Objective:
We determined the frequency and correlates (sociodemographic, clinical, and personality traits) of poor self-esteem among people with idiopathic epilepsy in demavend, Iran. Our secondary objective was to estimate the psychometric properties and factor structure of a brief Gharagozli-Bhalla Self-Esteem in Epilepsy (GB-SEEQ) Questionnaire.
Methods:
We conducted multiple field exercises to identify patients in our study areas who meet our inclusion criteria. We examined all subjects carefully by using a detailed case-history and reliable questionnaires. We evaluated self-esteem under three broad components of social, home/family, and personal-self. Individual elements included, because of epilepsy, I: (a) feel inferior to others, (b) feel self-conscious, (c) am not fun to be with, (d) other members are better liked than me in the family, (e) doubt if ever be able to succeed my epilepsy, (f) am displeased with myself.
Results:
We identified a total of 52 participants with idiopathic epilepsy, and their mean self-esteem score was 2.2 (95%CI 1.1-3.3; Males: 1.3, 95%CI 0.3-2.9, Females: 3.0, 95%CI 1.4-4.6), p=0.05. The alpha coefficient was 88.7. The factors associated with various components of self-esteem were: neuroticism (78.3x, p=0.004), illiteracy (17.4x, p=0.002), insulted due to epilepsy (13.3x, p=0.003), always thinking about epilepsy (12.3x, p=0.04), unemployment (3.5x, p=0.04), and headache (11.7x, p=0.005), hands tremors (12.9x, p=0.005) and difficulty in finding words (8.9x, p=0.004).
Conclusions:
We found that people with etiologically unknown (idiopathic) epilepsy may have their self-esteem compromised to a certain extent, particularly the females. These results validate our position that people with epilepsy are “more than their mere symptomatic illness”, and that there is a worth in capturing wider patient-reported outcomes, beyond mere seizure frequency and severity. We consider that the usual epilepsy care must go beyond the mere prescription of ASMs.
Full text fully formatted PDF text version and Speech Abstract©:
academia and Egnyte and pr@mail.euclid.int
- Unknown epilepsy
- Idiopathic
- Epilepsy
- Bhalla
- Self-esteem
- Epidemiology
- Intergovernmental Research and Policy Journal
- irpj.academia.edu
INTRODUCTION
People with epilepsy are more than their mere symptomatic illness. By this, we mean that the patient’s cognitive, behavioural or emotional perceptions may also factor for the favourable clinical outcomes and social situation of the affected patients.1 One such factor would be the patient’s self-esteem. Self-esteem is defined as a perception of inner-self in determining relation to oneself. It is an essential concept in chronic conditions, like epilepsy, for numerous reasons. Theories have held that what we believe about ourselves strongly influences our choices, decisions, level of effort and persistence, and how we subsequently perform.1 For instance, low self-esteem is related to procrastination, delay and avoidance2 as an excuse for adverse outcomes. Others have shown that those who report low self-esteem feel vulnerable and discouraged from seeking help.3 On the other hand, higher the self-esteem, the more motivated would be the patient to engage in self-care and coping,4 which, in turn, means the reduced impact of illness on one’s life.5 Self-esteem and self-efficacy are distinct constructs, but, increasing self-esteem could subsequently increase willpower in changing the negative health-related behaviours, which, in turn, builds self-efficacy.6
In case of epilepsy, reducing self-perception of epilepsy as something devaluating and shameful is an important goal of treatment strategy7 because a poor sense of self-esteem contributes to the feelings of being different, which may counteract positive effects of treatment. For instance, others have shown that people with epilepsy feel like a burden on their family, which, in turn, increases their risk of self-injuries and death.8 Similarly, low self-esteem is a barrier against learning of how to live with symptoms and being accustomed to the resultant identity change, which is essential for well-being in epilepsy.9 In contrast, high self-esteem protects against falling into a negative, doubtful state regarding one's ability to cope with or overcome their illness.10
The risk of poor self-esteem may vary depending upon the cultural context of the patients. For instance, in many cultures, epilepsy is seen as a possession by evil spirits.11 In another example, in the 6th century BC Persian Textbook of Avesta,12 the “God states that the persons with epilepsy should not make an offering in honour of him”. So, people with epilepsy may feel the devaluation, shame, secrecy and withdrawal triggered by such negative stereotypes, 13 which may marginalize the patients, and their families and community. In addition, epilepsy is not a single and homogeneous disease condition, which means that the patient’s own sense of esteem may differ with the type of epilepsy and seizures. For instance, etiologically unknown (hereafter referred as idiopathic) epilepsies, by definition, are those for which the underlying cause is not known (i.e., lack of causal inference). So, this ambiguity of identifiable external cause of the illness may mean that patients would perceive themselves as the internal locus of causality, i.e. recognizing oneself as the cause of events, something which is associated with low self-esteem.14 Moreover, the causal ambiguity goes against the theory of locus of control in the sense that others (e.g., medical professionals) are controlling life’s decisions (e.g., medication uptake) rather than the individual himself. Furthermore, confusion about one's identity arising from the idiopathic nature of epilepsy may lead one to maladaptive coping responses of escapism or avoidance of current issues.9
Furthermore, many epilepsy patients never achieve (or maintain) clinical remission despite several therapeutic options,15 which means that adverse psychosocial sequelae would possibly be affecting their therapeutic outcomes in epilepsy.16 Thus, with such a vision, the primary aim of this study was to look into the frequency and correlates of poor self-esteem in persons affected with idiopathic epilepsy in Demavend, Iran. The secondary aim of our study was to estimate the psychometric properties and factor structure parameters of a brief Gharagozli-Bhalla Self-Esteem in Epilepsy (GB-SEEQ) Questionnaire. We believe our work would help to provide means for rapid assessment of self-esteem in usual clinical settings as a way to improve the outcomes of epilepsy for the patient’s wholesome and sustained well-being.
