COVID-19 has disrupted normal life and has enforced a substantial change in the policies, priorities and activities of individuals, organisations and governments. These changes are proving to be a catalyst for technology and innovation. In this entry, we discuss the pandemic's potential impact on the adoption of the Internet of Things (IoT) in healthcare. Our perspective and forecast of this impact on IoT adoption is based on a thorough research literature review, a careful examination of reports from leading consulting firms and interactions with several industry experts. For each of these sectors, we also provide the details of notable IoT initiatives taken in wake of COVID-19. We also highlight the challenges that need to be addressed and important research directions that will facilitate accelerated IoT adoption.
- COVID-19
- internet of things
- healthcare
1. Introduction
The Internet of Things (IoT) is envisioned as a network of billions of devices that can sense, communicate and share data which can then be analyzed to unlock a wealth of intelligence useful for planning, management, and decision making [1]. IoT promises huge benefits for healthcare. Despite the popularity of the IoT concept and its promised benefits, its adoption has been significantly slower than expected [2][3]. Some of the major reasons behind this include: 1) security, privacy, policy, and trust issues [3][4][5]; 2) organisational inertia, long capital cycles and shortage of specialist workforce needed to successfully implement IoT [2][5]; and 3) lack of convincing use cases with clear return on investment (ROI) in some sectors.
COVID-19 has impacted all walks of life so much that we may never return to the old normal. This pandemic is proving to be a catalyst for digital transformation because COVID-19 has created or expanded applications and use cases of digital technologies [6][7][8]. It has also forced governments, organisations and individuals to change/adapt their priorities, their views on societal/ethical issues, and the way they operate. In many cases, this has addressed or mitigated many of the above mentioned reasons behind the slower-than-expected adoption of IoT across many verticals. For example, governments have invested huge amount of resources in IoT and other technologies to combat COVID-19. Lifestyle changes brought about by COVID-19 such as work/study from home have also provided new use cases of IoT with clear ROI such as remote asset control, workforce tracking and remote employee collaboration [9]. Consequently, many organisations have increased investment in IoT and the pace of their IoT projects [10][11]. Also, the fight against COVID-19 has resulted in less strict stance on privacy issues, higher trust in technology and fast-tracked approval procedures. This is also paving the way for accelerated adoption of IoT in healthcare.
In this entry, we discuss the potential impact of COVID-19 on the adoption of IoT in healthcare. To this end, we have extensively analyzed recent relevant research literature and examined existing reports from Gartner, Yole, McKinsey and other consulting firms. We find that COVID-19 has not necessarily positively impacted the adoption of IoT in all aspects, at least in the short-term. Therefore, we discuss both the short-term and mid-to long-term impact of COVID-19 on IoT adoption in healthcare. We also discuss new initiatives that are being taken, challenges that need to be addressed, and important research directions that will facilitate IoT adoption.
2. Related Work
In the past year or so, numerous studies have discussed key potentials of IoT and other digital technologies in the fight against COVID-19 or future pandemics. Authors in [12] present a survey of IoT-based solutions used to fight COVID-19. Researchers in [13] analyse the effect of this pandemic on various technologies and discuss their social impacts. A detailed review of digital health solutions used in countries with high COVID-19 cases is presented in [14]. A consensus of Chinese experts on IoT-aided diagnosis of COVID-19 and its treatment is presented in [15]. Impacts of IoT implementation in healthcare in terms of cost, time and efficiency are enlisted in [16]. Applications of IoT, Big Data, Artificial Intelligence (AI) and Blockchain in mitigating the impact of COVID-19 are explored in [17]. Another research article [18] proposes some IoT applications that can be useful to combat COVID-19. [19] discuss how different industry 4.0 technologies (e.g., AI, IoT, Virtual Reality, etc.) can help reduce the spread of disease. Applications of AI for COVID-19 have been proposed in [20]. A comprehensive review of the COVID-19 pandemic and the role of IoT, drones, AI, blockchain, and 5G in managing its impact is explored in [21]. [22] argue that contact tracing should be the responsibility of facilities and propose a contact tracing architecture which is fully automated and does not depend on user cooperation. [23] discuss several IoT healthcare applications during three main phases: early diagnosis, quarantine time, and after recovery. A recent survey [24] discusses the use of Machine Learning (ML), AI and other intelligent approaches for the prognosis of COVID-19.
Potential IoT-based solutions to combat COVID-19 have been compiled in [25]. They present a detailed study on the capabilities of existing IoT systems at different layers such as perception layer, network layer, fog layer and cloud layer. Moreover, they also discuss applications of IoT in diagnosing symptoms of COVID-19. A four-layered architecture based on IoT and Blockchain technologies has been proposed in [26] to help fight against COVID-19. The Blockchain-based method is proposed to ensure privacy and security of physiological information shared among IoT nodes. It also enlists various applications that have been developed for detecting and tracing potential COVID-19 patients. The role of IoT in existing digital healthcare infrastructure has been discussed in [27]. It also debates on the implications of data generated through IoT enabled healthcare infrastructure on the decisions made by policy makers. Moreover, existing enablers and barriers in adopting IoT-based healthcare have also been enlisted.
A detailed survey on the contributions of IoT in healthcare in response to COVID-19 is provided in [28]. This is a detailed study enlisting recent developments in Healthcare IoT (HIoT). It also outlines comparison of different implementation strategies for IoT systems before and during this pandemic. [29] present a survey enlisting early efforts for the adoption of digital technologies in healthcare to fight against COVID-19, considering different categories such as diagnosis, prevention and surveillance. [30] emphasize the dire need of using AI techniques to combat future pandemics. They also highlight the limitations of the existing AI-based approaches towards eradication of the pandemic. Finally, they conclude that there is a need to use data science in global health to produce better predictions helpful for policy makers. A comparison of adoption of digital technologies in some specific regions of the world is provided in [7].
The entry highlights that COVID-19 has acted as a catalyst for adoption of e-Health, e-Education and e-Commerce. [31] present an analysis of how AI and IoT can be potentially used to fight against the COVID-19 pandemic.
3. Impact of COVID-19 on IoT and New Initiatives
COVID-19, as a macroeconomic shock, has impacted not only individual behaviours but has also enforced governments and organisations to change their policies and priorities. This is fueling the adoption of IoT and other technologies in many areas especially in healthcare.
In this section, we discuss the potential impact of COVID-19 on IoT adoption in healthcare. We also discuss the most notable recent initiatives taken in healthcare in the wake of COVID-19. We also set alerts on Google Scholar so that we do not miss recently published papers. Furthermore, we carefully examined reports from leading consulting firms such as Gartners, Yole and McKinsey as well as relevant articles/reports from reputable online sources. However, while our perspective and forecast on the impact of COVID-19 on healthcare presented in this article is often inspired by our interactions with these experts, we support the claims by citing relevant research papers, reports or articles wherever necessary.
