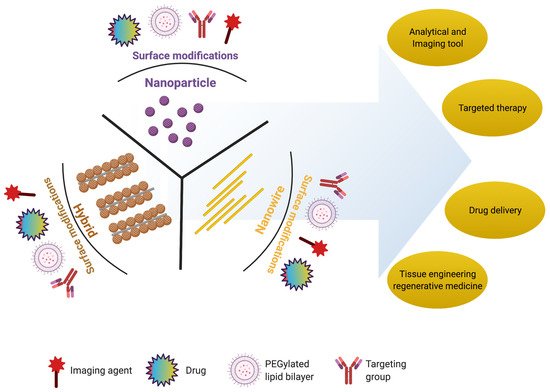
Nanoscience and nanotechnology have revolutionized key areas of environmental sciences, including biological and physical sciences. Nanoscience is useful in interconnecting these sciences to find new hybrid avenues targeted at improving daily life. Pharmaceuticals, regenerative medicine, and stem cell research are among the prominent segments of biological sciences that will be improved by nanostructure innovations. Nanoparticles, nanowires, hybrid nanostructures, and nanoscaffolds, that have been useful in mice for ocular tissue engineering and regeneration.
- nanoparticles
- nanodisks
- scaffolds
- nano-biomaterials and retina
- nanoscaffolds and retinal regeneration
- nanoparticles and retinal regeneration
1. Introduction
2. Nanomaterials for Retinal Regeneration
In the present section, we will discuss the importance of nanoparticles, nanowires, and hybrid nanostructures in retinal regeneration, summarized in Table 1.
| Nanostructure | Nanomaterial | Size Range (nm) | Target Tissue/Cells | Ref. |
|---|---|---|---|---|
| Nanoparticles | Gold (Au) (diameter) |
3–5 | Choroidal and retinal endothelial cells | [42] |
| 10–12 | Retina of rabbit | [43] | ||
| 10–20 | Photoreceptor precursor transplantation | [44] | ||
| 80 | Retinal cells | [45] | ||
| 20–80 | Nucleus and mitochondria of retinal cells | [46] | ||
| 5–20 | Blood–retinal barrier | [44,47,48] | ||
| Gold (Au) nanodisk | Thickness: 20 Diameter: 160 |
Retina | [47] | |
| Silver (Ag) (diameter) |
20–80 | Bovine retinal endothelial cells | [49] | |
| 40–50 | Porcine retinal endothelial cells | [50] | ||
| Superparamagnetic iron oxide nanoparticles | Diameter: 5–20 |
Retina | [51] | |
| Magnetite | 10 | Retina and cells | [52,53] | |
| NWs | Poly (ε-caprolactone) (PCL) membranes | Length: 2500 |
Implantation into subretinal space | [54] |
| Gallium phosphide (GaP) | Length: 500–4000 |
Retinal cells | [55] | |
| n-type silicon | Length: 4400 |
Retinal cells | [56] | |
| Gold (Au) nanorods | Thickness: 10–35 |
Retinal cells and photoreceptors | [57] | |
| Hybrid nanostructure | Gold NPs coated over titania (TiO2) NWs |
Au NP diameter: 5–15 TiO2 NW length: 2000 |
Artificial photoreceptors | [54,58,59,60,61] |
| Gallium phosphide (GaP) rod and cone | Length: 20–2500 |
Ganglion cells, and bipolar cells | [55] | |
| Gold NPs coated over silicon NWs |
Au NP diameter: 5–10 NW length: 500–2500 |
Artificial photoreceptors | [62,63] | |
| Thin film functionalized with the NPs | Diameter: 5–50 |
Photoreceptors | [64,65] | |
| p–n junction silicon NWs | NW length: 10–120 |
Membranes of live bipolar cells | [66] | |
| Au-coated carbon nanotube (Au-CNT) | Au NP diameter: 5–20 CNT length: 500–2500 |
Subretinal space of mice | [67] | |
| Iridium oxide (IrOx) combined with reduced graphene oxide | IrOx diameter: 2–25 CNT length: 2–2500 |
Subretinal implant into live mice | [68] | |
| Iridium oxide (IrOx) coated with CNT | IrOx diameter: 5–25 CNT length: 500–2500 |
Retinal cells/tissues | [52,69,70,71,72] | |
| Core–shell-structured β-NaYF4:20%Yb, 2%Er@β-NaYF4 nanoparticles | Diameter: 30–40 |
Subretinal space of mice | [15] | |
| Nanoscaffolds | Natural polymer: gelatin, fibrin, chitosan, laminin, and hyaluronic acid |
Diameter/porosity: 100–200 |
Extracellular matrix and cell attachment | [73,74,75,76,77,78] |
| Synthetic polymer: poly (lactic-co-glycolic acid) (PLGA), poly (ε-caprolactone) (PCL), poly (L-lactic acid) (PLA), polyimide, and poly (l-lactide-co-ε-caprolactone) |
Diameter/porosity: 50–500 |
RPE, biological activity, extracellular matrix, and cell attachment | [79,80,81,82] | |