METHODS
Self-esteem and related concepts:
There are related concepts, which are seemingly similar to self-esteem, but those have important differences. For instance, while self-esteem is the feeling self, self-concept is a cognitive self, which is the “the totality of a complex, organized, and dynamic system of learned beliefs, attitudes and opinions that each person holds to be true about his or her personal existence”.17 Self-image is similar to self-concept in that it is all about how you see yourself, and could be based on false and inaccurate thoughts about oneself. While self-esteem is what we think, feel, and believe about ourselves, self-worth is the more global recognition that we are valuable human beings worthy of love. Self-esteem is also not self-confidence because self-confidence is about trust in oneself and one’s ability to deal with challenges, solve problems, and engage successfully with the world.18 So, this way, self-confidence is based more on external measures of success and value than the internal measures that contribute to self-esteem. Finally, self-esteem is also not self-compassion. Self-compassion centers on how we relate to ourselves rather than how we judge or perceive ourselves.19 Being self-compassionate means one is kind and forgiving to oneself, and avoid being harsh or overly critical of self. Of all, self-esteem is referred as one of the basic human needs,19 a necessity to grow as a person and achieve self-actualization, i.e. realization of one's full potential and becoming self-effective.
Recruitment and analysis:
To collect our data, we recruited our participants through 26 rural health house areas in demavend, Tehran. We did the inclusion of all interested adults (at least 15 years of age) with idiopathic epilepsy. 20-21 They could be males or females, resident in their respective village for at least six months, and are otherwise able and interested to participate independently. Throughout our country, each of the 98,000 villages has one functioning health house that is managed by local and trained employees who are from the village itself. The health House staff undergo a mandatory three years’ program that is similar in its content and scope for all health houses of our entire country. All health houses are affiliated to the nearest district hospital. These health houses maintain a structured household file for each household that is under their respective work area, which collects field data about every health-related event. The health house workers are required to maintain regular contact in their allotted area through periodic field visits, which ensures that health-related events do not remain hidden for a long time. This exercise of identifying health-related events remain continuous.
Additionally, we conducted, one month before the start, ancillary verbal information campaign through health house staff, who informed the public in their respective areas about the possibility of having a cost-free convenient consultation at patient’s homes by city specialists. In addition, we enquired with the village residents and fellow patients upon our domestic health visits in the field22-24 about any person who may have remained unidentified but known to these village residents. Unlike popular beliefs, the healthcare system in Iran is of high-quality and reasonably well developed.
All participants underwent careful re-assessment by trained specialists with the help of a reasonably detailed case-history examination. This assessment included details about sociodemographic features, past medical history, natural history, clinical examination, risk factor exposure, precipitating factors, electroencephalogram (EEG) and CT or MRI results, and treatment (both traditional and modern) aspects. We classified patients based on etiological types as idiopathic, among whom no conventional underlying etiological factor was confirmed or suspected to be present, either currently or in the past.20-21
The criteria for the diagnosis of epilepsy were a clear description of the recurrent and paroxysmal time-limited change in motor activity or behaviour. The consciousness was the major discriminator. The seizures were categorized based on available patient information to derive a best fit seizure classification.25 Also, as per standard practice,25 our participants did not include people with acute symptomatic seizures, febrile seizure or single isolated seizure.
We evaluated self-esteem by using GB-SEEQ for plausible representation and perception of epilepsy-related self-esteem under three broad components: social, home/family, and personal self. The items included, because of epilepsy, I: (a) feel inferior to others, (b) feel self-conscious, (c) am not fun to be in the home/family, (d) other members are better liked than me in the family, (e) doubt if ever be able to succeed my epilepsy, (f) am displeased with myself. Upon a review of possible literature 26 and hands-on experience with epilepsy, we prepared a pool of items that possibly represent perceptions about self-esteem. After that, a series of discussions took place and items that were deemed to be most relevant in representing the perceptions of poor self-esteem in epilepsy were selected. While doing this, we followed the requirements of relevance, brevity, feasibility, readability, consistency of style and formatting, and clarity of the language.
