This entry describes the actual knowledge on diagnosis and management of extra-esophageal manifestations of gastro-esophageal reflux disease.
The 2006 Montreal consensus defined GERD as a condition that develops when the reflux of the stomach contents causes troublesome symptoms and/or complications into the esophagus. Tissue damage related to GERD range from esophagitis to Barrett’s esophagus and esophageal adenocarcinoma; troublesome symptoms attributable to reflux can be esophageal (heartburn, regurgitation) or extra-esophageal (EE). GERD can be further classified by the presence of erosions on endoscopic examination (Erosive Reflux Disease [ERD] and Nonerosive Reflux Disease [NERD]).
- gastroesophageal reflux disease
- proton pump inhibitors
- extraesophageal manifestations
1. Introduction
Gastroesophageal reflux disease (GERD) is a common gastrointestinal (GI) condition with a worldwide diffusion and high prevalence in Western countries.
GERD-related EE manifestations are frequent and represent a diagnostic and therapeutic challenge, being able to involve lungs, upper airways, and mouth, presenting with asthma, laryngitis, chronic cough, dental erosions, and non-cardiac chest pain (Figure 1).
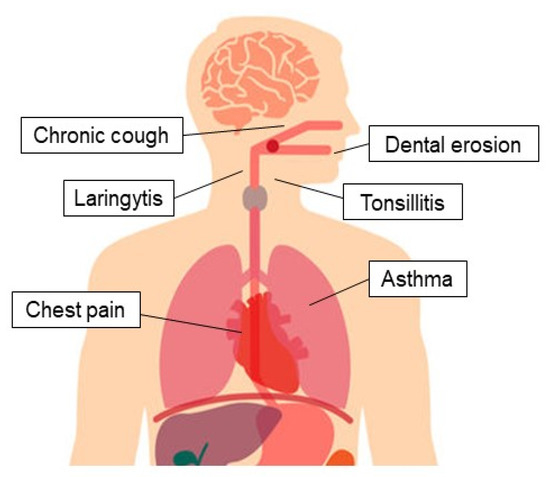
Figure 1. Extra-esophageal presentation of gastroesophageal reflux disease.
2. Common Extra-Esophageal Manifestations
It has been estimated that one-third of patients with GERD may have atypical or EE symptoms[1]: non-cardiac chest pain is the most common complaint (23.1%), followed by pulmonary manifestations (bronchitis—14.0%, asthma—9.3%) and head and neck symptoms (hoarseness—14.8%, globous sensation—7.0%)[2]. In a prospective European study, the prevalence of EE symptoms was 32.8% in patients complaining of heartburn, with a higher proportion in those with ERD (34.9%) than in those with NERD (30.5%)[1]. Chest pain (14.5%), chronic cough (13%), laryngeal disorders (10.4%), and asthma (4.8%) were the commonest disorders associated with GERD[1].
The prevalence of EE disorders in patients not complaining of typical symptoms of GERD is hard to define, due to the increased difficulty of establishing the correct diagnosis. It has been estimated that between 20% and 60% of patients with GERD have head and neck symptoms without any considerable heartburn. Thus, the diagnosis of GERD-related EE manifestations requires a strong collaboration between specialists to exclude alternative causes[3].
Physiologically, the competence of esophageal sphincters (lower and upper) protect the esophageal and laryngeal mucosa from acid refluxate, while the esophago-glottic closure reflex protects the airway. Peristaltic waves perform mechanical clearance by promoting the progression of the bolus through the esophagus: primary peristalsis is a voluntary process that occurs concurrently with swallowing; thus, it is typical of daytime, while secondary peristalsis is involuntary and predominates during the night. Saliva produced during meals neutralizes acids with its content of bicarbonate and plays a chemical clearance during primary peristalsis[4]. When a reflux event happens, esophageal peristalsis pushes the refluxate back in the stomach, while swallowed saliva neutralize acid[4].
The degree and the duration of acid exposure are responsible for the severity of esophageal mucosal injury and GERD-related symptoms, depending from the incompetence of protective mechanisms. Impairment of the esophageal sphincters is the main predisposing condition: upper esophageal sphincter (UES) insufficiency can be diagnosed by esophageal manometry or pH monitoring. Factors associated with EE are the same as those of GERD, either endogenous, as gastric acidity, pepsin, bile, and pancreatic enzymes, or exogenous such as smoke, alcohol, drugs, and hypertonic solutions[5].
Two main mechanisms have been proposed to explain GERD-related EE manifestations: direct damage induced by the aspiration of gastric materials, and indirect damage, which is vagus nerve mediated.
