother class used the MCH handbook as the main reference material during the educational sessions [24]. Attending mothers showed improvement in knowledge regarding immediate breastfeeding (OR = 2.79, 95% CI: 1.48–5.25), giving colostrum (OR = 2.09, 95% CI: 1.09–4.02), exclusive breastfeeding duration (OR = 3.54, 95% CI: 2.04–6.15), use of antibiotic for newborn’s eyes (OR = 4.58, 95% CI: 3.05–6.88), hepatitis B immunization at birth (OR = 1.56; 95% CI: 1.06–2.28), thermal protection (OR = 3.99, 95% CI: 1.59–10.06), cord care (OR = 8.86, 95% CI: 5.69–13.8), and recognition of danger signs in newborns (OR = 3.29, 95% CI: 2.15–5.05) [24]. Indonesian mothers who used the MCH handbook were more likely to practice good newborn care than the standard care group (OR = 1.81, 95% CI: 1.24–2.66) [24]. Similarly, a multi-country study showed that mothers who used home-based maternal records became more involved in looking after their health and newborns [20].
Table 1. Roles of the MCH handbook and other home-based records on newborn health.
| Outcome | Intervention | No Effect, (n) | Mixed Effect, (n) | Positive Effect, n (%) |
Total Times Outcome Reported, (n) |
|---|---|---|---|---|---|
| Newborn care seeking | |||||
| Care seeking for newborn complications [6] | MCH handbook | 1 | 0 | 0 (0) | 1 |
| Care seeking after delivery [22] | MCH handbook | 0 | 0 | 1 (100) | 1 |
| Use of laboratory services [23] | RTH booklet | 0 | 0 | 1 (100) | 1 |
| Total (newborn care seeking) | 1 | 0 | 2 (67) | 3 | |
| Newborn care knowledge | |||||
| Immediate breastfeeding [24][25] | MCH handbook | 0 | 0 | 2 (100) | 2 |
| Giving colostrum [24] | MCH handbook | 0 | 0 | 1 (100) | 1 |
| Exclusive breastfeeding Duration [24] |
MCH handbook | 0 | 0 | 1 (100) | 1 |
| Use of antibiotic for eyes [24] | MCH handbook | 0 | 0 | 1 (100) | 1 |
| Hepatitis B immunization at birth [24] |
MCH handbook | 0 | 0 | 1 (100) | 1 |
| Thermal protection [24] | MCH handbook | 0 | 0 | 1 (100) | 1 |
| Cord care [24] | MCH handbook | 0 | 0 | 1 (100) | 1 |
| Recognize the danger signs in newborns [24] | MCH handbook | 0 | 0 | 1 (100) | 1 |
| Total (newborn care knowledge) | 0 | 0 | 9 (100) | 9 | |
| Newborn care practices | |||||
| Immediate breastfeeding [7][26] | MCH handbook; maternity case notes | 2 | 0 | 0 (0) | 2 |
| Good newborn care and self-care [20][24] |
MCH handbook; home-based maternal record | 0 | 0 | 2 (100) | 2 |
| Total (newborn care practices) | 2 | 0 | 2 (50) | 4 | |
| Perinatal mortality and morbidity | |||||
| Neonatal deaths [7][26] | MCH handbook; maternity case notes | 2 | 0 | 0 (0) | 2 |
| APGAR score [7] | MCH handbook | 1 | 0 | 0 (0) | 1 |
| Total (perinatal mortality and morbidity) | 3 | 0 | 0 (0) | 3 |
MCH—maternal and child health, APGAR—appearance, pulse, grimace, activity, and respiration, RTH—road to health.
