The COVID-19 pandemic is a serious challenge for societies around the globe as entire populations have fallen victim to the infectious spread and have taken up social distancing. In many countries, people have had to self-isolate and to be confined to their homes for several weeks to months to prevent the spread of the virus. Social distancing measures have had both negative and positive impacts on various aspects of economies, lifestyles, education, transportation, food supply, health, social life, and mental wellbeing.
- COVID-19
- economy
- lifestyle
- health
- education
- environment
1. Introduction
COVID-19 is a disease that causes the novel acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which has spread throughout most countries and has caused multiple health and social problems. Disturbances in various areas of life have been consequences of the restrictions imposed by governments and health authorities, as mentioned in Table 1 [1]. For instance, health, education, community relationships, and availability of food and jobs have been impacted by the restrictions applied to limit the transmission of the disease [2].
2. Global Economic Recession
2.1. During the Peak Period of the COVID-19 Outbreak
Many studies proved that economic growth is greatly related to population health [46]. COVID-19 may cause either the death of workers or their incapacitation, and both cases affect the economy by interrupting production. Various countries previously imported numerous products from China. Since the virus outbreak, however, China’s production has considerably slowed down. Hence, the economy dropped by 0.4%, accompanied by a decrease in the global economy by 0.1% [47]. As a reaction to the growing fear, China’s central bank pumped out about USD 22 billion into the system in February 2020 to stabilize the market [48]. It will be difficult for governments to minimize the negative impact of the COVID-19 pandemic on the economy since the highest priority was to reduce death rates. However, parallel measures have to be taken to counter the inevitable economic downturn [49].
2.2. After the Shock Period and Updates
After the first sudden wave, the disease spread around the world and began to change between countries. Per the latest updates of 23 April 2021, the United States harbors the largest number of injuries, followed by India; then Brazil; then France, Russia, Turkey; and the United Kingdom [51].
Although it is impossible to precisely determine the economic damage caused by the COVID-19 outbreak, all economists agree that it has had a severe negative effect on the global economy. Since the virus became a global pandemic, it is estimated that most economic growth will decrease by at least 2.4% of respective GDPs globally.
2.3. Transportation
The COVID-19 pandemic became a global situation within weeks. During that period, worldwide communities looked to transportation systems, public and private, as one of the main reasons for the global pandemic. As a result, transportation systems struggled to preserve their economic value due to both the preventive measures taken by governments as well as the fear of people regarding travel due to the risk of transmission/infection [22,53,54]. An inter-county ban on China was the first precaution, and hence, the challenge became a reality; this was followed by a complete suspension of planes leaving from China.
Losses to the commercial aviation sector reached nearly USD 252 billion in 2020 [21,23]. The new situation and the exacerbation of losses led to an urgent necessity to open transportation again, but at the forefront were social distancing, wearing masks, personal hygiene, and frequent hand washing, as some of the prerequisites to maintain health safety.
3. Lifestyle during the COVID-19 Pandemic
3.1. Staying at Home
The spread of COVID-19 around the world led to increased calls from many parties, including international organizations, government institutions, and individuals, to stay at home [57]. Stay-at-home orders can reduce activities associated with community spread of the virus, including population movement and close person-to-person contact outside the household. Close contact between family members, relatives, or friends is one cause of COVID-19 spread [7,8]. Stay-at-home orders might assist in limiting potential exposure to COVID-19 and garnered significant public support. On the contrary, the social and psychological damages were tangible and created a feeling of isolation and loneliness [10,58].
3.2. Social Media
Under the COVID-19 pandemic, social media has been engaged directly as the fastest method for spreading information. Whether it is used as entertainment or as a source of reliable or fabricated information, online communication occurs primarily through Facebook (79% of internet users), followed by Instagram (32%), and then Twitter (24%) [76,77]. The number of global social media users reached 3.6 billion in 2020 and is expected to reach 4.41 billion users in 2025 [78]. Therefore, social media could serve as a suitable method for communicating the best practices for preventing COVID-19 spread.
Facebook and Twitter directed people to confirmed medical care websites. Google Scholar highlighted the top leading journals and recommended articles surrounding COVID-19, which helped to control online traffic by directing users to trusted sources (Figure 1) [26,79,80].
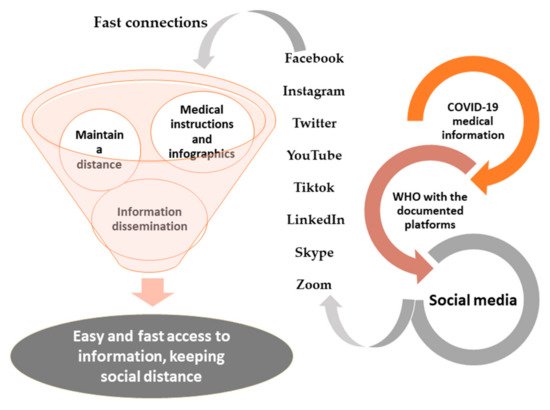
Figure 1. Social media participation and the continuation of its role during the pandemic, especially using documented pages of international and local organizations as well as press institutions on the Facebook and Twitter platforms to update information about COVID-19 around the clock for users.