The content validity was assessed qualitatively by an expert panel of specialists from neurology, mental health, and public health. We used the responses from this panel to improve the items. Content validity index (CVI) was measured, and a CVI score higher than 0.75 was considered acceptable.27 The responses to each of the six epilepsy-related elements of self-esteem were dichotomous based on the patient’s subjective perception about the absence (score zero) or presence (score one) of those elements. Each patient’s self-esteem score was the sum of the total number of elements that were reportedly present among them, which were then averaged for the entire sample population as well as for the males and females. The higher the score on a range of 0-6, the poorer was the self-esteem. Besides, we analyzed the big five personality traits (openness, conscientiousness, extraversion, agreeableness, and neuroticism) by using validated ten-item personality inventory.28
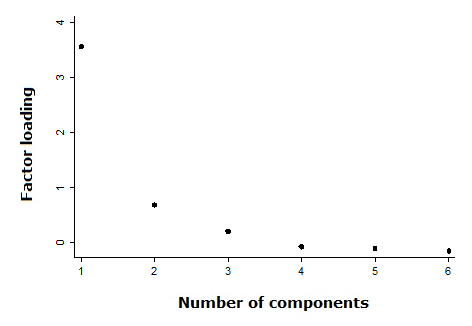
In order to analyze, the proportions and means were compared by using Z-test and t-test, respectively, wherever required. Wherever required, the data were summarized descriptively in terms of mean, number, frequency, proportion, 95% confidence interval (CI). The psychometric properties were determined by measuring the alpha coefficient for all and individual items. Those items that had had a low (<0.3) item-test correlation were planned to be deleted. Alpha coefficient was also measured group-wise, i.e., separately for responding yes or no to an item. We did exploratory factor analysis (EFA) to determine the possible number of latent factors that items altogether could be categorized into, by using eigenvalue ≥1.0 and factor loadings ≥0.40. We used the scree plot for EFA.
For confirmatory factor analysis (CFA), we estimated fit indices, size of residual, and coefficient of determination. Sampling adequacy was determined by measuring the Kaiser-Meyer-Olkin (KMO) Test for sampling adequacy. After that, by using logistic regression, we determined the association of individual self-esteem elements with all possible independent variables separately, after constraining the effects of sex. The bootstrap method was used with 100x replication of our sample to determine the odds of association between variables, should the application of sample be replicated 100-times. The results were also calculated in terms of effect size, which does not depend upon the sample size, unlike other measures of association.
In a posthoc manner, by using the mean self-esteem score of our sample, the expected general population mean self-esteem score of 3.0 (i.e., the midway of the possible self-esteem score of 0-6), a standard deviation of 2.0, two-sided alpha of 0.05, power of 80.0%. In addition, by using similar parameters as above along with the actual sample size of 52 subjects, the power of our sample was determined. We obtained informed consent from all interested subjects before permitting their participation. We obtained ethics approval from the Institutional Review Board of Shahid Beheshti University of Medical Sciences, Iran.
RESULTS
We identified a total of 52 participants with idiopathic epilepsy. The cases had a median age of 39.0 (95%CI 33.3-44.7 years. The cases were males (45.0%), married (70.0%) and illiterate (35.0%). Active epilepsy was present in 85.0% of subjects, 80.0% had generalized seizures.
The mean self-esteem score was 2.2 (95%CI 1.1-3.3), which was 1.3 (95%CI 0.3-2.9) among the males and 3.0 (95%CI 1.4-4.6) among the females, p=0.05. The most frequent reported self-esteem elements were those related to the personal self (42.5%) followed by social (30.0%) and family/home aspects (27.5%). Upon logistic regression, the neuroticism was associated with the self-esteem element of “being displeased with myself” (78.3, 95%CI 41.1-115.5), p=0.004.
From among the treatment-related side-effects, after constraining the effects of sex, the social self-esteem elements of “feel inferior to others” and “feel self-conscious” was associated with hands shake all the time (12.9, 95%CI 9.8-16.0, p=0.005). Home/family self-esteem element of “am not fun to be in the home/family” was associated with easy to become agitated and restless (12.3, 95%CI 10.9-13.9, p=0.004). Personal self-esteem element of “doubt if ever be able to succeed my epilepsy” was associated with difficulty in word-finding, names and appointments (8.9, 95%CI 7.4-11.1, p=0.04).
Among the social and clinical variables, after constraining the effects of sex, the Home/family self-esteem element of “am not fun to be in the home/family” was associated with always thinking about epilepsy (12.3, 95%CI 11.0-13.9, p=0.004) and often suffer from headache (11.7, 95%CI 9.4-14.6, p=0.005). Home/family self-esteem element of “other members are better liked than me in the family” was associated with illiteracy (17.4, 95%CI 13.0-22.7, p=0.002), sometimes can not do anything because of headache (10.2, 95%CI 9.4-11.0, p=0.005), and having been insulted due to epilepsy (13.3, 95%CI 12.3-14.3, p=0.003). Personal self-esteem element of “displeased with myself” was associated with unemployment (3.5, 95%CI 1.2-12.3, p=0.04).