However, findings suggest no significant effects of home-based records on immediate breastfeeding (n = 2), neonatal deaths (n = 2), or APGAR (i.e., appearance, pulse, grimace, activity, and respiration) score (n = 1). One RCT conducted in the UK showed no significant difference between mothers in the case note group and cooperation card group about breastfeeding after delivery (78.9% vs. 77.4%, respectively) and the incidence of neonatal deaths (both 2.0%, GRADE certainty of evidence: very low) [26]. The same results were obtained in one cluster RCT conducted in Mongolia [7]. A higher rate of immediate breastfeeding initiation was observed among mothers who received the MCH handbook (versus no handbook); however, there was no significant difference (RR = 1.07, 95% CI: 0.97–1.18, GRADE certainty of evidence: moderate) [7]. Moreover, there was no significant difference in either neonatal deaths (RR = 1.00, 95% CI: 0.99–1.02, GRADE certainty of evidence: very low) or APGAR scores (MD = 0.21, 95% CI: −0.21–0.63, GRADE certainty of evidence: moderate) using the MCH handbook compared with the control group [7].
5. Roles of Home-Based Records on Child Health
We found evidence on the positive effects of home-based records on childcare seeking (n = 6) and vaccination uptake and recording (n = 10) (Table 2).
Table 2. Roles of the MCH handbook and other home-based records on child health.
| Outcome | Intervention | No Effect, (n) |
Mixed Effect, (n) | Positive Effect, n (%) |
Total Times Outcome Reported, (n) |
|---|---|---|---|---|---|
| Vaccination use/uptake | |||||
| DTP3 completion [27][28][29][30] | Home-based health record booklet; educational immunization cards; redesigned immunization card | 2 | 0 | 2 (50) | 4 |
| Rotavirus vaccination [31] | MCH handbook | 0 | 1 | 0 (0) | 1 |
| BCG and polio vaccination [32] | MCH handbook | 0 | 1 | 0 (0) | 1 |
| Mumps, measles, chickenpox [33] |
MCH handbook | 0 | 1 | 0 (0) | 1 |
| Total (vaccination use/uptake) | 2 | 3 | 2 (29) | 7 | |
| Vaccination history/records [34][35][36][37][38][39][40][41][42] |
MCH handbook; personal health record; personal child health record and advice booklet; individually tailored calendar; child health card; patient-held vaccination records; personalized calendar | 0 | 1 | 8 (89) | 9 |
| Childcare seeking | |||||
| Care seeking for child Illnesses [6][43][44][45] |
MCH handbook; personal health record; parent-held child health record | 2 | 0 | 2 (50) | 4 |
| Use of healthcare and laboratory Services [45][46][47] |
MCH handbook; parent-held child health record | 1 | 0 | 2 (67) | 3 |
| Adherence to recommended Immunizations [48][49] |
MCH handbook; personal health record | 0 | 0 | 2 (100) | 2 |
| Adherence to childcare visit Recommendations [49] |
Personal health record | 0 | 0 | 1 (100) | 1 |
| Total (childcare seeking) | 3 | 0 | 7 (70) | 10 | |
| Child healthcare knowledge | |||||
| General health [43][45][50] | MCH handbook; personal child health record; parent-held child health record | 2 | 0 | 1 (33) | 3 |
| Immunization [24][48][51][52][53] | MCH handbook | 3 | 1 | 1 (20) | 5 |
| Exclusive breastfeeding [48][54][55] |
MCH handbook | 0 | 0 | 3 (100) | 3 |
| Detection of biliary atresia [56][57][58] |
MCH handbook stool card | 0 | 2 | 1 (33) | 3 |
| Sudden infant death syndrome [59] | MCH handbook | 0 | 1 | 0 (0) | 1 |
| Accident prevention of infant [60] | MCH handbook | 0 | 0 | 1 (100) | 1 |
| Total (child healthcare knowledge) | 5 | 4 | 7 (44) | 16 | |
| Child healthcare practices | |||||
| Exclusive breastfeeding [6][48][55] |
MCH handbook | 1 | 0 | 2 (67) | 3 |
| Continued breastfeeding [6] | MCH handbook | 0 | 0 | 1 (100) | 1 |