A bad reputation for misinformation is dominant around social media. This becomes very clear when the general population addresses questions such as whether COVID-19 was created in a laboratory, what the symptoms and nature of the virus are, as well as any precautions that should be taken against it.
4. Education and Research Activities during the COVID-19 Pandemic
4.1. Education
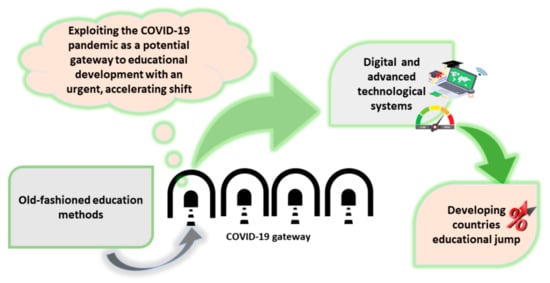
espite it not being new, online courses were the only way to replace face-to-face contact. Some educational facilities already had the infrastructure needed for applying for online courses at a large scale. This can be taken as a positive point in developing countries to begin paying attention to providing these means, to consider it among essential needs, as well as to face the current crisis and to explore new strategies in the future to keep up with technological improvements (Figure 2) [28].
4.2. Research Activities
Just as life activities were influenced by COVID-19 circumstances, so was research activity. During the pandemic, most research and research-related activities have been carried out remotely/virtually. Worldwide, universities, and research centers have abruptly stopped their routines. Scientists were worried about the progress of their research projects, and in response, many universities and research institutes supported their staff working at home [31]. In parallel to this, there was an urgent need to continue research activities to find a vaccine or optimal treatment for COVID-19-related disorders, so keeping research participants and staff active was necessary.
5. Health Sector during the COVID-19 Pandemic
5.1. Food Supply, Dietary Patterns, Nutrition, and Health
In developing countries, food insecurity is mainly attributed to the rising food inflation (inability to afford adequate food supply) [104]. The State of Food Security and Nutrition in the World, in their last published edition, estimated that the COVID-19 pandemic may have added 83–132 million more people to the undernourished population of 2020 [106].
In developed countries, however, it is more pertinent to trade restrictions and currency deflation [104]. Export-restrictive measures implemented by some countries have put the trade flow of staple foods such as wheat and rice at risk [103].
Food supply distribution influences the individual’s food-related behavior. This is relevant because nutrition is vital for health and well-being, especially if the immune system is involved. Moreover, restricted access to fresh food may also have detrimental effects on both mental and physical health [17].
5.2. Health and Psychological Effects on Students during the School Closures
Psychological effects of the pandemic and quarantine measures are evident among all groups of people, including fear of disease and infection, as well as its consequences. Among students, fear of the future, especially concerning educational attainment and qualification for jobs, has been abundant.
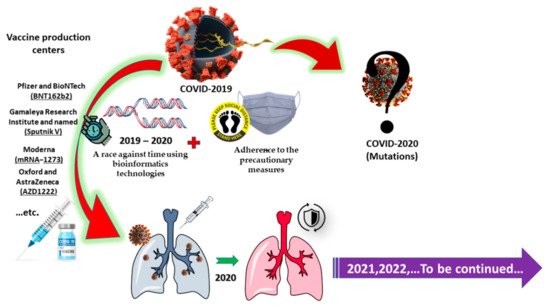
5.3. Vaccine Production
Combatting the COVID-19 pandemic is a race against time, testing the world’s ability to act quickly as the virus mutates. Subsequently, a variety of efforts have been made to create vaccines against COVID-19. Vaccine production takes place at various stages, including preclinical and clinical stages, which is a three-phase process. According to the WHO, the vaccine must be highly efficient, healthy, and appropriate for all ages and backgrounds [128]. Researchers are investigating various formulations of medications for treating COVID-19 patients, but all of the formulas are still under examination.
After nearly one year, Pfizer in cooperation with BioNTech announced (on 9 November 2020) its readiness to offer a vaccine against COVID-19 with some realistic and trusted documentation (Figure 3) [34]. The results were considered extremely rapid in relation to common vaccine production processes. Such processes normally require many years of high-quality research and procedures in follow-up, bearing in mind the viral mRNA and the potential for mutation [132].
6. Global Warming and Reports on Weather and the Environment during the COVID-19 Pandemic
Despite the epidemic’s impact on humans, it has been somewhat beneficial to nature during the pause from human activity.