| Biohybrid: nanofibers of Bruch’s membrane |
Diameter/porosity: 100–200 |
RPE and biological activity | [83] |
2.1. Nanoparticles
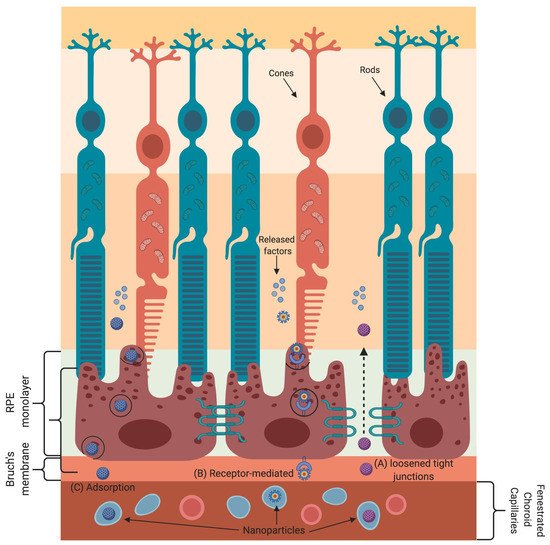
Nanoparticle-based gene and drug delivery to retinal cells has been harnessed to treat various eye diseases [44,84,85,86,87,88,89,90,91]. The various transport mechanisms that nanoparticles employ to cross the blood–retinal barrier are shown in Figure 3. Nanoparticles absorb or scatter light at specific frequencies/wavelengths as a function of their physical and chemical characteristics. These properties of nanoparticles are well suited for bioimaging and to treat cancer by using near-infrared-triggered photothermic therapy (PTT) [92]. Due to the low absorption coefficients of hemoglobin and water, the penetration of near-infrared (650–900 nm) rays in tissues is very high, allowing the use of near-infrared rays for nanoparticle stimulation without damaging the tissue [93]. Gold-nanoparticle-based intravitreal injection is used for retinal imaging and for the inhibition of retinal neovascularization to treat macular degeneration [89,90,91].
2.2. Nanowires
Engineered nanostructural materials are essential for the development of advanced retinal applications. Among them, nanowires have been reported for retinal applications in recent years [59]. It has also been demonstrated that the structure and morphology of nanowires are similar to those of photoreceptors, and the photoabsorption and charge separation properties of nanowires are comparable to those of photodetectors or solar cells [60]. The gold-nanoparticle-decorated titania (Au-TiO2) nanowire acts as an artificial photoreceptor that restores the light responses in a photoreceptor-degenerated retina. The use of nanowires with poly (ε-caprolactone) (PCL) scaffolds for the delivery of retinal progenitor cells resulted in increased differentiation and migration of these cells into both degenerated and normal retinas [54,61]. Nanowires made of gallium phosphide have been shown to support the long-term survival of photoreceptors (rods and cones), ganglion cells, and bipolar cells [55].
2.3. Hybrid Nanostructures
A vast range of nanomaterials and nanostructures have been explored as neural interfaces in retinal physiology; still, no single material has been successful in mimicking the biological, mechanical, and electrical properties of the retina. In recent years, many hybrid approaches have been designed to explore the merits of many materials while at the same time suppressing their demerits. Recently, Tang et al. demonstrated that artificial photoreceptors made of gold-nanoparticle-decorated titania (Au–TiO2) nanowire arrays were able to absorb light, generate photovoltage, and process visual information in a photoreceptor-degenerated retina [14]. Not only is nanowire arrays’ rough morphology useful for their association with cultured neurons, but they are also biocompatible or (photo)chemically stable for over 2 months when used as a subretinal implant in mice [66]. The use of a gold coating on carbon nanotubes (Au-CNTs) further enhanced their surface area and electrical and mechanical adhesion [100]. Iridium oxide–carbon nanotube hybrids (IrOx-CNT) were reported to have a high effective surface area and much higher charge storage capacities compared to pure iridium oxide [67]. Furthermore, the hybrid coatings formed by combining iridium oxide with reduced graphene oxide or graphene oxide exhibited 10% higher charge storage capacities than those of pure iridium oxide and iridium oxide–carbon nanotube hybrids, indicating superior electrochemical stability [52,68,69,70,71].