| Complementary feeding [6] | MCH handbook | 0 | 0 | 1 (100) | 1 |
| Proper feeding order [6] | MCH handbook | 0 | 0 | 1 (100) | 1 |
| Varied foods feeding [6] | MCH handbook | 0 | 0 | 1 (100) | 1 |
| Complementary feeding [6] | MCH handbook | 0 | 0 | 1 (100) | 1 |
| Proper feeding order [6] | MCH handbook | 0 | 0 | 1 (100) | 1 |
| Varied foods feeding [6] | MCH handbook | 0 | 0 | 1 (100) | 1 |
| Self-feeding training [6] | MCH handbook | 0 | 0 | 1 (100) | 1 |
| Recording immunizations [27][37][61][62][63] |
MCH handbook; home-based health record booklet; child health record; home-based record | 1 | 2 | 2 (40) | 5 |
| Growth monitoring [37][62][64][65][66][67][68][69] |
MCH handbook; child health card; child personal health record; child health handbook; health and living log | 3 | 2 | 4 (44) | 9 |
| Total (child healthcare practices) |
5 | 4 | 13 (59) | 22 | |
| Infant and child illness management | |||||
| Home care for cough [6] | MCH handbook | 0 | 0 | 1 (100) | 1 |
| Home care for diarrhea [6][41] | MCH handbook | 1 | 0 | 1 (50) | 2 |
| Vitamin A use [6][48] | MCH handbook | 0 | 0 | 2 (100) | 2 |
| Total (infant and child illness management) | 1 | 0 | 4 (80) | 5 | |
| Child mortality and morbidity | |||||
| Underweight children [6] | MCH handbook | 0 | 0 | 1 (100) | 1 |
| Stunted growth [6] | MCH handbook | 0 | 0 | 1 (100) | 1 |
| Wasting [6] | MCH handbook | 1 | 0 | 0 (0) | 1 |
| Risk of cognitive delay [70] | MCH handbook | 0 | 0 | 1 (100) | 1 |
| Total (child mortality and morbidity) | 1 | 0 | 3 (75) | 4 | |
| Continuum of care [6][20][22][41][55][71][72][73] |
MCH handbook; home-based maternal record | 0 | 1 | 7 (88) | 8 |
MCH—maternal and child health, DTP3—third dose of diphtheria, tetanus toxoids, and pertussis, BCG—Bacillus Calmette–Guérin.
Mothers who received home-based records were more likely to utilize healthcare services [6][43][44][45][46][47] and adhere to the recommended immunizations and childcare visit recommendations [34][35][36][37][38][39][40][41][42][48][49]. However, a mixed effect was obtained concerning age-appropriate immunization, such as a three-dose series of diphtheria, tetanus toxoids, and pertussis (DTP) [27][28][29][30]. Findings in randomized trials conducted in the UK and USA suggested no significant effects on the DTP3 completion rate among children using home-based records compared to no home-based records (pooled RR = 0.89, 95% CI: 0.64–1.24, GRADE certainty of evidence: very low) [27][28]. In contrast, in an RCT conducted in Pakistan, children who were using a redesigned immunization card showed significant improvement in the DTP3 completion rate compared to a standard expanded program on immunization (EPI) card (pooled RR = 1.46, 95% CI: 1.09–1.94, GRADE certainty of evidence: moderate) [29][30].
Six out of 16 studies showed a positive effect of home-based records on child healthcare knowledge. Mothers who used home-based records showed improvement in their knowledge of general health [43], immunization [48], exclusive breastfeeding [48][54][55], biliary atresia [57], and infant accident prevention [60]. Among less-educated Japanese women who are literate, the MCH handbook effectively provided adequate knowledge about exclusive breastfeeding [54]. Similarly, mothers who had read the MCH handbook were more careful of infant accidents than a group of mothers who had never read the handbook (p < 0.01) [60]. On the other hand, a few studies reported no effect/mixed results related to immunization [51][52][53], detection of biliary atresia [56][58], and sudden infant death syndrome [59]. Japanese mothers requested more information on the vaccination schedule, stool color card, and sudden infant death syndrome.