Changes started to be noticed in the calculations after a small period post-implementation of COVID-19 precautions as a result of the reduced use of coal-fired power stations and less oil burned for transportation, and a 20% drop in the scale of greenhouse gas emissions was observed by March 2020 in China. Chinese cities reported an approximately 40% drop in comparison to the same period in 2019 [94,95].
In the United States, a third of Americans drink groundwater as their primary source of hydration and most neighborhoods are located near factories, which may increase the risk of wastewater leaking into the groundwater [137].
A 50% increase in deforested areas according to the Brazilian National Institute for Space Research (INPE) was already noticed in the first quarter of 2020 compared to the previous year [38].
7. Conclusions
COVID-19 poses a great threat to global health. After the aggravation of the pandemic, it is no longer just a transient health condition but rather has led to global quarantines. Countries have begun a battle of endurance in regard to confronting the disease spread.
Sometimes, misfortunes come with benefits. During the crisis, the greatest benefit to the land and to nature resulted from human quarantine. The global climate recorded high cure rates and gave humans a definitive guide about how to solve some of nature’s problems that had previously been thought to be impossible. Response from nature served to alert humans and provided insights into human selfishness and negligence of nature.
Recently, some communities have begun to relax their precautionary measures again when confronting the disease. Although social distance and healthcare strategies are the main methods used to avoid disease spread, communities have noticed that these strategies have consequences for mental health; for children, and younger and elder individuals; and for the poor or those with limited income [138,139]. Negative effects extend also to food availability and the economy. Patience and rationality are very much required when making decisions during the coming period or the post-pandemic period and when returning to normal life in order to avoid experiencing a relapse in the spread of the disease. It is necessary to think outside the box and not only to identify the negative points but also to learn from them. Ideas or, more precisely, evolutionary leaps that create a better society with greater intellect and awareness of immunity always sprout during crises and even wars.
coronavirus disease-2019 (COVID-19): The epidemic and the challenges. Int. J. Antimicrob. Agents 2020, 55, 105924–105932,
doi:10.1016/j.ijantimicag.2020.105924.
2. Dwivedi, Y.K.; Hughes, D.L.; Coombs, C.; Constantiou, I.; Duan, Y.; Edwards, J.S.; Gupta, B.; Lal, B.; Misra, S.; Prashant, P.; et
al. Impact of COVID-19 pandemic on information management research and practice: Transforming education, work and life.
Int. J. Inf. Manag. 2020, 55, 102211–102230, doi:10.1016/j.ijinfomgt.2020.102211.
3. Omary, M.B.; Eswaraka, J.; Kimball, S.D.; Moghe, P.V.; Panettieri, R.A.; Scotto, K.W. The COVID-19 pandemic and research
shutdown: Staying safe and productive. J. Clin. Investig. 2020, 130, 2745–2748, doi:10.1172/JCI138646.
4. Király, O.; Potenza, M.N.; Stein, D.J.; King, D.L.; Hodgins, D.C.; Saunders, J.B.; Grif, M.D.; Gjoneska, B.; Billieux, J.; Brand, M.;
et al. Preventing problematic internet use during the COVID-19 pandemic: Consensus guidance. Compr. Psychiatry 2020, 100,
152180–152184.
5. de Oliveira Neto, L.; Elsangedy, H.M.; de Oliveira Tavares, V.D.; Teixeira, C.V.L.S.; Behm, D.G.; Da Silva-Grigoletto, M.E. TrainingInHome-training at home during the COVID-19 (SARS-CoV-2) pandemic: Physical exercise and behavior-based approach.
Braz. J. Exerc. Physiol. 2020, 19, 9–19.
6. Chakraborty, I.; Maity, P. COVID-19 outbreak: Migration, effects on society, global environment and prevention. Sci. Total Environ. 2020, 728, 138882–138888, doi:10.1016/j.scitotenv.2020.138882.
7. Coleman, T.S. Thoughts on Financial Crises and Coronavirus. 2020, 1–4, Available online: http://www.hilerun.org/econ/papers/FinCrisesThoughts_20200313.pdf (accessed on 22 May 2021).
8. Wang, Q.; Zhang, F. What does the China’s economic recovery after COVID-19 pandemic mean for the economic growth and
energy consumption of other countries? J. Clean. Prod. 2021, 295, 126265–126284, doi:10.1016/j.jclepro.2021.126265.
9. Altena, E.; Baglioni, C.; Espie, C.A.; Ellis, J.; Gavriloff, D.; Holzinger, B.; Schlarb, A.; Frase, L.; Jernelöv, S.; Riemann, D. Dealing
with sleep problems during home confinement due to the COVID-19 outbreak: Practical recommendations from a task force of
the European CBT-I Academy. J. Sleep Res. 2020, 29, e13052, doi:10.1111/jsr.13052.