The alpha coefficient of GB-SEEQ was 88.7, while none of the items had this coefficient lesser than 0.86. For individual items, the item-test correlation was no less than 0.78. By group, the alpha coefficient was 0.85 and 0.93 for those reporting a yes and those reporting a no to the questionnaire items, respectively. Upon EFA, we found a one-factor structure for our questionnaire with a cumulative variance of 86.9%, figure 1. The KMO for sampling adequacy was 0.79. Upon CFA, we found a 90.0% coefficient of determination, 0.80 fit index, and a small (0.09) standardized residual. By using mean self-esteem score of our sample, the expected general population mean self-esteem score of 3.0 (i.e. midway of the self-esteem score range of 0-6), a standard deviation of 2.0, two-sided alpha of 0.05, power of 80.0%, the required sample size was 49. In addition, by using the similar parameters as above along with the actual sample size of 52 subjects, our sample had the 82.2% power to detect the mean self-esteem score that we had in our sample population.
Figure 1: Screeplot showing the underlying one-factor structure of Gharagozli-Bhalla Self Esteem in Epilepsy questionnaire (GB-SEEQ)
DISCUSSION
The methods of our study were adequately robust for many reasons. For instance, we had participants with idiopathic epilepsy; which means that their risk to have poor self-esteem was not likely to be confounded by many of the underlying factors such as head trauma.29 Our cultural context was also appropriate for appraising self-esteem since, on one hand, The Holy Quran instructs “Surely Allah does not change the conditions in which a people are in until they change that which is in themselves” (Chapter 13, verse 11). While, on the other hand, old scriptures such as the 6th century BC Persian Textbook of Avesta,12 it is stated that “the persons with epilepsy should not make an offering in honour of God”. Nevertheless, self-esteem remains poor among people with epilepsy in the region where Iran is located.7
In addition, our sample size was an estimated one, and our sample power was adequately high. Generally, regular practice is to report the odds ratio alone,30 which is not the correct measure of association.31 Here, we estimated effect size because it does not depend on the sample size. We also used the bootstrap method; which provided results after replicating our sample the 100 times. Our participants were from the general population; hence, they were not selective as could have been with other study designs. Our participants were resident, both males and females and with active epilepsy.
Furthermore, our questionnaire relates well to common representations of self-esteem. It also relates well to theoretical frameworks, such as the appraisal theory of emotion, which asserts that our emotions (i.e., self-esteem) are determined by our appraisal of the stimulus (i.e., epilepsy). Moreover, we employed various means to identify our participants. Our assessment, as shown above, covered many aspects of the subject’s case history and was done by trained specialists. We used standard criteria for reaching the diagnosis of idiopathic epilepsy and seizure types.25 We can externalize our sample with a simple example. For instance, idiopathic epilepsies are more frequent among females, which was seen in our sample as well.
Self-esteem is a clinically relevant parameter in epilepsy. For instance, by improving self-esteem, one may reduce the symptomatology and have improved quality of life.14-15 Low self-esteem is a possible obstacle in effective self-management and coping, such as by negatively affecting one’s willpower to adhere. Low self-esteem may also lead to mental health issues such as depression or anger, which may further compound the negative impact of epilepsy on one’s life.32
In our study, the mean self-esteem was poorer among females than males, but, upon logistic regression, there was no association between sex and self-esteem components. These results are consistent with current data from numerous countries that have shown that males display higher self-esteem than females.33 Any pattern of sex difference in self-esteem is possibly the result of multiple macropsychological mechanisms and a broad set of social, economic, demographic and cultural value indicators that guide culture-specific self-esteem development in males and females.33 Another possible explanation for a sex difference in self-esteem could be related to the fact that females are more likely to have neurotic traits than males,34 which was found to be strongly related to being “displeased with myself” in our study. Neuroticism is the most studied personality trait in the health literature, and its association with poor self-esteem is not unexpected.35 So, from these results, we may infer the need to include personality trait assessment as a part of usual epilepsy care, more so since therapy may alter negative personality traits, 36 which may help the patients in their day-to-day management of epilepsy.37 Moreover, treating physicians may also consider complementing behaviour-modifying positive body image interventions38 that help to trounce unhealthy beliefs to ensure one’s acceptability to oneself. The association of hand tremors with self-esteem can also be understood through possible subjective alternation in body image and self-concept among the patients due to their epilepsy or its treatment.39 Thus, active engagement of theory-based behaviour-modifying positive body image interventions, such as persuasive cognitive dissonance,38 within usual epilepsy care may help to trounce unhealthy patient beliefs to ensure one’s acceptability to oneself.