Most studies reported an improvement in child health practices (n = 8) and illness management (n = 3) among recipients of home-based records. A significant change in exclusive breastfeeding practice was seen among mothers who received the MCH handbook in Bangladesh (16.9% vs. 0.7%) and Vietnam (74.9% vs. 18.3%) [48][55]. However, one RCT conducted in Indonesia showed no effect of the MCH handbook on exclusive breastfeeding for six months (OR = 0.76, 95% CI: 0.51–1.14, GRADE certainty of evidence: low) [6]. Despite this opposite result, the authors reported that Indonesian mothers who received the MCH handbook tended to practice continued breastfeeding (OR = 2.31, 95% CI: 1.22–4.39), complementary feeding (OR = 4.35, 95% CI: 2.85–6.65), proper feeding order (OR = 2.70, 95% CI: 1.79–4.09), varied foods feeding, e.g., by providing fruits and/or fruits extract (OR = 2.18, 95% CI: 1.42–3.36), and self-feeding training (OR = 2.75, 95% CI: 1.74–4.36) [6] (GRADE certainty of evidence: moderate). In a similar study, mothers who received the MCH handbook tended to practice home care for cough (OR = 3.50, 95% CI: 1.44–8.52, GRADE certainty of evidence: low) and vitamin A use (OR = 2.00, 95% CI: 1.16–3.47, GRADE certainty of evidence: moderate) [6]. The study did not show a significant difference between the intervention and control arm for home care for diarrhea (83.3% of 24 cases, 92.6% of 27 cases) [6]. In contrast, growth monitoring seemed to concern mothers who received a home-based record. Mothers ignored developmental indicators that they did not understand, such as head circumference [64] and growth curves (e.g., weight-versus-age chart, BMI-versus-age chart) [65][67]. Further explanation may have supported mothers to address this issue. In Japan, reading and completing the MCH handbook were associated with maternal characteristics, with older mothers and mothers with little childcare experience completing the handbook more [66].
Two randomized studies showed evidence related to child mortality and morbidity [6][70]. In Indonesia, mothers who received the MCH handbook were less likely to have underweight children (OR = 0.33, 95% CI: 0.12–0.94, GRADE certainty of evidence: very low) and children with stunted growth (OR = 0.53, 95% CI: 0.30–0.92, GRADE certainty of evidence: low) [6]. However, no significant difference was observed between the intervention and control arm concerning wasting among children [6]. In Mongolia, MCH handbook users showed a reduction in the risk of children’s cognitive delay compared with the control group at a three-year follow-up (AOR = 0.32, 95% CI: 0.14–0.73, GRADE certainty of evidence: very low) [70].
Seven out of eight studies showed a positive effect of home-based records on the continuum of care [6][20][22][41][55][71][72]. Among all home-based records, the MCH handbook showed evidence of the continuum of maternal, newborn, and childcare. In Vietnam, the proportion of pregnant women who made ≥ 3 antenatal care (ANC) visits and practiced exclusive breastfeeding significantly increased between pre- and post-intervention (p < 0.001) [55]. In Burundi, the proportion of mothers who received birth notification at health facilities significantly increased from 4.6% to 61.0% (p < 0.05, 95% CI: 55.9–66.2%) [22]. In the Dominican Republic, the rate of mothers receiving antenatal and postpartum care at designated clinics or hospitals increased from 13% to 40% [41]. In Japan, mothers who had seen their own MCH handbook when they were young had a higher continuity awareness than those who had not [72]. The MCH handbook also strengthened the collaborative interactions among hospitals, local government units, and schools [73]. However, more effort is needed to translate the positive utilization of the MCH handbook into personal responsibility for health [73].
This entry is adapted from the peer-reviewed paper 10.3390/ijerph18147463
References
- World Health Organization. WHO Recommendations on Home-Based Records for Maternal, Newborn and Child Health. Available online: (accessed on 21 May 2021).
- Osaki, K.; Aiga, H. Adapting home-based records for maternal and child health to users’ capacities. Bull. World Health Organ. 2019, 97, 296–305.
- Magwood, O.; Kpadé, V.; Thavorn, K.; Oliver, S.; Mayhew, A.D.; Pottie, K. Effectiveness of home-based records on maternal, newborn and child health outcomes: A systematic review and meta-analysis. PLoS ONE 2019, 14, e0209278.
- Nakamura, Y. The role of maternal and child health (MCH) handbook in the era of sustainable development goals (SDGs). J. Glob. Health Sci. 2019, 1, 1–7.
- Osaki, K.; Aiga, H. What Is Maternal and Child Health Handbook? Available online: (accessed on 21 May 2021).