10. Douglas, M.; Katikireddi, S.V.; Taulbut, M.; Mckee, M.; Mccartney, G. Mitigating the wider health effects of covid-19 pandemic.
BMJ 2020, 369, 1557–1562, doi:10.1136/bmj.m1557.
11. Allen-Ebrahimian, B. China’s Domestic Violence Epidemic. Axios. Available online: https://www.axios.com/china-domesticviolence-coronavirus-quarantine-7b00c3ba-35bc-4d16-afdd-b76ecfb28882.html 2020 (accessed on 19 March 2021).
12. Guenfoud, I. French Women Use Code Words at Pharmacies to Escape Domestic Violence during Coronavirus. Available
online: https://abcnews.go.com/International/french-women-code-words-pharmacies-escape-domestic-violence/story?id=69954238 2020 (accessed on 19 March 2021).
13. Piquero, A.R.; Jennings, W.G.; Jemison, E.; Kaukinen, C.; Knaul, F.M. Domestic violence during the COVID-19 pandemic-Evidence from a systematic review and meta-analysis. J. Crim. Justice 2021, 74, 101806–101815, doi:10.1016/j.jcrimjus.2021.101806.
14. Feldmann, A.; Gasser, O.; Lichtblau, F.; Pujol, E.; Poese, I.; Dietzel, C.; Wagner, D.; Wichtlhuber, M.; Tapiador, J.; Vallina-Rodriguez, N.; et al. The lockdown effect: Implications of the COVID-19 pandemic on internet traffic. In Proceedings of the ACM
Internet Measurement Conference, Pittsburgh, PA, USA, 27–29 October 2020; Volume 2008, pp. 10959–10976,
doi:10.1145/3419394.3423658.
15. Usher, K.; Bhullar, N.; Durkin, J.; Gyamfi, N.; Jackson, D. Family violence and COVID-19: Increased vulnerability and reduced
options for support. Int. J. Ment. Health 2020, 29, 549–552, doi:10.1111/inm.12735.
16. Campbell, A.M. An increasing risk of family violence during the Covid-19 pandemic : Strengthening community collaborations
to save lives. Forensic Sci. Int. Rep. 2020, 2, 100089–100091, doi:10.1016/j.fsir.2020.100089.
et al. Effects of COVID-19 home confinement on eating behaviour and physical activity: Results of the ECLB-COVID19 international online survey. Nutrients 2020, 12, 1583- 1595.
18. Puig-Domingo, M.; Marazuela, M.; Giustina, A. COVID-19 and endocrine diseases. A statement from the European Society of
Endocrinology. Endocrine 2020, 68, 2–5, doi:10.1007/s12020-020-02294-5.
19. Purwanto, A.; Asbari, M.; Fahlevi, M.; Mufid, A.; Agistiawati, E.; Cahyono, Y.; Suryani, P. Impact of work from home (WFH)
on Indonesian teachers performance during the Covid-19 pandemic: An exploratory study. Int. J. Adv. Sci. Technol. 2020, 29,
6235–6244.
20. Vos, J. De The effect of COVID-19 and subsequent social distancing on travel behavior. Transp. Res. Interdiscip. Perspect. 2020, 5,
100121–100123, doi:10.1016/j.trip.2020.100121.
21. IATA. IATA Economics’ Chart of the Week. International Air Transport Association. Available online:
| https//www.iata.org/en/iata-repository/publications/economic-reports/covid-2019-delivers-unprecedented-shock/2020 cessed on 2 October 2020). |
(ac |
1–21.
23. Amankwah-amoah, J. Stepping up and stepping out of COVID-19: New challenges for environmental sustainability policies in
the global airline industry. J. Clean. Prod. 2020, 271, 123000–123007, doi:10.1016/j.jclepro.2020.123000.
24. Mandrola, J.; Futyma, P. The role of social media in cardiology. Trends Cardiovasc. Med. 2020, 30, 32–35,
doi:10.1016/j.tcm.2019.01.009.
25. Höttecke, D.; Allchin, D. Reconceptualizing nature-of-science education in the age of social media. Sci. Educ. 2020, 104, 641–666,
doi:10.1002/sce.21575.
26. Merchant, R.M.; Lurie, N. Social media and emergency preparedness in response to novel coronavirus. JAMA 2020, 323, 2011–
2012, doi:10.1001/jama.2020.4469.
27. Huerta-álvarez, R.; Cambra-fierro, J.J.; Fuentes-blasco, M. The interplay between social media communication, brand equity
and brand engagement in tourist destinations: An analysis in an emerging economy. J. Destin. Mark. Manag. 2020, 16, 100413–
100424, doi:10.1016/j.jdmm.2020.100413.