3.1 Healthcare
COVID-19 is a healthcare crisis and hence the immediate impact on healthcare is more obvious. A study from Juniper Research found that IoT platform revenue is expected to increase by around 20% in 2020, reaching $66 billion in 2020 from $55 billion in 2019, mainly due to its accelerated adoption in healthcare sector [32]. Three main themes are accelerating IoT adoption in healthcare sector as detailed next.
3.1.1 Wearable Devices:
While wearables, such as smart watches, smart bands and finger rings, have been around for several years, COVID-19 has triggered a huge increase in their demand. Wearables can play vital roles in fighting against COVID-19 and other future pandemics [33]. For example, the data from wearable devices can be used to alert the users when changes in their metrics match with those associated with COVID-19 or other diseases [34]. The wearable devices can also be used for broadcasting health knowledge [35], providing capabilities for tracking and contact tracing [36], ensuring social-distancing [35], and providing mental healthcare [37] by tracking an individual’s cognition and mood in real-time, thus, enabling personalised interventions [38]. These and other similar applications are boosting the demand of wearables. Papa et al.[39] provide insights as to how the smart wearables would bring a revolution in healthcare. Research by GlobalData [40] estimates that the market for wearables is now on track to increase from being worth nearly $27 billion in 2019 to a whopping $64 billion by 2024. Next, we briefly discuss some recent relevant success stories in the fight against COVID-19.
WHOOP Inc. in collaboration with some leading research organizations has developed a COVID-19 identification system based on their WHOOP strap which measures respiratory rate using Resting Heart Rate (RHR) and Heart Rate Variability (HRV). The data from WHOOP strap is communicated to a mobile application and then forwarded to a cloud, collectively called WHOOP system [41] . Their system identified 20% of COVID-19 positive individuals in the two days prior to symptom onset, and 80% of COVID-19 positive cases by the third day of symptoms. Philips has also developed disposable patches for early detection of COVID-19 patients [42] and disposable biosensors for early COVID-19 patient deterioration detection [43] which measure and transmit various predictors of deterioration such as respiratory rate, heart rate, activity level, posture and ambulation etc.
Researchers from MIT and Harvard University investigated whether COVID-19 subjects could be accurately discriminated only from a forced-cough cell phone recording using AI [44]. Their results are based on cough recordings of over 5000 subjects and demonstrate that their model discriminates officially tested COVID-19 subjects 97.1% accurately, with a 100% asymptomatic detection rate. In the past, cough recordings had also been used to accurately diagnose conditions such as pneumonia and asthma [45]. This shows the potential of integrating such solutions in wearables to enable a non-invasive, real-time solution for disease diagnosis, pre-screening and outbreak monitoring.
The Scripps Research Translational Institute has conducted a study named DETECT (Digital Engagement & Tracking for Early Control & Treatment) that collects data from smartwatches and activity trackers of consenting partners as well as self-reported symptoms and test results [46]. They recently reported [47] that the data from wearable devices along with self-reported symptoms can be used for identifying cases of COVID-19 with greater success than looking at symptoms alone. To help combat COVID-19, many other similar studies [48][49][50][51][52] have accelerated deployment to allow interested individuals to voluntarily share their sensor and clinical data.
3.1.2. Changes in Regulations and Procedures
In the past, the adoption of IoT in healthcare had been slower than expected due to regulatory policies related to privacy, data security and approval procedures. In response to COVID-19, emergency regulations are being adopted using fast-tracked procedures and many new technologies have been given emergency approvals, which is accelerating IoT adoption. For example, U.S. Food and Drug Administration (FDA) has issued an Emergency Use Authorization certificate to the electrocardiogram low ejection fraction tool developed by Eko, a digital health company, to help clinicians assess cardiac complications associated with COVID-19 [53]. Handheld and portable ultrasound solutions in particular have become valuable tools for clinicians treating COVID-19 patients due to their imaging capabilities, portability and ease of disinfection. Philips has received clearance from FDA for Lumify, a portable ultrasound device [54]. Lumify has a transducer which needs to be connected with the user’s smartphone running Lumify application. Moreover, FDA has also allowed Aidoc (a technologycompany) to use their AI-CT algorithms for COVID-19 detection [55].
The World Health Organisation (WHO) has warned of the risk of infections in crowded hospitals and emergency rooms [56]. Consequently, regulatory response to minimise hospital and clinic visits has accelerated the adoption of telehealth and homecare. For example, many countries are encouraging the use of telehealth services and have added various types of medical services on their public health programs (e.g., Medicare Australia) that can now be accessed via telehealth [57]. The sharp increase in the use of telehealth is encouraging the adoption of IoT and related technologies in healthcare sector. Analysis on the relationship between IoT technologies, smart telemedicine diagnosis systems, and virtual care for different age, race/ethnicity, gender, education, and geographic regions is presented in [58]. Similar analysis is performed in [59][60] for AI, Internet of Medical Things (IoMT) and Big Data enabled healthcare for monitoring, detection and prevention of COVID-19. Recently, a novel IoMT platform has been proposed for remote health monitoring offering emotional treatment suggestion to the doctors and patients [61]. A detailed analysis of contactless health services in pre-, during-, and post-pandemic periods can be found in [62]. The study predicts that hybrid healthcare services would emerge in the post-COVID-19 era, potentially with new advances due to the accelerating technological development.
There are various other changes in regulations and procedures that are accelerating the adoption of IoT. For example, to combat COVID-19, some countries have introduced confinement measures and tracking of COVID-19 patients using GPS, bracelets or other technological tools [63]. Furthermore, many countries have introduced new regulations including stricter cleaning requirements [64] and record keeping requirements for contact tracing [65]. This has led to the deployment of robots for efficient and effective disinfection [66][67][68][69] as well as technology-assisted record keeping and visitor tracking/monitoring [70][71].