- Osaki, K.; Hattori, T.; Toda, A.; Mulati, E.; Hermawan, L.; Pritasari, K.; Bardosono, S.; Kosen, S. Maternal and child health handbook use for maternal and child care: A cluster randomized controlled study in rural Java, Indonesia. J. Public Health 2019, 41, 170–182.
- Mori, R.; Yonemoto, N.; Noma, H.; Ochirbat, T.; Barber, E.; Soyolgerel, G.; Nakamura, Y.; Lkhagvasuren, O. The maternal and child health (MCH) handbook in Mongolia: A cluster-randomized, controlled trial. PLoS ONE 2015, 10, e0119772.
- Isaranurug, S. Maternal and child health handbook in Thailand. Kokusai Hoken Iryo. (J. Int. Health) 2009, 24, 61–66.
- Nakamura, Y. Maternal and child health handbook in Japan. JMAJ 2010, 53, 259–265.
- Aiga, H.; Pham Huy, T.K.; Nguyen, V.D. Cost savings through implementation of an integrated home-based record: A case study in Vietnam. Public Health 2018, 156, 124–131.
- Every Woman Every Child. The Global Strategy for Women’s, Children’s and Adolescents’ Health 2016–2030. Available online: (accessed on 21 May 2021).
- World Health Organization. Maternal, Newborn, Child and Adolescent Health. Available online: (accessed on 21 May 2021).
- World Health Organization. Children: Improving Survival and Well-Being. Available online: (accessed on 21 May 2021).
- Svefors, P.; Selling, K.E.; Shaheen, R.; Khan, A.I.; Persson, L.; Lindholm, L. Cost-effectiveness of prenatal food and micronutrient interventions on under-five mortality and stunting: Analysis of data from the MINIMat randomized trial, Bangladesh. PLoS ONE 2018, 13, e0191260.
- Goudet, S.; Jayaraman, A.; Chanani, S.; Osrin, D.; Devleesschauwer, B.; Bogin, B.; Madise, N.; Griffiths, P. Cost effectiveness of a community based prevention and treatment of acute malnutrition programme in Mumbai slums, India. PLoS ONE 2018, 13, e0205688.
- Pitt, C.; Tawiah, T.; Soremekun, S.; ten Asbroek, A.H.; Manu, A.; Tawiah-Agyemang, C.; Hill, Z.; Owusu-Agyei, S.; Kirkwood, B.R.; Hanson, K. Cost and cost-effectiveness of newborn home visits: Findings from the Newhints cluster-randomised controlled trial in rural Ghana. Lancet Glob. Health. 2016, 4, e45–e56.
- Gowani, S.; Yousafzai, A.K.; Armstrong, R.; Bhutta, Z.A. Cost effectiveness of responsive stimulation and nutrition interventions on early child development outcomes in Pakistan. Ann. N. Y. Acad. Sci. 2014, 1308, 149–161.
- Fischer, T.K.; Anh, D.D.; Antil, L.; Cat, N.D.; Kilgore, P.E.; Thiem, V.D.; Rheingans, R.; Thole, H.; Glass, R.I.; Bresee, J.S. Health care costs of diarrheal disease and estimates of the cost-effectiveness of rotavirus vaccination in Vietnam. J. Infect. Dis. 2005, 192, 1720–1726.
- The World Bank. World Bank Country and Lending Groups. Available online: (accessed on 21 May 2021).
- Shah, P.M.; Selwyn, B.J.; Shah, K.; Kumar, V. Evaluation of the home-based maternal record: A WHO collaborative study. Bull. World Health Organ. 1993, 71, 535–548.
- McGuinness, L.A.; Higgins, J.P.T. Risk-of-bias VISualization (robvis): An R package and shiny web app for visualizing risk-of-bias assessments. Res. Synth. Methods 2021, 12, 55–61.
- Kaneko, K.; Niyonkuru, J.; Juma, N.; Mbonabuca, T.; Osaki, K.; Aoyama, A. Effectiveness of the maternal and child health handbook in Burundi for increasing notification of birth at health facilities and postnatal care uptake. Glob. Health Action 2017, 10, 1297604.