28. Timmis, S.; Broadfoot, P.; Sutherland, R.; Oldfield, A. Rethinking assessment in a digital age: Opportunities, challenges and
risks. Br. Educ. Res. J. 2016, 42, 454–476, doi:10.1002/berj.3215.
29. Viner, R.M.; Russell, S.J.; Croker, H.; Packer, J.; Ward, J.; Stansfield, C.; Mytton, O.; Bonell, C.; Booy, R. Review school closure
and management practices during coronavirus outbreaks including COVID-19: A rapid systematic review. Lancet Child Adolesc.
Health 2020, 4, 397–404, doi:10.1016/S2352-4642(20)30095-X.
30. Ahmed, H.; Allaf, M.; Elghazaly, H. COVID-19 and medical. Lancet Infect. Dis. 2020, 2019, 777–778, doi:10.1016/S1473-
3099(20)30226-7.
31. Ghebreyesus, T.A. Safeguard research in the time of COVID-19. Nat. Med. 2020, 26, 443, doi:10.1038/s41591-020-0852-1.
32. Chahrour, M.; Assi, S.; Bejjani, M.; Nasrallah, A.A.; Salhab, H.; Fares, M.; Khachfe, H.H. A bibliometric analysis of COVID-19
research activity: A call for increased output. Cureus 2020, 2, e7357, doi:10.7759/cureus.7357.
33. Mattioli, A.V.; Sciomer, S.; Cocchi, C.; Maffei, S.; Gallina, S. Quarantine during COVID-19 outbreak: Changes in diet and physical activity increase the risk of cardiovascular disease. Nutr. Metab. Cardiovasc. Dis. 2020, 30, 1409–1417, doi:10.1016/j.numecd.2020.05.020.
34. Callaway, E. What Pfizer’s landmark COVID vaccine results mean for the pandemic. Nature 2020, 1–7, doi:10.1038/d41586-020-
03166-8.
35. Matsungo, T.M.; Chopera, P. The effect of the COVID-19 induced lockdown on nutrition, health and lifestyle patterns among
adults in Zimbabwe. medRxiv 2020, 3, 205–212.
36. Mattioli, A.V.; Nasi, M.; Farinetti, A. COVID-19 pandemic: The effects of quarantine on cardiovascular risk. Eur. J. Clin. Nutr.
2020, 74, 852–855, doi:10.1038/s41430-020-0646-z.
37. Lindsey, P.; Allan, J.; Brehony, P.; Dickman, A.; Robson, A.; Begg, C.; Bhammar, H.; Blanken, L.; Breuer, T.; Fitzgerald, K. Conserving Africa’s wildlife and wildlands through the COVID-19 crisis and beyond. Nat. Ecol. Evol. 2020, 4, 1300–1310,
doi:10.1038/s41559-020-1275-6.
38. Feldman, A.L.; Chávez, C.; Vélez, M.A.; Bejarano, H.; Chimeli, A.B.; Féres, J.; Robalino, J. Environmental impacts and policy
responses to Covid-19: A view from Latin America. Environ. Resour. Econ. 2020, 13, 1–6, doi:10.1007/s10640-020-00460-x.
39. Mandal, I.; Pal, S. COVID-19 pandemic persuaded lockdown effects on environment over stone quarrying and crushing areas.
Sci. Total Environ. 2020, 732, 139281–139290, doi:10.1016/j.scitotenv.2020.139281.
40. Zambrano-monserrate, M.A.; Alejandra, M.; Sanchez-alcalde, L. Indirect effects of COVID-19 on the environment. Sci. Total
Environ. 2020, 728, 138813–138816, doi:10.1016/j.scitotenv.2020.138813.
41. Saadat, S.; Rawtani, D.; Mustansar, C. Environmental perspective of COVID-19. Sci. Total Environ. 2020, 728, 138870–138875,
doi:10.1016/j.scitotenv.2020.138870.
42. Khalifa, S.A.M.; Mohamed, B.S.; Elashal, M.H.; Du, M.; Guo, Z.; Zhao, C.; Musharraf, S.G.; Boskabady, M.H.; El-Seedi, H.H.R.;
Efferth, T.; et al. Comprehensive overview on multiple strategies fighting covid-19. Int. J. Environ. Res. Public Health 2020, 17,
5813-5825, doi:10.3390/ijerph17165813.
Coronavirus and Financial Stability; SAFE Policy Letter, No. 78, Leibniz Institute for Financial Research SAFE: Frankfurt, Germany, 2020.
44. Khan, N.; Fahad, S.; Faisal, S.; Naushad, M. Quarantine Role in the Control of Corona Virus in the World and Its Impact on the
World Economy 2020. Available at: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3556940 (accessed on 5 April 2021).
