Amblyopia is the most common cause of monocular poor vision affecting up to 3.7% of the global population. Classically, the first step in treatment has been optical correction, followed by patching and/or pharmacological treatment. However, this is an evolving scenario, since researchers and clinicians are interested in new binocular treatments due to the increasing development of new technologies. In this article main, current binocular treatments as Dig Rush, falling blocks, I-BiT, Occlu-tab, Vivid Vision, and movies are reviewed for binocular amblyopia management.
- amblyopia
- binocular treatment
- dichoptic movies
- video games
1. Introduction
Amblyopia of the eye, also called “lazy eye”, is a disorder of sight defined as a decreased best corrected visual acuity (BCVA) of one or both eyes without any organic abnormality or pathology of the globe. Clinically, monocular amblyopia is defined as a BCVA of two or more lines less than the fellow eye [1].
Amblyopia comprises a limited visual function including a compromised form, color, and motion perception [2]. In a recent systematic review and meta-analysis published in 2018, Hashemi et al. [3] concluded that the pooled prevalence estimate of amblyopia was 1.8%, with the highest estimate in European Regional Office (3.7%) and the lowest in Africa Regional Office (0.5%).
2. Types of Amblyopia
Generally, amblyopia is caused by strabismus (loss of ocular alignment), anisometropia (loss of focus), visual deprivation (loss of form vision), or reverse amblyopia (due to too aggressive amblyopia therapy) [6,7]. A mixed amblyopia is common since strabismus and anisometropia can take place together.
2.1. Anisometropic Amblyopia
Anisometropia is the condition in which both eyes have unequal refractive power. Generally, a difference in two or more diopters is the accepted threshold to label the mentioned condition [8]. It can be present in myopic, hyperopic, or astigmatic patients. Moreover, is possible to have an isoametropic amblyopia if both eyes have a similar uncorrected high refractive error and both become amblyopic. Severity of the refractive error and the amblyopia are directly related. According to Hashemi et al. [3], the most common cause of amblyopia was anisometropia (61.6%).
2.2. Strabismic Amblyopia
Strabismus occurs when one eye is not properly aligned, so it may turn inwards (esotropia), outwards (exotropia), downwards (hypotropia), or upwards (hypertropia). The strabismus can be present some of the time (intermittent) or all the time (constant). Constant strabismus led to more severe amblyopia than intermittent ones [2].
Strabismic amblyopia is secondary to strabismus. The brain suppresses the image of the deviating eye as a result of a process to avoid double vision developing anomalous retinal correspondence occasionally [9]. Retinal points in the right and left eyes, which receive stimuli from one object in space, have the same visual direction despite a manifest motor deviation. Patients with anomalous retinal correspondence could have certain degree of peripheral fusion and clumsy stereopsis.
2.3. Deprivation Amblyopia
Deprivation amblyopia is the most unusual and, typically, the most severe form of amblyopia. It develops when the visual axis is covered. Various causes of stimulus deprivation include eyelid ptosis, cornea opacities, cataracts, and vitreous hemorrhage, among others [5]. An early treatment of the deprivation etiology is essential to avoid or soften this form of amblyopia.
2.4. Reverse Amblyopia
Finally, other infrequent cause of amblyopia is reverse amblyopia. It is a special case of iatrogenic deprivation amblyopia following the patching or atropine excess of the dominant eye and becoming amblyopic as a result [10].
3. Classical Treatments
3.1. Optical Correction
Treatment of the refractive errors is probably the first-line management for amblyopia. For many decades, the Pediatric Eye Disease Investigators Group (PEDIG), the Monitored Occlusion Treatment of Amblyopia Study Cooperative Group (MOTAS Cooperative), and other authors claimed that optical treatment is a good first-line therapy for both anisometropic and strabismic amblyopia [11–13]. The amblyopic eye improves the BCVA rapidly during the first 15 weeks when a plateau in visual curve is reached, after which BCVA improves only slowly [11].
A meta-analysis based on 29 articles indicated that although refractive adaptation can improve visual acuity in amblyopic eyes, its effect is significantly decreased with older age. Moreover, visual acuity improves as treatment progresses and a better initial acuity is associated with a higher improvement effect [14].