- Haeri Mazanderani, A.; Sherman, G.G.; Moyo, F.; Goga, A.E.; Feucht, U. Leveraging the road to health booklet as a unique patient identifier to monitor the prevention of mother-to-child transmission programme. S. Afr. Med. J. 2018, 108, 729–733.
- Nasir, N.M.; Amran, Y.; Nakamura, Y. Changing knowledge and practices of mothers on newborn care through mother class: An intervention study in Indonesia. J. Trop Pediatr. 2017, 63, 440–446.
- Yanagisawa, S.; Soyano, A.; Igarashi, H.; Ura, M.; Nakamura, Y. Effect of a maternal and child health handbook on maternal knowledge and behaviour: A community-based controlled trial in rural Cambodia. Health Policy Plan. 2015, 30, 1184–1192.
- Lovell, A.; Zander, L.I.; James, C.E.; Foot, S.; Swan, A.V.; Reynolds, A. The St. Thomas’s hospital maternity case notes study: A randomised controlled trial to assess the effects of giving expectant mothers their own maternity case notes. Paediatr Perinat Epidemiol. 1987, 1, 57–66.
- Lakhani, A.D.; Avery, A.; Gordon, A.; Tait, N. Evaluation of a home based health record booklet. Arch. Dis. Child. 1984, 59, 1076–1081.
- Stille, C.J.; Christison-Lagay, J.; Bernstein, B.A.; Dworkin, P.H. A simple provider-based educational intervention to boost infant immunization rates: A controlled trial. Clin. Pediatr. 2001, 40, 365–373.
- Usman, H.R.; Akhtar, S.; Habib, F.; Jehan, I. Redesigned immunization card and center-based education to reduce childhood immunization dropouts in urban Pakistan: A randomized controlled trial. Vaccine 2009, 27, 467–472.
- Usman, H.R.; Rahbar, M.H.; Kristensen, S.; Vermund, S.H.; Kirby, R.S.; Habib, F.; Chamot, E. Randomized controlled trial to improve childhood immunization adherence in rural Pakistan: Redesigned immunization card and maternal education. Trop. Med. Int. Health 2011, 16, 334–342.
- Inoue, M.; Takanashi, S.; Ushijima, H.; Okitsu, S.; Sakiyama, H.; Mizuguchi, M. Cumulative vaccination rate of rotavirus vaccines in Fuchu City, Tokyo [in Japanese]. J. Jpn. Pediatric Soc. 2015, 119, 525–537.
- Yamamoto, Y.; Nakano, C.; Suga, H. Study on caregiver awareness on vaccination- current status of caregiver support and reality after revision of vaccination law [in Japanese]. Bull. Kobe City Jun Coll. Nurs. 1998, 17, 61–66.
- Kimura, M. History of infection and vaccination for varicella and mumps among children and importance of immunization against these infections [in Japanese]. Jpn. J. Pediatric 2010, 63, 1959–1963.
- Jeffs, D.; Nossar, V.; Bailey, F.; Smith, W.; Chey, T. Retention and use of personal health records: A population-based study. J. Paediatr. Child. Health 1994, 30, 248–252.
- McMaster, P.; McMaster, H.J.; Southall, D.P. Personal child health record and advice booklet programme in Tuzla, Bosnia Herzegovina. J. R. Soc. Med. 1996, 89, 202–204.
- Kreuter, M.W.; Caburnay, C.A.; Chen, J.J.; Donlin, M.J. Effectiveness of individually tailored calendars in promoting childhood immunization in urban public health centers. Am. J. Public Health 2004, 94, 122–127.
- Mukanga, D.O.; Kiguli, S. Factors affecting the retention and use of child health cards in a slum community in Kampala, Uganda, 2005. Matern. Child. Health J. 2006, 10, 545–552.
- McElligott, J.T.; Darden, P.M. Are patient-held vaccination records associated with improved vaccination coverage rates? Pediatrics 2010, 125, e467–e472.
- Abbott, P.; Menzies, R.; Davison, J.; Moore, L.; Wang, H. Improving immunisation timeliness in aboriginal children through personalised calendars. BMC Public Health 2013, 13, 598.