3.1.3. IoT for Test and Trace
IoT-enabled testing and tracing of COVID-19 can reduce the transmission which is critical in the fight against this pandemic. Therefore, IoT is now being extensively used for test and trace applications which is accelerating IoT adoption [72]. For example, see [73] which provides an analysis of 13 technologies, to monitor users with COVID-19 symptoms, that can be used by governments and other organisations to combat COVID-19 and future pandemics. A large number of countries and regions have adopted digital test and trace efforts, including UK, South Korea, Germany, Spain, Vietnam, Taiwan, etc. [74][75]. While some of these efforts have not been very successful in tracing COVID-19, the countries that have extensively used technology in their solutions have done much better in their fight against this pandemic. For example, it was reported in [76] that UK’s test and trace system employing around 27,000 contact tracers was not able to reach 21% of the people who were tested positive in the week of 2 July to 8 July 2020. Moreover, the 79% of the people who were reached identified 13,807 close contacts but only 71% of these contacts were reached and asked to self-isolate. On the other hand, Taiwan had better systems in place (due to the lessons learned from the 2003 SARS outbreak) and was successful in curbing the first COVID-19 wave mainly due to quick and effective policy decisions and extensively using digital technologies [77]. Despite Taiwan’s initial success, there has been a surge of COVID-19 cases in Taiwan recently which is attributed to the lax adherence to safety protocols, fewer tests (around 13 total tests performed per thousand people as of 21 May 2021, in contrast, US has conducted around 1322 tests per thousand people [78]) and slow vaccine roll out (only 1.26% of the population has received a COVID-19 vaccine as of 21 May 2021 [78]). This shows that an advanced technology-based test and trace system can only be an effective tool to fight against the pandemic if all other safety protocols are also followed and strict policy decisions are enforced.
Figure 1 shows an architecture diagram for a test and trace system similar to the solution employed by Taiwan. There are mainly two layers of such advanced test and trace system, namely Data Acquisition and Data Integration.
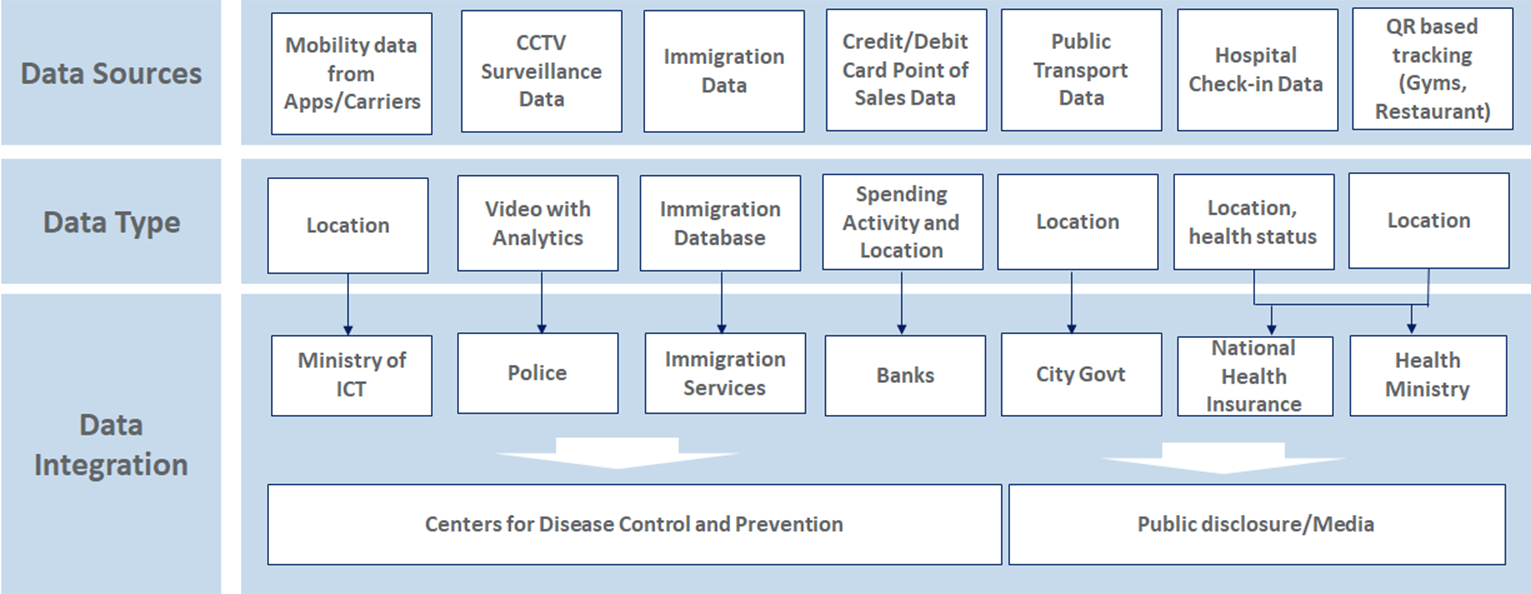
Figure 1. An Example of a Test and Trace IoT Architecture
Data Acquisition: Mobility data is acquired from multiple sources including immigration department database, GSM and GPS based mobile phone tracking, and QR code based tracking and so forth. This helps Taiwan in tracking international as well as local travellers. Resources from smart city are also utilized including CCTV cameras based surveillance [79]. Credit card based payments are also detected and tracked to locate users and predict their activities [80]. Similarly, hospital visits of the individuals are also recorded and tracked to help contact tracing [81].
Data Integration: In this layer, the data from different sources are integrated and shared with the relevant departments [82]. For example, the immigration database and National Health Insurance (NHI) database are shared with the Centers for Disease Control and Prevention [77]. Location information is shared with local authorities. For example, surveillance data from smart city setup is shared with police officers for necessary actions [77]. Data extracted from certain sources such as public transport and shopping malls is also shared with public to help them make informed decisions about their daily routines [83].
4. Challenges and Key Research Directions
COVID-19 has brought about opportunities as well as many real challenges forIoT adoption. From a macro perspective, IoT adoption needs to cater to the profound societal and economic changes caused by COVID-19. Since the beginning of the global pandemic, behaviors of individuals, communities and organisations have undergone a major shift [84]. Moreover, some of this shift will not be restored in the next few years or even beyond that. The focus of social construction is on well-being during the pandemic and in post-pandemic world. In the context of financial constraints, IoT adoption must be more effective, efficient, purposeful, and have a significant ROI.
From a micro perspective, IoT technology requires faster and more revolutionary innovation to ensure the functioning of society, promote civil construction, and respond to possible crises in the future. The global IoT market was growing before the pandemic, but some of its shortcomings have been magnified during the pandemic such as the ease and economy of device installation and data security. New specific problems are emerging in healthcare and effective IoT solutions for these problems will be the key in accelerated IoT development and adoption in healthcare.
In this section, we discuss challenges as well as key research directions in IoT for healthcare. We also discuss key research directions important to facilitate and accelerate IoT adoption in healthcare.