3.2. Patching
Patching is usually an effective second-line treatment for amblyopia. This treatment is based on patching the fellow eye for some hours per day depending on the degree of amblyopia. Usually, the patient has been previously motivated to do near tasks as those activities stimulate the visual system. In 2008, the PEDIG group in a randomized clinical trial found that near and distance tasks had similar effects on amblyopia treatment success [15]. Guidelines from the American Academy of Ophthalmologists [16] and the Royal College of Ophthalmologists [17] advised to use a 6 h patching for severe amblyopia and 2 h occlusion for moderate ones.
In 2019, a large retrospective study of real-world outcomes of amblyopia treatment using PEDIG amblyopia protocols in 877 patients treated at a single center was published [18]. The study population achieved outcomes comparable to those demonstrated by the PEDIG studies in terms of treatment hours.
3.3. Pharmacological Treatment
Pharmacological treatment is an alternative treatment for amblyopia when the visual acuity is not fully improved by optical correction, patching is not possible, or a low compliance is detected. The most used drugs are topical atropine and oral levodopa-carbidopa. Their mechanism of action acts by blurring the non-amblyopic eye. Levodopa is converted to dopamine; for the retinal mechanism of action and for cortical mechanism, it has been suggested that increased dopamine levels lead to shrinkage in the size of the receptive field and produce a reduction in the size of the suppression scotoma, respectively, improving visual acuity [19].
In 2002, the PEDIG compared the effectiveness of patching and atropine treatments for moderate amblyopia in 419 children younger than 7 years. Improvement was initially faster in the patching group, but after 6 months, visual acuity improvement was similar in both groups [20].
Afterwards, the PEDIG evaluated the effect of daily topical atropine prescribed for the dominant eye in 195 children from 3 years old to younger than 7 years of age with moderate amblyopia. A beneficial effect was demonstrated with atropine treatment, and in 55 children who did not respond properly to atropine alone, a plano spectacle lens was prescribed to improve visual acuity [21].
Moreover, Repka et al. [22] compared daily atropine to weekend atropine treatment for 168 children younger than 7 years with moderate amblyopia. In short, daily and weekend atropine treatment provided similar visual acuity improvement.
Seol et al. [23] assessed the efficacy of intermittent atropine penalization (one drop in the dominant eye twice a week) for 4 months in 41 children where the mean age was 5.59 ± 1.52. For all the children included in this study, patch therapy had failed previously.
Regarding levodopa as a treatment, Repka et al. [24] compared the efficacy of levodopa as adjunctive treatment to patching by comparing its effect against with treatment with placebo and patching. They found that the group treated with levodopa and patching improved 0.6 and 0.2 logMAR lines in placebo and patching group, respectively.
Likewise, Sofi et al. [25] compare the efficacy of levodopa versus placebo plus occlusion therapy in 50 patients between 5 and 20 years old. As a conclusion, visual acuity improved in both groups but more in the group treated with levodopa. For that reason, they concluded that levodopa-carbidopa can be used as an adjunct to conventional occlusion therapy in amblyopia, particularly, in older children and in severe cases of amblyopia, and it is well tolerated.
3.4. Perceptual Learning
Perceptual learning is another treatment for children and adults with amblyopia. Patients are often trained on contrast sensitivity tasks with occlusion of the non-amblyopic eye. Perceptual tasks are conducted with the Cambridge Visual Stimulator (CAM), a technology from the 1970s using a rotating disc on which high-contrast sine-wave gratings of six different spatial frequencies are displayed. The first grating used is the finest on which the patient can distinguish the orientation of the stripes. After some training, the grating frequencies are being increased, while the visual acuity is improved [26,27].
The use of perceptual learning was fairly limited, some studies such as Willshaw et al. [28], in 1980, showed a visual acuity improvement in children with no previous amblyopia treatment and also in those whose previous occlusion therapy had failed. After 4 weeks of completion of treatment, 47 patients were followed-up and 18 of them failed to maintain their visual acuity improvement. This fact brings to light the lack of sustained effects and long-term follow-up using CAM as a treatment. On the other hand, other authors as Tytla and Labow-Daily in 1981 compared a control group undergoing the same procedure without the grating stimulation and a group of patients who followed the CAM treatment [29]. They concluded that the improvements were not significantly different and the vision changes could be attributed to the short-term occlusion.