- Kanno, T.; Wada, H. Study of vaccination history of children entering elementary school (from 2 school registration in Morioka years S61 and 62) [in Japanese]. Jpn. Med. J. 1988, 3335, 30–34.
- Shimizu, I. Introducing a maternal child health handbook in the province of Dajabón, Dominican Republic: Prospects and issues from the perspectives of sustainability and replicability [in Japanese]. J. Int. Health. 2007, 22, 153–161.
- Ogasawara, T. Issues of MCH handbook utilization during disasters [in Japanese]. Jpn. J. Telemed. Telecare 2016, 12, 102–104.
- Kawakatsu, Y.; Sugishita, T.; Oruenjo, K.; Wakhule, S.; Kibosia, K.; Were, E.; Honda, S. Effectiveness of and factors related to possession of a mother and child health handbook: An analysis using propensity score matching. Health Educ. Res. 2015, 30, 935–946.
- Zhou, Y.Y.; Leith, W.M.; Li, H.; Tom, J.O. Personal health record use for children and health care utilization: Propensity score-matched cohort analysis. J. Am. Med. Inform. Assoc. 2015, 22, 748–754.
- Bjerkeli Grøvdal, L.; Grimsmo, A.; Ivar Lund Nilsen, T. Parent-held child health records do not improve care: A randomized controlled trial in Norway. Scand. J. Prim. Health Care 2006, 24, 186–190.
- Mudany, M.A.; Sirengo, M.; Rutherford, G.W.; Mwangi, M.; Nganga, L.W.; Gichangi, A. Enhancing maternal and child health using a combined mother & child health booklet in Kenya. J. Trop. Pediatr. 2015, 61, 442–447.
- Nakazawa, M.; Takahashi, S.; Sato, T.; Ishikawa, K. The relationship between the result of diagnosis after neonatal hearing screening and the achievement of the hearing development checklist [in Japanese]. Audiol. Jpn. 2007, 50, 113–121.
- Bhuiyan, S.; Nakamura, Y.; Qureshi, N. Study on the development and assessment of maternal and child health (MCH) handbook in Bangladesh. J. Public Health Dev. 2006, 4, 45–59.
- Tom, J.O.; Chen, C.; Zhou, Y.Y. Personal health record use and association with immunizations and well-child care visits recommendations. J. Pediatr. 2014, 164, 112–117.
- Moore, J.; Brindle, A.; Goraya, P.; Monk, S.; Rennie, D.; Tamhne, R.; Watterson, J.; Stretch, D. A personal child health record for children with a disability. Ambulatory Child. Health 2000, 6, 261–267.
- Yahata, H.; Tanaka, T. How to improve the measles vaccination rate? [in Japanese]. J. Jpn. Soc. Health Educ. Health Promot. 2005, 13, 286–287.
- Oguchi, T.; Kumakura, M. Measles and rubella—Vaccine use and strategies for their elimination in “A” prefecture, Japan [in Japanese]. Bull. Dokkyo Med. Univ. School Nurs. 2014, 7, 1–9.
- Kamiya, S.; Kumita, A.; Okamoto, K.; Shimizu, N.; Komatsu, M. Childrearing mother’s state and difficulties faced when gathering vaccination information [in Japanese]. Bull. Aichi Prefect. Coll. Nurs. Health 2016, 22, 37–44.
- Hagiwara, A.; Ueyama, M.; Ramlawi, A.; Sawada, Y. Is the maternal and child health (MCH) handbook effective in improving health-related behavior? Evidence from Palestine. J. Public Health Policy 2013, 34, 31–45.
- Aiga, H.; Nguyen, V.D.; Nguyen, C.D.; Nguyen, T.T.; Nguyen, L.T. Knowledge, attitude and practices: Assessing maternal and child health care handbook intervention in Vietnam. BMC Public Health 2016, 16, 129.
- Yamagiwa, I.; Akiyama, T. The questionnaire survey on the level of knowledge and interest about biliary atresia of pregnant women [in Japanese]. Niigata Seiryo Acad. Soc. 2009, 1, 113–119.