COVID-19 has made it even more important for healthcare to be ubiquitous, low threshold, and more efficient in monitoring, testing and diagnosis. This brings about many new challenges. First, ubiquity means that IoT-based medical services must be available on-demand and accessible to a wider population. However, most people do not own professional medical equipment, whereas more affordable devices such as smartphones and wearables have limited capabilities in healthcare. Second, the low threshold requires reducing the cost and difficulty of using IoT-based medical services. However, medical service processes are typically complicated and expensive. Moreover, many people find it hard to adopt and use new technologies such as IoT systems for healthcare. Third, it is important to address energy requirements and computational efficiency of healthcare sensors, e.g., to enable continuous monitoring and high-quality testing/diagnosis. Based on these challenges, below we enumerate some promising R&D directions for healthcare IoT.
4.1. Financial Constraints
A large number of companies, organisations and individuals are facing financial stress which is one key factor negatively affecting IoT adoption. Many organisations have reduced or stopped altogether their investment on many new or planned initiatives such as IoT projects. Another financial challenge caused by COVID-19 is the increasing labor costs for device installation under social contact restrictions.
A key challenge that needs attention is to reduce the cost of IoT system development, installation, and usage. Convergence of IoT and cloud services is important, making the IoT infrastructure that is heavily related to geographic space a virtualized and sustainable resource. Furthermore, open source IoT data processing software, analytics tools and testbeds need to be developed to enable organisations to avoid/reduce the cost of outsourcing or developing these in-house.
It has become ever more important to develop IoT sensors and devices that are cheap and easier to install and maintain. For example, it is important to invent devices that operate on minimal power [85] as this can reduce the maintenance cost, i.e., replacing batteries. One such example is the Ultra Low Power SoC for battery powered IoT devices [86], developed by Dialog Semiconductor, which can provide more than one year battery life for many IoT applications. It is also critical to develop cheap plug-and-play sensing devices [87][88] that can be easily integrated into ordinary facilities without additional hardware investment and deployment cost. It will also be helpful to explore self-configuration and self-adaptation of IoT devices [89] as well as intelligent human-computer interaction [90] to ease the installation and usage of IoT systems.
4.2. Data Security and Privacy
Many countries have introduced various emergency regulations during the pandemic such as limits on people’s movements, social distance requirements and less strict privacy obligations [91]. Once the pandemic is over, such regulations will need to be carefully reviewed to ensure people’s rights and privacy are protected [64]. In order to be better prepared for future pandemics and emergencies, the research community needs to work on robust data access policies, security protocols and privacy-preserving solutions for tracking, monitoring and analytics etc. Also, instead of conventional data centers, decentralized data pools at personal devices may be considered to give more control to the end users over their own data. IoT sensors do not actively collect and upload data but transfer the created data to user devices. Users can choose to distribute data peer-to-peer to their trusted users or third-party applications for data analysis and decision-making. Moreover, lightweight but reliable encryption and network transmission technology are needed for personal devices. The solution should be efficiently integrated with emerging technologies such as 5G, edge computing, and Blockchain [92].
4.3 Upgraded Wearable Technology
There is a need to make wearables more comfortable to wear/carry. Some recent studies [93][94] have pointed out that the product design of wearables should be optimized for different groups with different lifestyles and circumstances. For example, to adapt to the needs of patients with respiratory diseases, Ruth et al. [95] incorporate an optical sensor array into a wearable face mask for continuous cardiovascular monitoring. There is also a need to develop energy harvesting sensors for wearables since smart algorithms on wearables can drain its battery quickly. Therefore, energy harvesting technology utilizing thermometric principle can be applied to wearables, e.g., Kim et al. [96] demonstrate the feasibility of operating a commercial glucose sensor using only the body heat as its energy source.
4.4 AIoT (AI + IoT) for Healthcare
Algorithms currently running on off-the-shelf IoT devices (e.g., smartphones and wearables) must be able to provide quality comparable to medical grade equipment [97]. In the recent years, AI for healthcare has achieved remarkable progress in screening, disease diagnosis, and telemedicine, using machine learning models driven by massive health data [98]. It is important to accelerate the integration of IoT and AI for healthcare. However, one urgent issue to solve is the model training and deployment on IoT devices that have limited computational and memory resources. There are preliminary works in this direction. Zhuang et al. [99] discuss the split AI architecture for mobile healthcare systems, where lightweight AI solutions can work locally on the client side. Liu et al. [100] present a multi-task convolutional network on an ARM CPU to enable real-time cardiovascular and respiratory measurement based on mobile videos. However, there are preliminary efforts and more work is needed in this direction.
4.5 Making Health Services More Accessible
People may be unwilling or unable to invest in specialized medical devices or wearables. To make healthcare services accessible to a wider population, a multi-faceted approach is needed. For example, there is a need to establish community-based un-manned clinics [101]. Similarly, it is important to develop low-cost and self-help medical solutions that work on off-the-shelf devices such as smartphones and home audio systems. A recent survey [37] found that most existing studies rely on expensive research-grade wearable devices and there is a need to replace these research-grade wearables with the current smartwatches. Some recent breakthroughs in making health services more accessible include COVID-19 screening using cough recording [44], smartphone-based capture and interpretation of Rapid Diagnostic Tests [102], and on-device vitals measurement [100].
This entry is adapted from the peer-reviewed paper 10.3390/s21113838
References
- Patel, KK; Patel, SM; Internet of things-IOT: definition, characteristics, architecture, enabling technologies, application & future challenges. International Journal of Engineering Science 2016, 6, 6122-6131, .
- . What’s new with the Internet of Thing . Mckinsey. Retrieved 2021-6-23
- Farhan, L.; Shukur, S.T.; Alissa, A.E.; Alrweg, M.; Raza, U.; Kharel, R. A survey on the challenges and opportunities of theInternet of Things (IoT). In Proceedings of the 2017 Eleventh International Conference on Sensing Technology (ICST), Sydney,NSW, Australia, 4–6 December 2017; pp. 1–5.
- Lin, D.; Lee, C.; Lin, K. Research on effect factors evaluation of internet of things (IOT) adoption in Chinese agricultural supplychain. In Proceedings of the 2016 IEEE International Conference on Industrial Engineering and Engineering Management (IEEM),Bali, Indonesia, 4–7 December 2016; pp. 612–615.
- Jalali, M.S.; Kaiser, J.P.; Siegel, M.; Madnick, S. The Internet of Things Promises New Benefits and Risks: A Systematic Analysis of Adoption Dynamics of IoT Products. IEEE Secur. Priv.2019,17, 39–48
- Renu, N. Technological advancement in the era of COVID-19.Sage Open Med.2021,9, 20503121211000912.