45. Baldwin, R.E.; di Mauro, W. Mitigating the COVID Economic Crisis; Centre for Economic Policy Research; 2020. Available online:
https://voxeu.org/content/mitigating-covid-economic-crisis-act-fast-and-do-whatever-it-takes (accessed on 5 April 2021).
46. Summers, L.H.; Pritchett, L. Wealthier is healthier. J. Hum. Resour. 1996, 31, 841–868.
47. Scenarios, S. The global macroeconomic impacts of COVID-19. Cent. Appl. Macroecon. Anal. 2020, 1–45.
48. Sohrabi, C.; Alsafi, Z.; Neill, N.O.; Khan, M.; Kerwan, A.; Al-jabir, A.; Iosifidis, C.; Agha, R. World Health Organization declares
global emergency: A review of the 2019 novel coronavirus (COVID-19). Int. J. Surg. 2020, 76, 71–76, doi:10.1016/j.ijsu.2020.02.034.
49. Korea, S.; Kong, H. How will country-based mitigation measures influence the course of the COVID-19 epidemic ? Lancet 2020,
395, 931–934, doi:10.1016/S0140-6736(20)30567-5.
50. Fernandes, N. Economic Effects of Coronavirus Outbreak (COVID-19) on the World Economy. 2020, 2–32. Available online:
https://edisciplinas.usp.br/pluginfile.php/5662406/mod_resource/content/1/FERNANDES_Economic%20Effects%20of%20Coronavirus%20Outbreak%20%28COVID19%29%20on%20the%20World%20Economy.pdf (accessed on 21 May
2021).
51. WHO Coronavirus (COVID-19) Dashboard|WHO Coronavirus (COVID-19) Dashboard with Vaccination Data. Available
online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019?adgroupsurvey={adgroupsurvey}&gclid=EAIaIQobChMI9cXs_rjV8AIVwV1gCh3YBwEoEAAYASAAEgIyHvD_BwE (accessed on 23 April 2021).
52. Li, Q.; Guan, X.; Wu, P.; Wang, X.; Zhou, L.; Tong, Y.; Ren, R.; Leung, K.S.M.; Lau, E.H.Y.; Wong, J.Y.; et al. Early transmission
dynamics in Wuhan, China, of novel coronavirus–infected Pneumonia. N. Engl. J. Med. 2020, 382, 1199–1207,
doi:10.1056/nejmoa2001316.
53. Medicine, T.; Xu, Y.; Bi, Y.; Wang, W.; Zheng, D.R.; Xu, Y.; Bi, Y.; Wang, W. Spatial transmission of COVID-19 via public and
private transportation in China. Travel Med. Infect. Dis. 2020, 34, 101626–101628, doi:10.1016/j.tmaid.2020.101626.
54. Loske, D. The impact of COVID-19 on transport volume and freight capacity dynamics: An empirical analysis in German food
retail logistics. Transp. Res. Interdiscip. Perspect. 2020, 6, 100165–100170, doi:10.1016/j.trip.2020.100165.
55. Dube, K.; Nhamo, G.; Chikodzi, D. COVID-19 pandemic and prospects for recovery of the global aviation industry. J. Air Transp.
Manag. 2021, 92, 102022-102033, doi:10.1016/j.jairtraman.2021.102022.
56. Id, K.P.; Kaewpoungngam, K.; Chotirosniramit, K. Commercial airline protocol during COVID-19 pandemic: An experience of
Thai Airways International. PLoS ONE 2020, 15, e0237299, doi:10.1371/journal.pone.0237299.
57. Hamidi, S.; Zandiatashbar, A. Compact development and adherence to stay-at-home order during the COVID-19 pandemic: A
longitudinal investigation in the United States. Landsc. Urban Plan. 2021, 205, 103952–103960, doi:10.1016/j.landurbplan.2020.103952.
58. Brooke, J.; Jackson, D. Older people and COVID-19: Isolation, risk and ageism. J. Clin. Nurs. 2020, 29, 2044–2046,
doi:10.1111/jocn.15274.
59. EuroNews Domestic Violence Cases Jump 30% during Lockdown in France. Available online: https://www.euronews.com/2020/03/28/domestic-violence-cases-jump-30-during-lockdown-in-france (accessed on 5 April 2021).
60. Graham-Harrison, E.; Giuffrida, A.; Smith, H.; Ford, L. Lockdowns around the world bring rise in domestic violence. Available
online: https//www.theguardian.com/Soc (accessed on 20 January 2021).
61. Rada, A.G. Covid-19: The precarious position of Spain’s nursing homes. BMJ 2020, 369, 1–3, doi:10.1136/bmj.m1554.
62. Iacobucci, G. Covid-19: Lack of PPE in care homes is risking spread of virus, leaders warn. BMJ 2020, 368, doi:10.1136/bmj.m1280
63. Albaqawi, H.M.; Pasay-an, E.; Mostoles, R.; Villareal, S. Risk assessment and management among frontline nurses in the context
of the COVID-19 virus in the northern region of the Kingdom of Saudi Arabia. Appl. Nurs. Res. 2021, 58, 151410–151415,
doi:10.1016/j.apnr.2021.151410.