The personal component of self-esteem was associated with unemployment and the side-effect of difficulty in finding words, names and appointments. Being gainfully employed allows one to feel content in personal, familial and social aspects of life.40 But, unemployment contributes towards ill health and influence peoples’ development, life’s pleasures, quality of life and self-esteem in a negative way.40 The association of self-esteem with unemployment in our study is reasonable since economic inactivity is strongly related to self-esteem.41 Unlike many other conditions, epilepsy could be more disruptive and poorly acceptable socially, which may interfere with the epilepsy patient’s chances of being employed.42 So, based on these results, we may infer the need for health agencies to improve the unfair prejudices and stereotypes (e.g., related to accidents and absenteeism from work43) of possible employers towards epilepsy.44 Also, the health agencies should focus on creating job quota system for people with epilepsy or develop occupations that are adapted to epilepsy, such as the micro-franchisee program designed by the last author. In this micro-franchisee program, the recovered (or well-controlled) epilepsy patients work as “local advocacy, support, and domestic health visiting agent” in their own rural settings in exchange for an honorarium and a bicycle.22-24
Another factor related to the personal component of self-esteem was the difficulty in finding words, names and appointments. Mild cognitive restrictions are common for people with epilepsy.45 So, we may infer that treating physicians should make use of cognitive training interventions to deal with such anticipated issues, either from the prolonged use of ASMs or from seizure-induced brain injuries and neurodegeneration.46 Others have also shown that those who undergo cognitive training achieve improved functional connectivity.47 Similar could be the strategies for other side-effect issues that were found to be associated with self-esteem, for instance, hand tremor, which is an established side-effect48 with ASMs, especially with valproate. Thus, instead of vague follow-ups, the health agencies should seek to develop a system of periodic follow-up contact with the patients to help issues identified early-on, through, for instance, domestic health visitors. 22-24 This way, treating physicians would have the possibility to optimize doses or change ASMs in an appropriate time and manner.48
The factors that affected the home/family component of our patient’s self-esteem were headache, having been insulted due to epilepsy, always thinking about epilepsy, and illiteracy. People with epilepsy are less likely to follow their mandatory education well or be adequately employed, which is a risk for their adequate self-esteem. There is a substantial overlap between illiteracy and one’s self-esteem through, for instance, unhealthy concepts and evaluations.4,7,10 For instance, people with low literacy levels are often viewed as unintelligent, unproductive and deficient, which may or may not be true though.49 Illiteracy is also associated with increased dependence upon others, poor coping and mental health;50 which may affect one’s esteem through internalizing and externalizing ways. Unfortunately, illiteracy is not a factor that can be modified at the patient level, but, high levels of health literacy may translate into less harmful psychological elements.51 Furthermore, the association of insult due to having epilepsy with self-esteem is not unexpected either. Feeling offended is a self-conscious emotion52 like shame, and is typically trigged by a blow to a person’s honour, hence to one’s public face.
Another factor related to low self-esteem was “always thinking about epilepsy”. Always thinking about epilepsy may precipitate into a constant state of anxiety or fear, which is relatively reasonable since epilepsy is a long-term illness, and the onset of seizures is sudden, unpredictable and unprovoked. A variety of cognitive-behavioural therapies are available, which can help patients confront the pervasive effects of epilepsy or its treatment (e.g., headache) through self-responsibility, self-acceptance, and self-assertiveness.53 For instance, cognitive-behavioural therapies may help epilepsy patients to overcome anxiety attacks, feelings of having no control over one’s life and being completely helpless.
We also estimated the psychometric properties of our B-GEQ questionnaire. The alpha coefficient of internal consistency was considerably higher than the usual criteria of 0.70. High alpha coefficient means that all our elements were in line with each other to measure a common underlying construct together. Also, our questionnaire was not biased to raise one particular type of participant response since the group alpha coefficient for responding a yes to an item (a0.85), and no to an item (a0.93) was sufficiently high and similar to each other. Besides these, our factor structure was also adequate, for instance, 90.0% coefficient of determination, 86.9% cumulative variance, and 0.09 as the standardized residual. For factor analyses, we used conventional parameters, such as eigenvalue ≥1.0 and factor loading ≥0.40.
Lastly, as usual, our work has a few limitations. We looked at three explicit self-esteem dimensions of personal/self, society and home/family although other dimensions may also be possible, such as religion practice. We believe that given the cultural influence on the patient’s self-esteem, the results may vary between populations. For example, in communities where epilepsy is considered as a demonic possession,11 the possibility of a person’s isolation and insult would be higher than elsewhere.
One popular perception among most is that the use of both positively and negatively worded items in questionnaires is necessary and prevents response bias.54 First of all, a mix of positive and negative worded items often produces uninterpretable patterning of answers, such as, someone who is both affected and unaffected. This kind of uninterpretable pattern could be due to the reasons of social desirability, momentary instinct, inattention, confusion, difficulty, cognitive fatigue, etc. of participants or questionnaire items. For example, after a set of positive worded questions, the respondent may miss the fact that consecutive item is worded negatively compared to the previous one;55 making the entire questionnaire answering process counter-productive. Others have also shown that mix worded items are prone to careless responding and cognitive fatigue and introduces noise, known as measurement error.56 For such reasons, we had designed our questionnaire with items indicating in a single lone direction. Also, our questionnaire used “I”, instead of “you”, which can make an important difference in relating the questionnaire items to the respondents, everytime an item is read.
