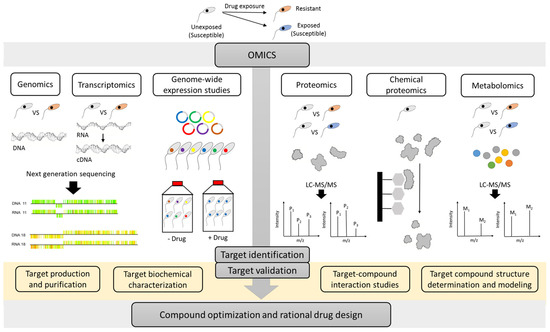
Kinetoplastid parasites are responsible for high mortality and morbidity in (sub)tropical regions. In the development of new drugs, phenotypic screening already allowed the identification of promising new chemical entities with anti-kinetoplastid activity potential, but knowledge on their mode-of-action (MoA) is lacking due to the generally applied whole-cell based approach. However, identification of the drug target is highly beneficial to steer further hit finding, lead optimization and rational drug design. Multiple complementary ‘omics’ approaches have been successfully used to define the MoA or mode-of-resistance (MoR) of current reference drugs and some new anti-kinetoplastid compounds.
- Kinetoplastid
- Leishmaniasis
- Trypanosomiasis
- disease
- treatment
- drug
- drug target
- omics
- mode-of-action
- mode-of-resistance
1. Definition
Kinetoplastids are the causative agents of leishmaniasis, human African trypanosomiasis, and American trypanosomiasis. They are responsible for high mortality and morbidity in (sub)tropical regions. Adequate treatment options are limited and have several drawbacks, such as toxicity, need for parenteral administration, and occurrence of treatment failure and drug resistance. Therefore, there is an urgency for the development of new drugs. Phenotypic screening already allowed the identification of promising new chemical entities with anti-kinetoplastid activity potential, but knowledge on their mode-of-action (MoA) is lacking due to the generally applied whole-cell based approach. However, identification of the drug target is essential to steer further drug discovery and development. Multiple complementary techniques have indeed been used for MoA elucidation.
2. Introduction
References
- Barrett, M.P.; Burchmore, R.; Stich, A.; Lázzari, J.O.; Frasch, A.C.; Cazzulo, J.J.; Krishna, S. The trypanosomiases. Lancet 2003, 362, 1469–1480. [Google Scholar] [CrossRef]
- Hotez, P.J.; Fenwick, A.; Savioli, L.; Molyneux, D. Rescuing the bottom billion through control of neglected tropical diseases. Lancet 2009, 373, 1570–1575. [Google Scholar] [CrossRef]
- Rao, S.P.S.; Barrett, M.P.; Dranoff, G.; Faraday, C.J.; Gimpelewicz, C.R.; Hailu, A.; Jones, C.L.; Kelly, J.M.; Lazdins-Helds, J.K.; Mäser, P.; et al. Drug Discovery for Kinetoplastid Diseases: Future Directions. ACS Infect. Dis. 2018, 5, 152–157. [Google Scholar] [CrossRef] [PubMed]
- Zulfiqar, B.; Shelper, T.B.; Avery, V.M. Leishmaniasis drug discovery: Recent progress and challenges in assay development. Drug Discov. Today 2017, 22, 1516–1531. [Google Scholar] [CrossRef] [PubMed]
- Perez-Molina, J.A.; Molina, I. Chagas disease. Lancet 2018, 391, 82–94. [Google Scholar] [CrossRef]
- Büscher, P.; Cecchi, G.; Jamonneau, V.; Priotto, G. Human African trypanosomiasis. Lancet 2017, 390, 2397–2409. [Google Scholar] [CrossRef]
- Baker, C.H.; Welburn, S.C. The Long Wait for a New Drug for Human African Trypanosomiasis. Trends Parasitol. 2018, 34, 818–827. [Google Scholar] [CrossRef]
- Gilbert, I.H. Drug Discovery for Neglected Diseases: Molecular Target-Based and Phenotypic Approaches. J. Med. Chem. 2013, 56, 7719–7726. [Google Scholar] [CrossRef]