Recently, an adaptative optics perceptual learning (AOPL) system has been used to measure and correct the high order aberrations in amblyopic eyes [30]. According to a study carried out by Liao et al. [31], adaptative correction may improve the optical qualities of amblyopic eyes.
In addition, two different types of perceptual learning have shown to be effective in clinical research: Gabor’s patches and letter optotypes by training monocularly [32]: Gabor’s patches are based on the spatial frequency and orientation of a sinusoidal gratings with a Gaussian envelope where orientation discrimination is worked [33,34]. Moreover, letter optotypes are based on the fact that letter recognition is affected by crowding and interaction contours in amblyopia, thus training with letter recognition with and without crowding and orientation discrimination is carried out [35].
Recently, a neuro-modulatory technique, high-frequency transcranial random noise stimulation (hf-tRNS), had been developed and combined with perceptual learning. In a pilot study of Campana et al. [36] and a study of Moret et al. [37], participants underwent 8 training sessions during a period of 2 weeks combining perceptual learning and hf-tRNS showing a VA improvement in patients with amblyopia; in the pilot study, the mean VA improvement was 0.18 logMAR [37], while in the latest study, the mean VA improvement was 0.19 logMAR in the hf-tRNS group [37]. These results are quite positive compared with the results obtained by Polat et al. [34] using only Gabor’s patches for more weeks.
The boredom associated with repetition of a perceptual task over many hours, the dedicated time required for treatment, and need of training systems have limited the use of perceptual learning. An important drawback of this treatment is that the improvements are specific to the trained task and do not transfer easily to novel tasks. Duration of training depends on the severity of the amblyopia without a rule about the specific treatment time required [38]. Another limitation of perceptual learning is the small number of participants in the studies carried out and the lack of sustained effects and long-term follow-up [28]. Consequently, technological improvements have developed new binocular treatments with video games and movies.
4. Modern Treatments
The interest and the technological improvements had been developing different treatments for amblyopic patients. Use of interactive devices have been a topic of interest among researchers and clinicians. The aim of binocular treatment is to not only improve visual acuity of the amblyopic eye but also restore binocular fusion and stereopsis. Dichoptic treatment is based on the fact that visual tasks can only be solved if both eyes are working together [39].
Currently, there are different ways to improve the visual acuity of the amblyopic eye using videogames or movies. Some of them use red-green anaglyphic glasses, another shutter glasses, others polarized glasses, and another a low-pass filtering that decrease luminance in the fellow eye. The most known binocular treatments are developed below.
4.1. Dig Rush
Dig Rush, an action-oriented adventure game, is played on iPad® (Apple® Inc) with a touch-sensitive screen while the patient wears red-green anaglyphic glasses. The game consists in miners digging for gold. The patient has to use a finger to manipulate both miners and their surroundings to dig for gold and return it to a cart as quick as possible while avoiding obstacles such as fire, lava, and monsters [40]. There are 42 levels increasing in difficulty and the patient can earn up to three stars per level (maximum star count, 126). Gold can be used to purchase more miners and digging tools, as well as to dig faster and carry more gold.
The game is played while the patient is wearing red-green anaglyphic glasses that separate game elements seen by each eye. Reduced contrast elements (e.g., gold and fire) are seen by the fellow eye, high-contrast elements (e.g., miners and monsters) are seen by the amblyopic eye, and high-contrast background elements (e.g., ground and rocks) are seen by both eyes (Figure 1).

Figure 1. Illustration of Dig Rush. High-contrast red elements (miners and fireball) are seen by the amblyopic eye. Low-contrast blue elements (gold and platforms) are seen by the fellow eye. Gray elements (rocks and ground) are seen by both eyes.
In order to succeed playing the game, both eyes must see their respective game components. Amblyopic eye contrast remained at 100% contrast, while fellow eye contrast started at 20% but increased with game success (a star earned) or decreased if game play was not successful. This makes the amblyopic eye works hard together with the fellow eye.