64. Yu, X.; Liu, C.; Wang, H.; Feil, J.H. The impact of COVID-19 on food prices in China: Evidence of four major food products from
Beijing, Shandong and Hubei Provinces. China Agric. Econ. Rev. 2020, 12, 445–458, doi:10.1108/CAER-04-2020-0054.
65. Ammar, A.; Chtourou, H.; Boukhris, O.; Trabelsi, K.; Masmoudi, L.; Brach, M.; Aloui, A.; Hammouda, O.; Paineiras-domingos,
L.L.; Braakman-jansen, A. Social participation and life satisfaction of peoples during the COVID-19 home confinement: The
ECLB-COVID19 multicenter study. medRxiv 2020, doi:10.1101/2020.05.05.20091066
66. Di Renzo, L.; Gualtieri, P.; Pivari, F.; Soldati, L.; Attinà, A.; Cinelli, G.; Cinelli, G.; Leggeri, C.; Caparello, G.; Barrea, L.; et al.
Eating habits and lifestyle changes during COVID-19 lockdown: An Italian survey. J. Transl. Med. 2020, 18, 229–233,
doi:10.1186/s12967-020-02399-5.
67. de Faria Coelho-Ravagnani, C.; Corgosinho, F.C.; Sanches, F.L.F.Z.; Prado, C.M.M.; Laviano, A.; Mota, J.F. Dietary recommendations during the COVID-19 pandemic. Nutr. Rev. 2021, 79, 382–393, doi:10.1093/nutrit/nuaa067.
68. Narici, M.; De Vito, G.; Franchi, M.; Paoli, A.; Moro, T.; Marcolin, G.; Grassi, B.; Baldassarre, G.; Zuccarelli, L.; Biolo, G.; et al.
Impact of sedentarism due to the COVID-19 home confinement on neuromuscular, cardiovascular and metabolic health: Physiological and pathophysiological implications and recommendations for physical and nutritional countermeasures. Eur. J. Sport
Sci. 2020, doi:10.1080/17461391.2020.1761076.
to help with the fight against COVID-19. J. Sports Sci. 2021, 39, 101–107, doi:10.1080/02640414.2020.1807089.
70. Kumari, A.; Ranjan, P.; Sharma, K.A.; Sahu, A.; Bharti, J.; Zangmo, R.; Bhatla, N. Impact of COVID-19 on psychosocial functioning of peripartum women: A qualitative study comprising focus group discussions and in-depth interviews. Int. J. Gynecol.
Obstet. 2021, 152, 321–327, doi:10.1002/ijgo.13524.
71. Williams, L.; Rollins, L.; Young, D.; Fleming, L.; Grealy, M.; Janssen, X.; Kirk, A.; MacDonald, B.; Flowers, P. What have we
learned about positive changes experienced during COVID-19 lockdown? Evidence of the social patterning of change. PLoS
ONE 2021, 16, e0244873, doi:10.1371/journal.pone.0244873.
72. Barbu-Banes, A.-O. Microtargeting in social media: Definitions and ethical issues. Univ. Babes Bolyai Ephemer. 2013, 58, 83–90.
73. Maryam, M. 10 TikTok Statistics That You Need to Know in 2020 Available online: https://my.oberlo.com/blog/tiktok-statistics
(accessed on 15 April 2021).
74. Jacobson, J.; Gruzd, A.; Hernández-garcía, Á.; Rogers, T.; Management, R.; Street, V.; Mb, C. Social media marketing: Who is
watching the watchers ? J. Retail. Consum. Serv. 2020, 53, 101774–101785, doi:10.1016/j.jretconser.2019.03.001.
75. Oliveira, T.; Araujo, B.; Tam, C. Why do people share their travel experiences on social media? Tour. Manag. 2020, 78, 104041–
104054, doi:10.1016/j.tourman.2019.104041.
76. Chan, A.K.M.; Nickson, C.P.; Rudolph, J.W.; Lee, A.; Joynt, G.M. Social media for rapid knowledge dissemination: early experience from the COVID-19 pandemic. Anaesthesia 2020, 75, 1579–1582.
77. Greenwood, S.; Perrin, A.; Duggan, M. Social media update 2016. Pew Res. Center 2016, 11, 1-18.
78. Clement, J. Number of Global Social Media Users 2017–2025. Stat. Website 2020. Available online: https://www.statista.com/statistics/278414/number-of-worldwide-social-network-users/ (accessed on 23 January 2021).