- Renslo, A.R.; McKerrow, J.H. Drug discovery and development for neglected parasitic diseases. Nat. Methods 2006, 2, 701–710. [Google Scholar] [CrossRef]
- Scarim, C.B.; Jornada, D.H.; Chelucci, R.C.; De Almeida, L.; Dos Santos, J.L.; Chung, M.C.; Chin, C.M. Current advances in drug discovery for Chagas disease. Eur. J. Med. Chem. 2018, 155, 824–838. [Google Scholar] [CrossRef]
- Osorio-Méndez, J.F.; Cevallos, A.M. Discovery and Genetic Validation of Chemotherapeutic Targets for Chagas’ Disease. Front. Microbiol. 2019, 8, 439. [Google Scholar] [CrossRef] [PubMed]
- De Rycker, M.; Baragaña, B.; Duce, S.L.; Gilbert, I.H. Challenges and recent progress in drug discovery for tropical diseases. Nature 2018, 559, 498–506. [Google Scholar] [CrossRef] [PubMed]
- Grishin, N.V.; Osterman, A.L.; Brooks, H.B.; Phillips, M.A.; Goldsmith, E.J. X-ray Structure of Ornithine Decarboxylase from Trypanosoma brucei: The Native Structure and the Structure in Complex with α-Difluoromethylornithine. Biochemistry 1999, 38, 15174–15184. [Google Scholar] [CrossRef] [PubMed]
- Sykes, M.L.; Avery, V.M. Approaches to Protozoan Drug Discovery: Phenotypic Screening. J. Med. Chem. 2013, 56, 7727–7740. [Google Scholar] [CrossRef]
- Alves, F.; Bilbe, G.; Blesson, S.; Goyal, V.; Monnerat, S.; Mowbray, C.; Ouattara, G.M.; Pécoul, B.; Rijal, S.; Rode, J.; et al. Recent Development of Visceral Leishmaniasis Treatments: Successes, Pitfalls, and Perspectives. Clin. Microbiol. Rev. 2018, 31, e00048-18. [Google Scholar] [CrossRef]
- Freitas-Junior, L.H.; Chatelain, E.; Kim, H.A.; Siqueira-Neto, J.L. Visceral leishmaniasis treatment: What do we have, what do we need and how to deliver it? Int. J. Parasitol. Drugs Drug Resist. 2012, 2, 11–19. [Google Scholar] [CrossRef]
- Berninger, M.; Schmidt, I.; Ponte-Sucre, A.; Holzgrabe, U. Novel lead compounds in pre-clinical development against African sleeping sickness. MedChemComm 2017, 8, 1872–1890. [Google Scholar] [CrossRef]
- Tulloch, L.; Menzies, S.; Coron, R.P.; Roberts, M.D.; Florence, G.J.; Smith, T.K. Direct and indirect approaches to identify drug modes of action. IUBMB Life 2017, 70, 9–22. [Google Scholar] [CrossRef]
- Terstappen, G.C.; Schlüpen, C.; Raggiaschi, R.; Gaviraghi, G. Target deconvolution strategies in drug discovery. Nat. Rev. Drug Discov. 2007, 6, 891–903. [Google Scholar] [CrossRef]
- Moffat, J.G.; Vincent, F.; Lee, J.A.; Eder, J.; Prunotto, M. Opportunities and challenges in phenotypic drug discovery: An industry perspective. Nat. Rev. Drug Discov. 2017, 16, 531–543. [Google Scholar] [CrossRef]
- Hefnawy, A.; Berg, M.; Dujardin, J.-C.; De Muylder, G. Exploiting Knowledge on Leishmania Drug Resistance to Support the Quest for New Drugs. Trends Parasitol. 2017, 33, 162–174. [Google Scholar] [CrossRef] [PubMed]
- Azad, M.A.; Wright, G.D. Determining the mode of action of bioactive compounds. Bioorganic Med. Chem. 2012, 20, 1929–1939. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.; Lodge, R.; Raymond, F.; Ritt, J.F.; Jalaguier, P.; Corbeil, J.; Tremblay, M.J. Gene expression modulation and the molecular mechanisms involved in Nelfinavir resistance in Leishmania donovani axenic amastigotes. Mol. Microbiol. 2013, 89, 565–582. [Google Scholar] [CrossRef] [PubMed]
This entry is adapted from the peer-reviewed paper 10.3390/microorganisms8060950