In the hypothesis of a direct stimulus, cough, laryngitis, or asthma exacerbation appear consequently to a tracheal or bronchial aspirate that stimulates the pharynx and larynx. An intact lower esophageal sphincter (LES) and UES protect from gastroesophago-pharyngeal reflux, while high basal UES pressure and the esophago-glottic closure reflex prevent pharyngeal and laryngeal contact with refluxate[5]. The hypothesis of an indirect mechanism is based on the common embryonic origin and vagus innervation of the esophagus and the bronchial tree, considering cough, bronchial spasm, and cardiac-type chest pain induced by the stimulation of the vagal reflex arc from the distal esophageal reflux[5].
A response to the empiric proton pump inhibitor (PPI) therapy (PPI test) would ideally confirm the diagnosis; however, in a meta-analysis, response to PPIs had only sensitivity of 78% and specificity of 54% in the diagnosis of GERD[6]. GERD-related EE manifestations are less responsive to standard therapy with PPIs[7]. Ambulatory 24-h esophageal pH monitoring is indicated in the evaluation of patients’ refractory to a PPI test and when the diagnosis of GERD is uncertain. This diagnostic test is the only capable of assessing the association between refluxates and reflux symptoms, being particularly useful in detecting GERD-related EE manifestations[8].
Upper gastrointestinal endoscopy is recommended when alarm signs are present (e.g., anemia, undesired loss of weight), in cases of no response to PPI treatment (no decrease of GERD symptoms after short PPI treatment, recurrence of EE symptoms besides 3 months of PPI treatment), dysphagia, suspicious of other causes of heartburn (e.g., eosinophilic esophagitis), long-lasting EE symptoms, the presence of GERD complications, the presence of Barrett esophagus, and fundoplication (before and after).
This entry is adapted from the peer-reviewed paper 10.3390/jcm9082559
References
- D. Jaspersen; M. Kulig; J. Labenz; A. Leodolter; T. Lind; W. Meyer-Sabellek; M. Vieth; S. N. Willich; D. Lindner; M. Stolte; et al. Prevalence of extra-oesophageal manifestations in gastro-oesophageal reflux disease: an analysis based on the ProGERD Study. Alimentary Pharmacology & Therapeutics 2003, 17, 1515-1520, 10.1046/j.1365-2036.2003.01606.x.
- G R Locke; N J Talley; S L Fett; A R Zinsmeister; L J Melton; Prevalence and clinical spectrum of gastroesophageal reflux: A population-based study in Olmsted County, Minnesota. Gastroenterology 1997, 112, 1448-1456, 10.1016/s0016-5085(97)70025-8.
- Russo Michele; Miraglia Chiara; Nouvenne Antonio; Leandro Gioacchino; Meschi Tiziana; Luigi De’ Angelis Gian; Di Mario Francesco; Diagnosis of GERD in typical and atypical manifestations. null 1970, 89, 5-11, 10.23750/abm.v89i8-S.7963.
- C. Broers; J. Tack; A. Pauwels; Review article: gastro-oesophageal reflux disease in asthma and chronic obstructive pulmonary disease. Alimentary Pharmacology & Therapeutics 2017, 47, 176-191, 10.1111/apt.14416.
- Fehmi Ates; Michael F. Vaezi; Approach to the patient with presumed extraoesophageal GERD. Best Practice & Research Clinical Gastroenterology 2013, 27, 415-431, 10.1016/j.bpg.2013.06.009.
- Mattijs E. Numans; Joseph Lau; Niek J. De Wit; Peter A. Bonis; Short-Term Treatment with Proton-Pump Inhibitors as a Test for Gastroesophageal Reflux Disease. Annals of Internal Medicine 2004, 140, 518-527, 10.7326/0003-4819-140-7-200404060-00011.
- Matteo Ghisa; Marco Della Coletta; Ilenia Barbuscio; Elisa Marabotto; Brigida Barberio; Marzio Frazzoni; Nicola DE Bortoli; Patrizia Zentilin; Salvatore Tolone; Andrea Ottonello; et al. Updates in the field of non-esophageal gastroesophageal reflux disorder. Expert Review of Gastroenterology & Hepatology 2019, 13, 827-838, 10.1080/17474124.2019.1645593.
- Philip O Katz; Lauren B Gerson; Marcelo F Vela; Guidelines for the Diagnosis and Management of Gastroesophageal Reflux Disease. American Journal of Gastroenterology 2013, 108, 308-328, 10.1038/ajg.2012.444.