Another popular argument could be that our items are worded negative. This was so because the focus of our interest was on the impact of epilepsy in causing the deprivation of one’s self-esteem, which is a therapeutically important measure.14-15 A negatively worded question is appropriate where disagreement would be a good answer, which matches well with the hypothesis of this study.14-15 A problem with positive worded measures or previous existing measures is that they can be affected by the desire to portray the self positively, i.e. desirable self-image.57
In contrast, the use of neutral worded items are likely to produce unintended multidimensionality in the questionnaires due to response bias.58 The neutral worded options provide an easy out for the respondents who are less inclined to express their opinion. A questionnaire can be considered incorrect mainly if it does not allow the possibility to the participants of saying a no to a questionnaire item, which our questionnaire did. One may also see that the alpha coefficient of responding a yes and no to an item was similar to each other, which automatically means that there was no bias in deriving a particular kind of response to an item. Nevertheless, there is no acceptable gold-standard in the questionnaire design, and there are plenty of arguments that support or un-support the use of mixed, positive, negative, or neutral worded items, be bivariate or likert in nature.
One may also argue that such construct should be measured indirectly, but the tools available are those that are on self-concept,59 and not specifically designed for epilepsy. As far as we are aware, ours is the only validated tool that has been designed specifically for evaluating self-esteem in epilepsy. Moreover, others have already shown that the correlations between explicit and implicit measures are often quite small.57
Another trivial argument one may provide is about the idiopathicity of epilepsy that it continues to change with improved diagnostic evaluations. However, the veracity is not so, and there has been no well-established new epilepsy etiological or risk factor, or any new diagnostic modality established on the ground that has significantly improved diagnostic competence beyond what is already known. Others have also shown that the proportion of epilepsies with unknown etiology has remained substantially unchanged in more recent years, including in high-income countries.21 Another trivial argument some may provide relates to the etiological classification, which is not beyond a mere re-arrangement of etiological groups that neither invalidates those with unknown etiologies nor the previous well-established “classification” system. For instance, metabolic, infectious, structural etc. lied under symptomatic epilepsies, and now these have been merely seperated from each other. Those epilepsies where the underlying cause remains unknown has not disappeared as others interpret.
CONCLUSION
To conclude, within the strengths and limitations of this study, we found that people with etiologically unknown (idiopathic) epilepsy in a non-western context may have their self-esteem compromised to a certain extent, particularly the females. These results validate our position that people with epilepsy are “more than their mere symptomatic illness”, and that there is a worth in capturing wider patient-reported outcomes, beyond mere seizure frequency and severity. By taking upfront the epilepsy patients as “more than their mere symptomatic illness”, we might be in a better position to reduce the compound impact of epilepsy on one’s physical, mental, and social well-being through complementing behavioural therapies with usual ASMs. However, it is necessary to estimate the effect one, and who, may obtain from such complementary therapeutic approaches in epilepsy.
SUPPLEMENT
Conflicts of Interest: DB receives research funds and attends and gives a talk in meetings that may have been funded directly or indirectly by commercial entities. The author is under the authority of UN treaty based public International Law. All other authors have no conflicts of interest.
Acknowledgment/Funding: The funding was procured from Shahid Beheshti University of Medical Sciences, Iran and Brain Mapping Research Centre (Shahid Beheshti University of Medical Sciences), Tehran, Iran. The funding agencies had no role in writing, editing, approval, or decision to publish.
REFERENCES
- Bandura A. Self-efficacy: The exercise of control. New York: Worth Publishers; 1997.
- Ferrari J. Dysfunctional procrastination and its relationship with self-esteem, interpersonal dependency, and self-defeating behaviors. Pers Indiv Differ. 1994;17(5):673-9.
- Zartaloudi A. Help-seeking as a threat to self-reliance and self- esteem of an individual with mental health problems: a questionnaire survey. Hellenic J Nurs Sci. 2010;3(3):67-74.
- Davis L, Kurzban S, Brekke J. Self-esteem as a mediator of the relationship between role functioning and symptoms for individuals with severe mental illness: a prospective analysis of Modified Labeling theory. Schizophr Res 2012;137(1):185-9.
- Clark NM, Dodge JA. Exploring self-efficacy as a predictor of disease management. Health Educ Behav. 1999;26:72-89.
- Flay BR, Petraitis J. The theory of triadic influence: a new theory of health behavior with implications for preventive interventions. Adv Med Sociol. 1994;4:19-44.
- Baker G, Jacoby A, Gorry J, et al. Quality of life of people with epilepsy in Iran, the Gulf and Near East. Epilepsia. 2005;46:132-40.
- Sawangchareon K, Pranboon S, Tiamkao S, et al. Moving the Self-Esteem of People with Epilepsy by Supportive Group. J Caring Sci. 2013;2(4):329-35.
- Mann M, Hosman C, Schaalma, et al. Self-esteem in a broad spectrum approach for mental health promotion. Health Educ Res.2004;19:357-72.
- Strecher VJ, DeVellis BM, Becker MH, et al. The role of self-efficacy in achieving health behavior change. Health Educ Behav. 1986;13:73-92.
- Shibre T, Alem A, Tekle-Haimanot R, et al. Community attitudes towards epilepsy in a rural Ethiopian setting: a re-visit after 15 years. Ethiop Med J. 2008;46:251-59.
- Vansan A, Paladin F. Epilepsy and Persian culture: an overview. Epilepsia. 1992;33:1057-64.
