Blood transfusion is a vital medical practice, and screening blood for various infectious agents is one of its main components—and concerns. Adequate screening of blood before transfusion is of utmost importance, because incidences of transfusion-transmitted infections (TTIs) are becoming the primary cause of mortalities and morbidities in various populations worldwide [
31]. Several viruses have been identified as being transmitted via blood transfusion, including HBV, HCV, HTLV, and HIV [
32]. These TTIs place significant burdens on healthcare providers around the world, including in Saudi Arabia. Therefore, TTI screening is an essential step in decreasing blood- and blood product transfusion-related biohazards.
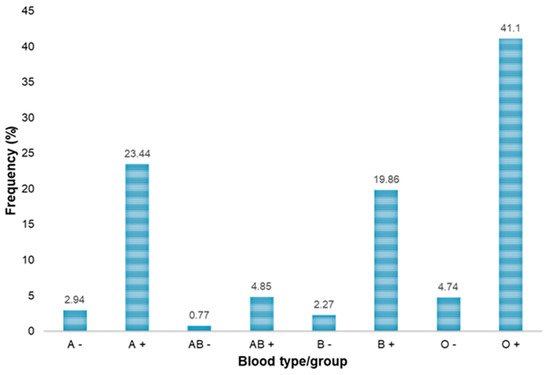
In Saudi Arabia, most of the blood bank laboratories, including that of KKGH, use all of the established serological tests and NATs for screening blood donors. Several studies have reported on the prevalence of various transfusion-transmitted viral diseases in different regions and cities of Saudi Arabia. However, keeping in view the regional differences in disease prevalence and to support the periodic update of the prevalence data in the country, the current study was conducted to estimate the prevalence of HBV and HCV among blood donors of the northern region of Riyadh province. Here, we have retrospectively investigated the incidence of the serological markers and NATs, used for the diagnosis of HBV and HCV, among blood donors. A total of 3733 blood donors were screened for HBV and HCV over a period of 2 years. In addition to donating blood, all the donors included in this study provided socio-demographic information. Out of 3733 donors, 3645 (97.65%) were men and 88 (2.35%) were women. This gender difference is due to the fact that female blood donors are uncommon in Saudi Arabia as compared to other countries. The majority of the donors were 18 to 37 years old, whereas the fewest donations came from older age groups, i.e., 57 years and above. Additionally, the most common blood type was O+ (41.1%), and the least common blood type was AB− (0.77%). A similar distribution of blood groups has been reported by other studies conducted in Saudi Arabia [
23,
33]. The results of serological assays on serum samples from the donors showed that 7 (0.19%), 260 (6.96%), 203 (5.44%) and 12 (0.32%) donors reacted to HBsAg, HBcAb, HBsAb and anti-HCV, respectively (
Table 2).
The seroprevalence of HBsAg among the blood donors included in this study was found to be 0.19%. Previously, various seroprevalence rates for HBsAg have been reported among blood donors in different countries, with 9.8%, 4.1% and 0.087% prevalence rates observed in Nigeria, Ethiopia and Serbia, respectively [
34,
35,
36]. Therefore, as evident from our results, the prevalence rate of HBsAg among blood donors in the current study was low. In Saudi Arabia, regional variations in HBV prevalence are well established in the literature. For example, 3%, 5.4%, 1.5% and 0.3% prevalence rates of HBsAg have been reported among blood donors in the northwest region of Saudi Arabia, the city of Tabuk [
37], southwest Saudi Arabia [
38], the central region of Saudi Arabia [
39] and the Al-Baha region of Saudi Arabia [
25], respectively. The HBV prevalence observed in the present study (0.19%) and in our earlier study (0.33%) [
23], both of which were performed in the north of the Riyadh region, revealed a notable decrease in HBsAg prevalence among the blood donors over time, between 2018 and 2019–2020. El Beltagy et al. proposed risk factors such as increased age, being married, lower educational level, specific occupations such as a blue-collar worker and the military, family history of HBV infection, and lack of immunization, to be associated with the prevalence of HBV infection [
37]. The low prevalence of HBV reported in our study could be attributed to the inclusion of an HBV vaccine and the expanded program of immunization (EPI) in 1998. A study conducted on blood donors from the Al-Baha region showed that the inclusion of an HBV vaccine in the EPI was associated with at least a seven-fold decline in the prevalence of HBV [
25]. Mass vaccination against HBV and the increasing public awareness about HBV infection are the key factors playing important roles in decreasing the prevalence of HBsAg in Saudi Arabia [
26,
40]. The seroprevalence of HBcAb/anti-HBc, another serological marker of HBV, has also reportedly declined in Saudi Arabia, from 15.32% to 9.15% between the years 1998 and 2001 [
17]. The downward trend in the prevalence of anti-HBc appears to have continued ever since, and in the present study, we observed a 6.96% prevalence rate of anti-HBc antibody among the blood donors, which is lower compared to that reported in our previous study (9.81%) in 2018, for the same region.
The prevalence of HCV infection in the present study was 0.32%, which is slightly lower than that reported in our previous study [
23]. Prevalence assessed from Saudi blood donor screening centers indicates HCV infection rates of 0.4–1.1% [
37,
41,
42]. Two studies from Riyadh reported a 1.1% prevalence rate of HCV in 2003 [
43] and 0.4% prevalence rate of HCV in 2004 [
39] among blood donors, which indicates a notable decline in the prevalence of HCV. The 0.32% prevalence rate of HCV among blood donors from the northern Riyadh region in the present study suggests the persistence of low-level HCV among blood donors in Riyadh over time. The inclusion of an HCV vaccine in the EPI contributed to the drop (4.3-fold decrease) in the HCV prevalence [
25]. However, future studies should assess the prevalence in at-risk groups such as drug addicts, people who are sexually active with multiple partners—if possible to identify—and prisoners.