- El Kadi, T.H. Uneven Disruption: COVID-19 and the Digital Divide in the Euro-Mediterranean Region. InIEMed MediterranianYearbook; 2020. Available online: https://www.iemed.org/observatori/arees-danalisi/arxius-adjunts/anuari/med.2020/Digital_Divide_Euro-Mediterranean_Covid-19_Tin_Hinane_El-Kadi_IEMed_YearBook2020_.pdf (accessed on 30 May 2021).
- Anderson, C.; Bieck, C.; Marshall, A. How business is adapting to COVID-19: Executive insights reveal post-pandemicopportunities.Strategy Leadersh.2020, doi:10.1108/SL-11-2020-0140.
- Fahrni, S.; Jansen, C.; John, M.; Kasah, T.; Koerber, B.; Mohr, N. Coronavirus: Industrial IoT in Challenging Times. Availableonline: https://www.mckinsey.com/industries/advanced-electronics/our-insights/coronavirus-industrial-iot-in-challenging-times (accessed on 30 May 2021).
- Stahie, S. COVID-19 Pandemic Increased IoT Adoption, Research Finds. Available online: https://www.bitdefender.com/box/blog/iot-news/covid-19-pandemic-increased-iot-adoption-research-finds/ (accessed on 30 May 2021).
- O’Halloran, J. Nearly Half of Firms to Increase Investments in IoT Despite the Impact of COVID-19. Available online: https://www.computerweekly.com/news/252491333/Nearly-half-of-firms-to-increase-investments-in-IoT-despite-the-impact-of-Covid-19 (accessed on 30 May 2021).
- Elansary, I.; Darwish, A.; Hassanien, A.E. The Future Scope of Internet of Things for Monitoring and Prediction of COVID-19 Patients. InDigital Transformation and Emerging Technologies for Fighting COVID-19 Pandemic: Innovative Approaches; Springer:Cham, Switzerland, 2021; pp. 235–247.
- Brem, A.; Viardot, E.; Nylund, P.A. Implications of the coronavirus (COVID-19) outbreak for innovation: Which technologies willimprove our lives? Technol. Forecast. Soc. Chang.2021,163, 120451.
- Kalhori, S.R.N.; Bahaadinbeigy, K.; Deldar, K.; Gholamzadeh, M.; Hajesmaeel-Gohari, S.; Ayyoubzadeh, S.M. Digital Health Solutions to Control the COVID-19 Pandemic in Countries With High Disease Prevalence: Literature Review.J. Med. Internet Res.2021,23, e19473.
- Bai, L.; Yang, D.; Wang, X.; Tong, L.; Zhu, X.; Zhong, N.; Bai, C.; Powell, C.A.; Chen, R.; Zhou, J.; et al. Chinese experts’ consensus on the Internet of Things-aided diagnosis and treatment of coronavirus disease 2019 (COVID-19).Clin. eHealth2020,3, 7–15.
- Singh, R.P.; Javaid, M.; Haleem, A.; Suman, R. Internet of things (IoT) applications to fight against COVID-19 pandemic. Diabetes Metab. Syndr. Clin. Res. Rev.2020,14, 521–524.
- Ting, D.S.W.; Carin, L.; Dzau, V.; Wong, T.Y. Digital technology and COVID-19.Nat. Med.2020,26, 459–461.
- Rahman, M.S.; Peeri, N.C.; Shrestha, N.; Zaki, R.; Haque, U.; Ab Hamid, S.H. Defending against the Novel Coronavirus (COVID-19) Outbreak: How Can the Internet of Things (IoT) help to save the World?Health Policy Technol.2020,doi:10.1016/j.hlpt.2020.04.005.
- Javaid, M.; Haleem, A.; Vaishya, R.; Bahl, S.; Suman, R.; Vaish, A. Industry 4.0 technologies and their applications in fighting COVID-19 pandemic. Diabetes Metab. Syndr. Clin. Res. Rev.2020,14, 419–422.
- Vaishya, R.; Javaid, M.; Khan, I.H.; Haleem, A. Artificial Intelligence (AI) applications for COVID-19 pandemic. Diabetes Metab. Syndr. Clin. Res. Rev.2020,14, 337–339.
- Chamola, V.; Hassija, V.; Gupta, V.; Guizani, M. A Comprehensive Review of the COVID-19 Pandemic and the Role of IoT, Drones, AI, Blockchain, and 5G in Managing its Impact. IEEE Access2020,8, 90225–90265.
- Mokbel, M.F.; Abbar, S.; Stanojevic, R. Contact Tracing: Beyond the Apps.arXiv2020, arXiv:2006.04585.
- Nasajpour, M.; Pouriyeh, S.; Parizi, R.M.; Dorodchi, M.; Valero, M.; Arabnia, H.R. Internet of Things for current COVID-19 and future pandemics: An exploratory study.arXiv2020, arXiv:2007.11147.
- Nayak, J.; Naik, B.; Dinesh, P.; Vakula, K.; Rao, B.K.; Ding, W.; Pelusi, D. Intelligent system for COVID-19 prognosis: A state-of-the-art survey. Appl. Intell.2021,51, 2908–2938.
- Dong, Y.; Yao, Y.D. IoT Platform for COVID-19 Prevention and Control: A Survey.arXiv2020, arXiv:2010.08056.
- Alam, T. Internet of Things and Blockchain-based framework for Coronavirus (Covid-19) Disease.SSRN2020,doi:10.2139/ssrn.3660503 .
- Kelly, J.T.; Campbell, K.L.; Gong, E.; Scuffham, P. The Internet of Things: Impact and Implications for Health Care Delivery. J.Med. Internet Res.2020,22, e20135.
- Ndiaye, M.; Oyewobi, S.S.; Abu-Mahfouz, A.M.; Hancke, G.P.; Kurien, A.M.; Djouani, K. IoT in the Wake of COVID-19: A Survey on Contributions, Challenges and Evolution. IEEE Access2020,8, 186821–186839.
- Golinelli, D.; Boetto, E.; Carullo, G.; Nuzzolese, A.G.; Landini, M.P.; Fantini, M.P. Adoption of Digital Technologies in HealthCare During the COVID-19 Pandemic: Systematic Review of Early Scientific Literature. J. Med. Internet Res.2020,22, e22280.
- Chang, A.C. Artificial Intelligence and COVID-19: Present State and Future Vision. Intell.-Based Med.2020,3, 100012.
- Abir, S.; Islam, S.N.; Anwar, A.; Mahmood, A.N.; Oo, A.M.T. Building Resilience against COVID-19 Pandemic Using Artificial Intelligence, Machine Learning, and IoT: A Survey of Recent Progress.IoT2020,1, 506–528.