- Ritsher J, Otilingam P, Grajales M. Internalized stigma of mental illness: psychometric properties of a new measure. Psychiatr Res. 2003;12:31-49.
- Shaha S. The Relationship of Self-Concept to Causal Attributions. ERIC. 1982;23:1-23.
- Hughes D, Bonnett L, Czanner G, et al. Identification of patients who will not achieve seizure remission within 5 years on AEDs. Neurol. 2018;91(22):e2035-e44.
- Jalava M, Sillanpää M, Camfield C, et al. Social adjustment and competence 35 years after onset of childhood epilepsy: a prospective controlled study. Epiilepsia. 1997;38(6):708-15.
- Purkey W. An Overview of Self-Concept Theory for Counselors. ERIC Clearinghouse on Counseling and Personnel Services. 1988;1988:ED304630.
- Baumeister RF, Campbell JD, Krueger JI, et al. Does high self-esteem cause better performance, interpersonal success, happiness, or healthier lifestyles? Psychol Sci Pub Int. 2003;4:1-44.
- Gilbert P, Procter S. Compassionate mind training for people with high shame and self-criticism: Overview and pilot study of a group therapy approach. Clin Psychol Psychother. 2006;13:353-79.
- Berg A, Berkovic S, Brodie M, et al. Revised terminology and concepts for organization of seizures and epilepsies: Report of the ILAE Commission on Classification and Terminology, 2005–2009. Epilepsia. 2010;51(4):676-85.
- Beghi E. The Epidemiology of Epilepsy. Neuroepidemiol. 2020;54:185-91.
- Hun C, Hok T, Bhalla D. Epilepsy: some controversies, some knowledge and some experience from Cambodia. Neurol India. 2014;62(6):606-9.
- Bhalla D. Domestic health visiting: an innovative approach to bridge Gaps in epilepsy care in Laos and Cambodia. Varetz, France: 2012.
- Bhalla D. Epilepsy in Cambodia: results and perspectives. Ho Chi Minh, Vietnam: 2011.
- Commission. Proposal for Revised Clinical and Electro encephalographic Classification of Epileptic Seizures. Epilepsia. 1981;22:489-501.
- Abdel-Khalek A. Introduction to the Psychology of self-esteem. In: Holloway F, Ed. Self-Esteem-Perspectives, influences, and improvement strategies. USA: Nova Science; 2016. p. 5-125.
- Lawshe CH. A quantitative approach to content validity. Personnel psychology. 1975;28(4):563-75.
- Ahmadi A. Reliability and Validity of the 10-Item Personality Inventory. Psychol Russ. 2019;12(3):30-6.
- Ponsford J, Kelly A, Couchman G. Self-concept and self-esteem after acquired brain injury: a control group comparison. Brain Inj. 2014;28(2):146-54.
- Viera AJ. Odds ratios and risk ratios: what's the difference and why does it matter? South Med J. 2008;101(7):730-4.
- Chen H, Cohen P, Chen S. How Big is a Big Odds Ratio? Interpreting the Magnitudes of Odds Ratios in Epidemiological Studies. Communication in Stats. 2010;39(4):860-4.
- Sowislo JF, Orth U. Does low self-esteem predict depression and anxiety? A meta-analysis of longitudinal studies. Psychol Bull. 2013;139:213-40.
- Bleidorn W, Arslan R, Denissen J, et al. Age and Gender Differences in self-esteem-A Cross-Cultural Window. J Pers Soc Psychol. 2016;111(3):396-410.
- Weisberg Y, DeYoung C, Hirsh J. Gender differences in Personality across the Ten aspects of the Big Five. Front Psychol. 2011;2:178-82.
- Ormel J, Rosmalen J, Farmer A. Neuroticism: a non-informative marker of vulnerability to psychopathology. Soc Psychiatr Psychiatric Epid. 2004;39(11):906-12.
- Roberts B, Luo J, Briley D, et al. A systematic review of personality trait change through intervention. Psychol Bull. 2017;143(2):117-41.
- Holmes E, Hughes D, Morrison V. Predicting Adherence to Medications Using Health Psychology Theories: A Systematic Review of 20 Years of Empirical Research. Value Health. 2014;17(8):863-76.
- Stice E, Rohde P, Durant S, et al. A preliminary trial of a prototype Internet dissonance-based eating disorder prevention program for young women with body image concerns. J Consult Clin Psychol. 2012;80(5):907-16.
- Lukianowicz N. "Body Image" Disturbances in Psychiatric Disorders. Br J Psychiatr. 1967;113(494):31-47.
- Axelsson A, Andersson I, Edén L, et al. Inequalities of Quality of Life in Unemployed Young Adults: A Population-Based Questionnaire Study. Int J Equity Health. 2007;6(1):25-31.
- Kwong K, Lam D, Tsui S, et al. Self-esteem in adolescents with epilepsy: Psychosocial and seizure-related correlates. Epilepsy Bbehav. 2016;63:118-22.
- Krumholz A, Hopp J., Sanchez A. Counseling epilepsy patients on driving and employment. Neurol Clin. 2016;34(2):427-42.