2.4. Nanoscaffolds
Nanoscaffolds are self-assembled or electrospun nanofibers made up of synthetic or natural polymers. Nanoscaffolds provide a microenvironment for cellular signaling that influences the proliferation, migration, and differentiation of various cells [108].
3. Studies on the Application of Nano-Biomaterials for Retinal Regeneration
| Analysis | Nanomaterial | Form | Size (nm) | Cell Response | Ref. |
|---|---|---|---|---|---|
| In vitro | Poly (ε-caprolactone) (PCL) | NWs | Length: 2500 |
↑ expression of PKC and recoverin in RPCs; cells undergo differentiation | [54] |
| Gallium phosphide (GaP) | NWs | Length: 500–4000 |
Extended growth of retinal cells | [61] | |
| n-type silicon | NWs | Length: 440 |
Long-term and dense growth of mouse retinal cells | [95] | |
| Gold (Au) | Nanoparticle | Diameter: 5–100 |
ARPE-19 cells undergo apoptosis upon AuNP internalization | [77] | |
| Diameter: 10–12 |
Gold nanoparticles inhibit proliferation of ARPE-19 cells; no cytotoxicity | [16] | |||
| Diameter: 80 |
Highly viable mesenchymal stem cells undergo differentiation and secrete various trophic factors | [15] | |||
| Gold (Au), silver (Ag) |
Nanoparticle | Diameter: 20–80 |
Increase uptake into retinal cells; ↑ apoptosis, oxidative stress, and microglia activation | [58] | |
| Gold (Au) | Nanodisk | Diameter: 160 |
Inhibition of in vitro angiogenesis without cellular toxicity of HRMECs | [56] | |
| Hybrid nanoscaffolds |
Combination of Antheraea pernyi silk fibroin (RWSF), PCL, and gelatin |
Diameter/porosity: 90–210 |
Increased expression of RPE marker genes (CRALBP, PEDF, VEGF, MITF, and PMEL 17 among others) |
[83] | |
| In vivo | Poly (ε-caprolactone) (PCL) membranes | NWs | Length: 2500 |
Successful implantation into subretinal space with limited tissue disruption and no inflammation | [54] |
| Gold (Au), titania (TiO2) | Au nanoparticle coated TiO2 NWs | AuNPs diameter: 5–15, TiO2 NW length: 2000 |
AuNP-decorated TiO2 NW arrays restore light-sensitive visual responses in degenerated photoreceptors | [14] | |
| Gold (Au) | Nanodisk | Diameter: 160 | Intravitreal injection attenuates neovascularization in mouse model of oxygen-induced retinopathy | [56] | |
| Gold (Au) | Nanoparticle | Diameter: 20–100 |
Intravitreal injection of gold nanoparticles passed through the blood–retinal barrier with no structural abnormality or cell death | [91] | |
| Gold (Au) | Nano-gold | Not reported | No retinal or optic nerve toxicity by intravitreal injection of nano-gold | [43,91] | |
| Gold (Au), poly (strenesulfate) | Poly (strenesulfate) or anti-CD90.2 antibody-coated Au nanorods (PSS-AuNRs) | Not reported | Intravitreal injection obscured the retinal signal and induced ocular inflammation | [57] | |
| Nanoscaffolds | Nanofibrous porous membrane | Diameter/porosity: 680 | Bruch’s membrane thickness changes with aging, and it correlates with RPE function | [83] | |
| Therapeutic | Gold (Au) | Nanoparticles | Diameter: 20 |
AuNP-labeled photoreceptor precursor transplantation provides high-resolution long-term tracking and cell survival with no toxic effects on retina or cells | [91,117] |
| Core–shell-structured β-NaYF4:20%Yb, 2%Er@β-NaYF4 | Nanoparticle (core–shell-structured upconversion nanoparticles (UCNPs)) |
Diameter: 35–40 |
Retinal pbUCNP injection extends the visual spectrum to the near infra-red range in mice | [15] | |
| Synthetic nanoscaffolds |
Nanofibrous scaffolds | Diameter/porosity: 100–200 |
Used as a cell replacement therapy | [108] |
This entry is adapted from the peer-reviewed paper 10.3390/nano11081880