- Juniper Research.IOT Platform Revenue to Grow 20% in 2020, Despite Global COVID-19 Pandemic. Available online:https://www.juniperresearch.com/press/press-releases/iot-platform-revenue-to-grow-20-in-2020 (accessed on 30 May 2021)
- Sawyer, J. Wearable Internet of Medical Things Sensor Devices, Artificial Intelligence-driven Smart Healthcare Services, and Personalized Clinical Care in COVID-19 Telemedicine. Am. J. Med. Res.2020,7, 71–77.
- Seshadri, D.R.; Davies, E.V.; Harlow, E.R.; Hsu, J.J.; Knighton, S.C.; Walker, T.A.; Voos, J.E.; Drummond, C.K. Wearable sensors for COVID-19: A call to action to harness our digital infrastructure for remote patient monitoring and virtual assessments. Front. Digit. Health2020,2, 8.
- Waheed, A.; Shafi, J. Successful Role of Smart Technology to Combat COVID-19. In Proceedings of the 2020 Fourth International Conference on I-SMAC (IoT in Social, Mobile, Analytics and Cloud)(I-SMAC), Palladam, India, 7–9 October 2020; pp. 772–777.
- Lin, L.; Hou, Z. Combat COVID-19 with artificial intelligence and big data. J. Travel Med.2020,27, taaa080.
- Ueafuea, K.; Boonnag, C.; Sudhawiyangkul, T.; Leelaarporn, P.; Gulistan, A.; Chen, W.; Mukhopadhyay, S.C.; Wilaiprasitporn, T.;Piyayotai, S. Potential Applications of Mobile and Wearable Devices for Psychological Support During the COVID-19 Pandemic:A Review.IEEE Sens. J.2020, doi:10.1109/JSEN.2020.3046259.
- Sahakian, B.; Vatansever, D.; Wang, S. COVID-19 and promising solutions to combat symptoms of stress, anxiety and depression. Neuropsychopharmacology 2021, doi:10.1038/s41386-020-00791-9.
- Papa, A.; Mital, M.; Pisano, P.; Del Giudice, M. E-health and wellbeing monitoring using smart healthcare devices: An empirical investigation. Technol. Forecast. Soc. Chang.2020,153, 119226.
- Global Data. Wearable Tech market SET to Grow 137% by 2024 But Smartwatches to See a 10% Decline in Revenue This Year Due to Shipment Delays and Tighter Consumer Wallets. Available online: https://www.globaldata.com/wearable-tech-market-set-to-grow-137-by-2024-but-smartwatches-to-see-a-10-decline-in-revenue-this-year-due-to-shipment-delays-and-tighter-consumer-wallets-says-globaldata/ (accessed on 30 May 2021).
- Miller, D.J.; Capodilupo, J.V.; Lastella, M.; Sargent, C.; Roach, G.D.; Lee, V.H.; Capodilupo, E.R. Analyzing changes in respiratoryrate to predict the risk of COVID-19 infection. PLoS ONE2020,15, e0243693.
- FDA. FDA Clears Philips’ Disposable Patch for COVID-19 Patient Deterioration. Available online: https://www.fdanews.com/articles/print/197314-fda-clears-philips-disposable-patch-for-covid-19-patient-deterioration (accessed on 30 May 2021).
- O’Reilly, K. Philips Launches Next Generation Wearable Biosensor for Early Patient Deterioration Detection, Including Clinical Surveillance for COVID-19. Available online: https://www.philips.com/a-w/about/news/archive/standard/news/press/2020/20200526-philips-launches-next-generation-wearable-biosensor-for-early-patient-deterioration-detection-including-clinical-surveillance-for-covid-19.html (accessed on 30 May 2021).
- Laguarta, J.; Hueto, F.; Subirana, B. COVID-19 Artificial Intelligence Diagnosis using only Cough Recordings.IEEE Open J. Eng.Med. Biol.2020,1, 275–281.
- Porter, P.; Abeyratne, U.; Swarnkar, V.; Tan, J.; Ng, T.W.; Brisbane, J.M.; Speldewinde, D.; Choveaux, J.; Sharan, R.; Kosasih, K.;et al. A prospective multi-centre study testing the diagnostic accuracy of an automated cough sound centred analytic system for the identification of common respiratory disorders in children. Respir. Res.2019,20, 81.
- Radin, J.M.; Wineinger, N.E.; Topol, E.J.; Steinhubl, S.R. Harnessing wearable device data to improve state-level real-time surveillance of influenza-like illness in the USA: A population-based study. Lancet Digit. Health2020,2, e85–e93.
- Quer, G.; Radin, J.M.; Gadaleta, M.; Baca-Motes, K.; Ariniello, L.; Ramos, E.; Kheterpal, V.; Topol, E.J.; Steinhubl, S.R. Wearable sensor data and self-reported symptoms for COVID-19 detection. Nat. Med.2020,27, 73–77.
- Mishra, T.; Wang, M.; Metwally, A.A.; Bogu, G.K.; Brooks, A.W.; Bahmani, A.; Alavi, A.; Celli, A.; Higgs, E.; Dagan-Rosenfeld, O.;et al. Early detection of COVID-19 using a smartwatch.medRxiv2020, doi:10.1101/2020.07.06.20147512 .
- Natarajan, A.; Su, H.W.; Heneghan, C. Assessment of physiological signs associated with COVID-19 measured using wearabledevices.medRxiv2020,3, 1–8.
- Evidation. Evidation Health and BARDA Partner on Early Warning System for COVID-19. Available online: https://evidation.com/news/evidationhealthandbardapartner/ (accessed on 30 May 2021).
- Oura Health. UCSF Tem Predict Study. Available online: https://blog.ouraring.com/ucsf-tempredict-study/ (accessed on 30May 2021).
- Robert Koch Institut. Corona Datenspende. Available online: https://corona-datenspende.de/science/en/ (accessed on 30 May2021).
- Lovett, L. Eko Lands EUA for device that Helps Detect Coronavirus Patients with Cardiac Complications. Available online: https://www.mobihealthnews.com/news/eko-lands-eua-device-helps-detect-coronavirus-patients-cardiac-complications (accessed on 10 November 2020).
- Groves, M. Philips Receives FDA Clearance for the Use of Its Ultrasound Portfolio to Manage COVID-19-Related Lung and Cardiac Complications. Available online: https://www.philips.com/a-w/about/news/archive/standard/news/press/2020/20200513-philips-receives-fda-clearance-for-the-use-of-its-ultrasound-portfolio-to-manage-covid-19-related-lung-and-cardiac-complications.html (accessed on 10 November 2020).
- Applied Radiology. Aidoc’s AI-CT Algorithms FDA Cleared for COVID-19. Available online: https://www.appliedradiology.com/communities/CT-Imaging/aidoc-s-ai-ct-algorithms-fda-cleared-for-covid-19 (accessed on 10 November 2020).