- Johnson E. Perspectives on work for people with epilepsy. In: Schultz I, Gatchel J, editors. Handbook of return to work. 2. New York: Springer; 2016. p. 617-32.
- Chaplin J. Vocational assessment and intervention for people with epilepsy. Epilepsia. 2005;46(1):55-6.
- Vingerhoets G. Cognitive effects of seizures. Seizure. 2006;15(4):221-26.
- Golino M, Flores-Mendoza C. Desenvolvimento de um programa de treino cognitivo para idosos. Rev Bras Geriatr Gerontol. 2016;19(5):769-85.
- Sherman D, Mauser J, Nuno M, et al. The Efficacy of Cognitive Intervention in Mild Cognitive Impairment (MCI): a Meta-Analysis of Outcomes on Neuropsychological Measures. Neuropsychol Rev. 2017;27(4):440-84.
- Morgan J, Harrison M. Antiepileptics. In: Factor S, Lang A, Weiner W, editors. Drug induced movement disorders. 1. Malden: Blackwell Futura; 2005. p. 408-29.
- Lipnevich A. Low Self-Esteem: Myth or Reality? Focus on Basics-Connecting research with practice. 2006;8:3-6.
- Maughan B, Carroll J. Literacy and Mental Disorders. Curr Opin Psychiatr. 2006;19(4):350-4.
- ASEM. Approaches to Reducing Stigma. In: Academies of Sciences and Medicine, Ed. Ending Discrimination against People with Mental and Substance Use Disorders: The Evidence for Stigma Change. 1. Washington, DC: National Academies Press (US); 2016. p. 50-72.
- Lewis M. Self-conscious emotions: embarrassment, pride, shame, and guilt. In: Lewis M, Haviland-Jones J, Feldman Barrett L, editors. Handbook of Emotions 3. New York: Guilford Press; 2008. p. 742-56.
- Foddis W. Branden's Self-Esteem Theory within the Context of Academic Psychology. J Ayn Rand Stud. 2016;16(1):187-206.
- Rorer L. The great response-style myth. Psychol Bull. 1965;63:129-56.
- Krosnick J. Survey research. Annu Rev Psychol. 1999;50:537-67.
- Bradley K, Royal K, Bradley J. An investigation of ‘honesty check’ items in higher education course evaluations. J Coll Teach Learn. 2008;5(8):39-48.
- Heine S, Lehman D. Culture, self-discrepencies, and self-satisfaction. Personal Soc Psychol Bull. 1999;25:915-25.
- Spector P, VanKatwyk P, Brannick M, et al. When two factors don't reflect two constructs: How item characteristics can produce artifactual factors. J Manag. 1997;23:659-77.
- Greenwald. A., Farnham S. Using the Implicit Association Test to Measure Self-Esteem and Self-concept. J Personal Soc Psychol. 2000;79(6):1022-38.
Publisher information: The Intergovernmental Research and Policy Journal (IRPJ) is a unique interdisciplinary peer-reviewed and open access Journal. It operates under the authority of the only global and treaty-based intergovernmental university in the world (EUCLID), with other intergovernmental organizations in mind. Currently, there are more than 17,000 universities globally, but less than 15 are multilateral institutions, EUCLID, as IRPJ’s sponsor, is the only global and multi-disciplinary UN-registered treaty-based institution.
IRPJ authors can be assured that their research will be widely visible on account of the trusted Internet visibility of its “.int” domain which virtually guarantees first page results on matching keywords (.int domains are only assigned by IANA to vetted treaty-based organizations and are recognized as trusted authorities by search engines). In addition to its “.int” domain, IRPJ is published under an approved ISSN for intergovernmental organizations (“international publisher”) status (also used by United Nations, World Bank, European Space Agency, etc.).
IRPJ offers:
- United Nations Treaty reference on your published article (PDF)
- “Efficiency” driven and “author-focused” workflow
- Operates the very unique author-centric metric of “Journal Efficiency Factor”
- Minimal processing fee with the possibility of waiver
- Dedicated editors to work with graduate and doctoral students
- Continuous publication i.e., publication of articles immediately upon acceptance
- The expected time frame from submission to publication is up to 40 calendar days
- Broad thematic categories
- Every published article will receive a DOI from Crossref and is archived by CLOCKSS.
Submit manuscript: pr@mail.euclid.int
EICs: Prof. Charalee GRAYDON, JD; Prof. Devender BHALLA, HDR
Full text fully formatted PDF text version and Speech Abstract©:
academia and Egnyte and pr@mail.euclid.int
All copyrights remain with the author(s) and IRPJ.
Please cite as: Gharagozli, K., Amini, F., Lotfalinezhad, E., Mirghafari, M., Delbari, A., Bhalla, D. Self-esteem in idiopathic epilepsy and psychometric properties of Gharagozli-Bhalla Self-esteem in Epilepsy Questionnaire. Intergovernmental Res Pol J (UN treaty). Vol. 2020, Issue e20, DOI: 10.36964/irpj2357, Article ID: 204, pages 1-11.