- Hirayama, Y.; Naito, S.; Iinuma, Y.; Hashizume, N.; Iida, H.; Nitta, K. A strategy for the early detection of biliary atresia by appending the stool color card to the maternal and child health handbook [in Japanese]. J. Jpn. Soc. Perinat. Neonat. Med. 2011, 47, 78–81.
- Yokoi, A.; Isono, K. Examination of the usefulness of stool color card in early detection of biliary atresia [in Japanese]. J. Jpn. Soc. Pediatric Surg. 2019, 55, 945–950.
- Ichikawa, M. Arial relationship between mother’s knowledge of the SIDS and a child-rearing source [in Japanese]. Bull. Hokkaido Univ. Sci. 2016, 41, 55–60.
- Nokubo, M.; Okabe, M.; Miyata, S.; Sakurai, S. Mothers’ awareness on the prevention of infant accidents [in Japanese]. Mie Nurs. J. 2006, 8, 75–86.
- Brown, D.W.; Tabu, C.; Sergon, K.; Shendale, S.; Mugoya, I.; Machekanyanga, Z.; Okoth, P.; Onuekwusi, I.U.; Ogbuanu, I.U. Home-based record (HBR) ownership and use of HBR recording fields in selected Kenyan communities: Results from the Kenya missed opportunities for vaccination assessment. PLoS ONE 2018, 13, e0201538.
- Enokido, F.; Iizuka, T. Study on MCH handbook use [in Japanese]. Jpn J. Matern Health. 1965, 6, 18–20.
- Fujimoto, M.; Nakamura, Y.; Ikeda, M.; Takeda, Y.; Higurashi, M. Study on MCH handbook utilization [in Japanese]. Jpn. J. Public Health 2001, 48, 486–494.
- Hamilton, L.; Wyver, S. Parental use and views of the child personal health record. Aust. Educ. Dev. Psychol. 2012, 29, 66–77.
- Araujo, E.M.N.d.; Gouveia, M.T.d.O.; Pedraza, D.F. Use of a child health surveillance instrument focusing on growth. A cross-sectional study. Sao Paulo Med J. 2017, 135, 541–547.
- Hokama, T.; Hamamoto, I.; Oomine, F.; Sakamoto, R.; Takeda, M. Second report on the study of MCH handbook utilization—from the results of a survey of mothers of 3-5 months old children [in Japanese]. Jpn. J. Matern. Health 2000, 41, 336–339.
- Aoki, M.; Kasuya, K.; Fujimaki, W. Attempt to optimize the usage of the maternal and child health handbook using a questionnaire survey of guardians of preschool child [in Japanese]. J. Child. Health 2009, 68, 575–582.
- Shibahara, M. Support for infants with lower limb disability living at home: Creation of a health and living log [in Japanese]. Rigakuryoho Kagaku 2010, 25, 693–697.
- Fujii, M.; Sato, T. Perception regarding maternal and child health handbook of mothers who gave birth to twins [in Japanese]. J. Jpn. Red Cross Soc. Nurs. Sci. 2020, 20, 52–60.
- Dagvadorj, A.; Nakayama, T.; Inoue, E.; Sumya, N.; Mori, R. Cluster randomised controlled trial showed that maternal and child health handbook was effective for child cognitive development in Mongolia. Acta Paediatr. 2017, 106, 1360–1361.
- Osaki, K.; Hattori, T.; Kosen, S. The role of home-based records in the establishment of a continuum of care for mothers, newborns, and children in Indonesia. Glob. Health Action 2013, 6, 1–12.
- Yuge, M.; Kawasaki, K.; Maruyama, Y.; Kinjo, H. The utility and its factor of the maternal and child health handbook—Survey on mothers’ consciousness with 4 months, 18 months, or three-year-old children [in Japanese]. Jpn. J. Health Sci. Res. 2010, 4, 65–72.
- Adachi, M.; Hori, H.; Komada, Y. Evaluation of the usefulness of the maternal and child health handbook in continuous care developed in the Kinan area of Mie Prefecture [in Japanese]. J. Child Health 2010, 69, 325–328.
This entry is offline, you can click here to edit this entry!