- Barr, J.R.; D’Auria, D.; Persia, F. Telemedicine, Homecare in the Era of COVID-19 & Beyond. In Proceedings of the 2020 Third International Conference on Artificial Intelligence for Industries (AI4I), Irvine, CA, USA, 21–23 September 2020; pp. 48–51.
- Australian Government, Department of Health. Providing Health Care Remotely during COVID-19. Available online:https://www.health.gov.au/news/health-alerts/novel-coronavirus-2019-ncov-health-alert/coronavirus-covid-19-advice-for-the-health-and-disability-sector/providing-health-care-remotely-during-covid-19 (accessed on 30 May 2021).
- Clarke, G. Remote Treatment of Patients during the COVID-19 Pandemic: Digital Technologies, Smart Telemedicine Diagnosis Systems, and Virtual Care. Am. J. Med. Res.2020,7, 29–35.
- Hughes, A. Artificial Intelligence-enabled Healthcare Delivery and Real-Time Medical Data Analytics in Monitoring, Detection, and Prevention of COVID-19. Am. J. Med. Res.2020,7, 50–56.
- Davis, R. Integrating Digital Technologies and Data-driven Telemedicine into Smart Healthcare during the COVID-19 Pandemic. Am. J. Med. Res.2020,7, 22–28.
- Zhang, T.; Liu, M.; Yuan, T.; Al-Nabhan, N. Emotion-Aware and Intelligent Internet of Medical Things towards Emotion Recognition during COVID-19 Pandemic. IEEE Internet Things J.2020.
- Lee, S.M.; Lee, D. Opportunities and challenges for contactless healthcare services in the post-COVID-19 Era. Technol. Forecast. Soc. Chang.2021,167, 120712.
- OECD. Regulatory Quality and COVID-19: Managing the Risks and Supporting the Recovery. Available online: http://www.oecd.org/regreform/regulatory-policy/Regulatory-Quality-and-Coronavirus%20-(COVID-19)-web.pdf (accessed on 30May 2021).
- Australian Government, Department of Health. Environmental Cleaning and Disinfection Principles for COVID-19. Available online: https://www.health.gov.au/sites/default/files/documents/2020/03/environmental-cleaning-and-disinfection-principles-for-covid-19.pdf (accessed on 30 May 2021).
- Coronavirus (COVID-19) Victoria. Record Keeping for Contact Tracing—Information for Business. Available online: https://www.coronavirus.vic.gov.au/record-keeping-contact-tracing-information-business (accessed on 30 May 2021).
- Statt, N. Boston Dynamics’ Spot Robot Is Helping Hospitals Remotely Treat Coronavirus Patients. Available online: https://www.theverge.com/2020/4/23/21231855/boston-dynamics-spot-robot-covid-19-coronavirus-telemedicine (accessed on 10 November 2020).
- Guettari, M.; Gharbi, I.; Hamza, S. UVC disinfection robot.Environ. Sci. Pollut. Res.2020, doi:10.1007/s11356-020-11184-2
- Ackerman, E. Autonomous Robots Are Helping Kill Coronavirus in Hospitals. IEEE Spectr.2020. Available online: https://spectrum.ieee.org/automaton/robotics/medical-robots/autonomous-robots-are-helping-kill-coronavirus-in-hospitals (accessed on: 30 May 2021).
- Zeng, Z.; Chen, P.J.; Lew, A.A. From high-touch to high-tech: COVID-19 drives robotics adoption. Tour. Geogr.2020,22, 724–734.
- Ahmed, N.; Michelin, R.A.; Xue, W.; Ruj, S.; Malaney, R.; Kanhere, S.S.; Seneviratne, A.; Hu, W.; Janicke, H.; Jha, S.K. A survey ofCOVID-19 contact tracing apps. IEEE Access2020,8, 134577–134601.
- Xia, Y.; Lee, G. How to return to normalcy: Fast and comprehensive contact tracing of COVID-19 through proximity sensing using mobile devices.arXiv2020, arXiv:2004.12576.
- Russo, M.; Feng, T. Contact Tracing Accelerates IoT Opportunities and Risks. Available online: https://www.bcg.com/en-au/publications/2020/contact-tracing-accelerates-iot-opportunities-and-risks-2 (accessed on 30 May 2021).
- Ribeiro-Navarrete, S.; Saura, J.R.; Palacios-Marqués, D. Towards a new era of mass data collection: Assessing pandemic surveillance technologies to preserve user privacy. Technol. Forecast. Soc. Chang. 2021,167, 120681.
- Moon, J.; Chekar, C.K.; Barberá, D.; Davey, G.; Gaisser, S.; Gaisser, T.; Iwuji, C.; Meseguer, E.; Ryan, J.G.; Hopkins, M.M. Optimising ’Test and Trace’ Systems: Early lessons from a comparative analysis of six countries.SSRN2020, doi:10.2139/ssrn.3694441.
- Cao, H.L.; Nguyen, H.A.D.; Luu, T.H.; Vu, H.T.T.; Pham, D.; Le, H.H.; Nguyen, D.X.B.; Truong, T.T.; Nguyen, H.D.; Nguyen, C.N.; et al. Localized automation solutions in response to the first wave of COVID-19: A story from Vietnam. Int. J. Pervasive Comput.Commun.2020, doi:10.1108/IJPCC-10-2020-0176.
- O’Dowd, A. COVID-19: UK Test and Trace System Still Missing 80% Target for Reaching Contacts. BMJ, 2020, 370;m2875. DOI:https://doi.org/10.1136/bmj.m2875
- Lin, C.; Braund, W.E.; Auerbach, J.; Chou, J.H.; Teng, J.H.; Tu, P.; Mullen, J. Policy Decisions and Use of Information Technology to Fight Coronavirus Disease, Taiwan. Emerg. Infect. Dis.2020,26, 1506.
- Our World in Data. Available online: https://ourworldindata.org (accessed on 21 May 2021).
- Shorfuzzaman, M.; Hossain, M.S.; Alhamid, M.F. Towards the sustainable development of smart cities through mass video surveillance: A response to the COVID-19 pandemic. Sustain. Cities Soc.2020,64, 102582.
- Chen, C.M.; Jyan, H.W.; Chien, S.C.; Jen, H.H.; Hsu, C.Y.; Lee, P.C.; Lee, C.F.; Yang, Y.T.; Chen, M.Y.; Chen, L.S.; et al. ContainingCOVID-19 among 627,386 persons in contact with the diamond princess cruise ship passengers who disembarked in Taiwan: Bigdata analytics. J. Med. Internet Res.2020,22, e19540.