4.2. Falling Blocks
This is one of the renowned games for binocular treatment. The game was played using an iPod Touch device at the patient’s habitual reading distance while wearing red-green anaglyphic glasses over an appropriate refractive correction. When the amblyopic eye looked through the green filter, only green elements were seen by this eye. In the same way, the fellow eye could see red elements when looked through the red filter. In addition, there were brown elements, which were seen by both eyes. Game elements were presented at 100% to the amblyopic eye and at lower contrast to the fellow eye. Binocular combination was required to successfully play the active video game. Thereby, contrast in the fellow eye was increased, as long as the performance was successful [43].
4.3. I-BiT
A variant modality of amblyopia therapy is interactive binocular treatment (I-BiT™). I-BiT™, developed by the Nottingham team [48], is based on three different mechanisms: first, by presenting fine and movable stimulus to the amblyopic eye and the fixed targets or background to the dominant eye; second, by showing the half of one image to each eye simultaneously; and third, by demonstrating identical images to both eyes with small retinal disparity. Binocular fusion is guaranteed thanks to the simultaneous stimulus presentation to both eyes. This system gives the possibility of adjusting its illumination and image contrast according to the patient’s visual acuity. During the treatment, the participant wore a shutter glasses, which lighten and darken in synchrony with the monitor but faster than the user can perceive. This allows a common background to be presented to both eyes and an “enriched” image to be presented only to the amblyopic eye, i.e., dichoptic stimulation.
4.4. Occlu-Pad or Occlu-Tab
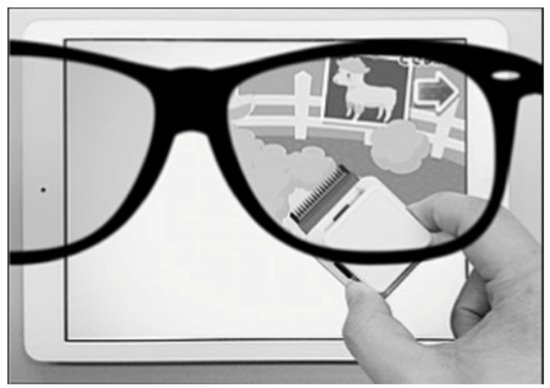
Occlu-pad is a device that processes images presented selectively to the amblyopic eye under open binoculars. Occlu-pad uses white-screen technology and polarized glasses. The white-screen technology involves peeling off the polarizing film layer of a liquid crystal panel of an iPad, and, by attaching this peeled film to glasses, viewing videos is only possible when the subject is wearing the polarized glasses. For example, if the film is attached to the right-eye lens of glasses, the subject can view the image only in the right eye (Figure 3). During training using the Occlu-pad, the patient played an arbitrary game requiring eye-hand coordination [51]. In Japan, this device is named “Occlu-pad” but outside Japan, it is named “Occlu-tab” [52].
4.5. Vivid Vision
Last but not least, mention the computer game called Diplopia Game (Vivid Vision, San Francisco, CA, USA), which was run in the Oculus Rift OC DK2 virtual reality head mounted display (Oculus VR) [55]. At first, two games were available, i.e., a space game, in which subjects were flying spaceship through a system of rings, and a breaker game, which is a typical block breaker game, but played in a virtual reality 3D setting. Next, they incorporated Hoopie, a game where the aim is to catch or refuse some objects using the hoop, and Bubbles, where the objective of the game is pop the floating bubbles in order from closest to farthest away. As some objects are seen with the amblyopic eye and others are seen with the fellow eye, the game forces the brain to use both eyes together (Figure 4).

4.6. Movies
It is clear than not all the patients know how or want to play video games, and moreover, some patients are so amblyopic that it is not possible to play video games. Passive dichoptic movies are a good alternative in those cases.
A digital mask composed of irregularly shaped blobs is applied on the images seen by the amblyopic eye, and an inverse mask was applied to the images seen by the fellow eye. So, the procedure is based on the presentation of complementary images in the two eyes while the patient wears polarized glasses. Thus, to perceive a completed coherent picture, it is necessary to combine information seen by both eyes. The shape and location of the blobs vary dynamically every 10 s. The contrast of the image seen by the amblyopic eye is fixed to its maximum, and the contrast of the image seen by the fellow eye is based on the results of the binocular balance contrast sensitivity baseline measure. If the subject perceives the full picture of the movie during a session, the contrast in the fellow eye was increased for the next session.
This entry is adapted from the peer-reviewed paper 10.3390/vision5020031