- Wang, C.J.; Ng, C.Y.; Brook, R.H. Response to COVID-19 in Taiwan: big data analytics, new technology, and proactive testing.JAMA2020,323, 1341–1342.
- Su, S.F.; Han, Y.Y. How Taiwan, a non-WHO member, takes actions in response to COVID-19.J. Glob. Health2020,10,doi:10.7189/jogh.10.010380.
- Zuo, F.; Wang, J.; Gao, J.; Ozbay, K.; Ban, X.J.; Shen, Y.; Yang, H.; Iyer, S. An interactive data visualization and analytics tool to evaluate mobility and sociability trends during COVID-19.arXiv2020, arXiv:2006.14882.
- Northumbria University Newcastle. 5 Ways Psychology Explains Our Changing Behaviour during the COVID-19 Pandemic. Available online: https://www.northumbria.ac.uk/study-at-northumbria/courses/msc-psychology-distance-learning-dtdppy6/social-psychology-coronavirus/ (accessed on 30 May 2021).
- Gulati, M.; Parizi, F.S.; Whitmire, E.; Gupta, S.; Ram, S.S.; Singh, A.; Patel, S.N. Cap Harvester: A Stick-on Capacitive Energy Harvester Using Stray Electric Field from AC Power Lines. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol.2018,2, 110:1–110:20, doi:10.1145/3264920.
- Dialog Semiconductor. DA16200: Ultra Low Power Wi-Fi SoC for Battery Powered IoT Devices. Available online: https://www.dialog-semiconductor.com/products/da16200 (accessed on 30 May 2021).
- Ravichandran, R.; Saba, E.; Chen, K.Y.; Goel, M.; Gupta, S.; Patel, S.N. Wibreathe: Estimating respiration rate using wireless signals in natural settings in the home. In Proceedings of the Pervasive Computing and Communications (PerCom), St. Louis, MO, USA, 23–27 March 2015; pp. 131–139.
- Zhao, C.; Chen, K.Y.; Aumi, M.T.I.; Patel, S.; Reynolds, M.S. Side Swipe: Detecting In-air Gestures Around Mobile Devices Using Actual GSM Signal. In Proceedings of the 27th Annual ACM Symposium on User Interface Software and Technology, Honolulu, HI, USA, 5–8 October 2017; ACM: New York, NY, USA, 2014; pp. 527–534, doi:10.1145/2642918.2647380.
- Chatzigiannakis, I.; Hasemann, H.; Karnstedt, M.; Kleine, O.; Kröller, A.; Leggieri, M.; Pfisterer, D.; Römer, K.; Truong, C. Trueself-configuration for the IoT. In Proceedings of the 2012 3rd IEEE International Conference on the Internet of Things, Wuxi, China, 24–26 October 2012; pp. 9–15.
- Chhikara, P.; Singh, P.; Tekchandani, R.; Kumar, N.; Guizani, M. Federated Learning meets Human Emotions: A Decentralized Framework for Human-Computer Interaction for IoT Applications. IEEE Internet Things J.2020, doi:10.1109/JIOT.2020.3037207.
- Barriga, A.d.C.; Martins, A.F.; Simões, M.J.; Faustino, D. The COVID-19 Pandemic: Yet another catalyst for governmental masssurveillance? Soc. Sci. Humanit. Open2020,2, 100096.
- Fan, K.; Ren, Y.; Wang, Y.; Li, H.; Yang, Y. Blockchain-based efficient privacy preserving and data sharing scheme of content-centric network in 5G.IET Commun.2017,12, 527–532.
- Metcalf, D.; Milliard, S.T.; Gomez, M.; Schwartz, M. Wearables and the internet of things for health: Wearable, interconnected devices promise more efficient and comprehensive health care. IEEE Pulse2016,7, 35–39.
- Hall, M.L.; Harty, C.; Knutsen, H.; Yoo, J. Wearables for health: developing designs for functional practicality. In Proceedings of the 2019 ACM International Joint Conference on Pervasive and Ubiquitous Computing and Proceedings of the 2019 ACM International Symposium on Wearable Computers, London, UK, 11-13 September 2019; pp. 1034–1036.
- Ruth, P.S.; Cao, J.; Li, M.; Sunshine, J.E.; Wang, E.J.; Patel, S.N. Multi-Channel Facial Photoplethysmography Sensing. In Proceedings of the 42nd Annual International Conference of the IEEE Engineering in Medicine Biology Society (EMBC), Montreal, QC, Canada, 20–24 July 2020; pp. 4179–4182, doi:10.1109/EMBC44109.2020.9176700.
- Kim, J.; Khan, S.; Wu, P.; Park, S.; Park, H.; Yu, C.; Kim, W. Self-charging wearables for continuous health monitoring.NanoEnergy2021,79, 105419
- Kinnunen, H.; Rantanen, A.; Kenttä, T.; Koskimäki, H. Feasible assessment of recovery and cardiovascular health: accuracy of nocturnal HR and HRV assessed via ring PPG in comparison to medical grade ECG. Physiol. Meas.2020,41, 04NT01.
- Lim, S.A.; Lim, T.H.; Ahmad, A.N. The Applications of Biosensing and Artificial Intelligence Technologies for Rapid Detection and Diagnosis of COVID-19 in Remote Setting. In Diagnostic Strategies for COVID-19 and Other Coronaviruses; Springer: Berlin/Heidelberg, Germany, 2020; pp. 109–134.
- Zhuang, D.; Nguyen, N.; Chen, K.; Chang, J.M. SAIA: Split Artificial Intelligence Architecture for Mobile Healthcare System.arXiv2020, arXiv:2004.12059.
- Liu, X.; Fromm, J.; Patel, S.; McDuff, D. Multi-Task Temporal Shift Attention Networks for On-Device Contactless VitalsMeasurement.arXiv2020, arXiv:2006.03790.
- Retail News Asia. Unmanned medical clinic opened in China. Available online: https://www.retailnews.asia/unmanned-medical-clinic-opened-in-china/ (accessed on 30 May 2021).
- Park, C.; Mariakakis, A.; Yang, J.; Lassala, D.; Djiguiba, Y.; Keita, Y.; Diarra, H.; Wasunna, B.; Fall, F.; Gaye, M.S.; et al. Supporting Smartphone-Based Image Capture of Rapid Diagnostic Tests in Low-Resource Settings. In Proceedings of the 2020International Conference on Information and Communication Technologies and Development, Guayaquil, Ecuador, 17-20 June2020; Association for Computing Machinery: New York, NY, USA, 2020, doi:10.1145/3392561.3394630.