79. Jin, K.-X. Keeping People Safe and Informed about the Coronavirus. Faceb. Newsroom Website. 2020. Available online:
https://about.fb.com/news/2020/12/coronavirus/ (accessed on 22 May 2021).
80. Josephson, A.; Lambe, E. Brand Communications in Time of Crisis, 2020. Available online: https://blog.twitter.com/en_us/topics/company/2020/Brand-communications-in-time-of-crisis.html (accessed on 15 Decembre 2020).
81. Google Scholar. Available online: https://scholar.google.com.eg/scholar?as_ylo=2017&q=hesham+el+seedi&hl=en&as_sdt=0,5
(accessed on 10 April 2021).
82. Allington, D.; Duffy, B.; Wessely, S.; Dhavan, N.; Rubin, J. Health-protective behaviour, social media usage and conspiracy
belief during the COVID-19 public health emergency. Psychol. Med. 2020, 1-7, doi: 10.1017/S003329172000224X.
83. Bedford, J.; Enria, D.; Giesecke, J.; Heymann, D.L.; Ihekweazu, C.; Kobinger, G.; Lane, H.C.; Memish, Z.; Oh, M.-d.; Schuchat,
A. COVID-19: Towards controlling of a pandemic. Lancet 2020, 395, 1015–1018, doi:10.1016/S0140-6736(20)30673-5.
84. Liu, W.; Zhang, Q.; Chen, J.; Xiang, R.; Song, H.; Shu, S.; Chen, L.; Liang, L.; Zhou, J.; You, L. Detection of COOVID-19 in children
in early January 2020 in Wuhan, China. N. Engl. J. Med. 2020, 382, 1370–1371
85. Moghadas, S.M. Simulating the effect of school closure during COVID-19 outbreaks in Ontario, Canada. BMC Med. 2020, 18,
230–237
86. Bosveld, M.H.; van Doorn, D.P.C.; Stassen, P.M.; Westerman, D.; Bergmans, D.C.J.J.; van der Horst, I.C.C.; van Mook, W.N.K.A.
Lessons learned: Contribution to healthcare by medical students during COVID-19. J. Crit. Care 2020, 10–13,
doi:10.1016/j.jcrc.2020.09.015.
87. Ali, R.A.; Rafie, M.; Arshad, M. Challenges and benefits in implementing M-learning in pre-university education in Egypt. Int.
J. Comput. Acad. Res. 2015, 4, 144–151.
88. Edmodo. Egyptan Edmodo online platform. Available online: https://new.edmodo.com/login?go2url=%2Fhome (accessed on
20 May 2021).
89. Bank, E.K. Egyptian Knowledge Bank. Available online: http://www.ekb.eg/ (accessed on 19 October 2020).
90. Egyptian_Ministry_of_Education Egyptian Ministry of Education. Available online: https://moe.gov.eg/ (accessed on 19 October 2020).
91. Saberi, P. Research in the time of coronavirus: Continuing ongoing studies in the midst of the covid-19 pandem. AIDS Behav.
2020, 24, 2232–2235, doi:10.1007/s10461-020-02868-4.
92. Sohrabi, C.; Mathew, G.; Franchi, T.; Kerwan, A.; Griffin, M.; Soleil C Del Mundo, J.; Ali, S.A.; Agha, M.; Agha, R. Impact of the
coronavirus (COVID-19) pandemic on scientific research and implications for clinical academic training–A review. Int. J. Surg.
2021, 86, 57–63, doi:10.1016/j.ijsu.2020.12.008
93. Mbunge, E.; Akinnuwesi, B.; Fashoto, S.G.; Metfula, A.S.; Mashwama, P. A critical review of emerging technologies for tackling
COVID-19 pandemic. Hum. Behav. Emerg. Technol. 2020, 2, 25–39, doi:10.1002/hbe2.237
94. Chen, J.; Liu, X.; Wang, D.; Jin, Y.; He, M.; Ma, Y.; Zhao, X.; Song, S.; Zhang, L.; Xiang, X.; et al. Risk factors for depression and
anxiety in healthcare workers deployed during the COVID-19 outbreak in China. Soc. Psychiatry Psychiatr. Epidemiol. 2021, 56,
47–55, doi:10.1007/s00127-020-01954-1.
95. Mina, F.B.; Billah, M.; Karmakar, S.; Das, S.; Rahman, M.S.; Hasan, M.F.; Acharjee, U.K. An online observational study assessing
clinical characteristics and impacts of the COVID-19 pandemic on mental health: A perspective study from Bangladesh. J. Public
Health 2021, doi:10.1007/s10389-020-01445-2.
96. Sahebi, A.; Nejati-Zarnaqi, B.; Moayedi, S.; Yousefi, K.; Torres, M.; Golitaleb, M. The prevalence of anxiety and depression
among healthcare workers during the COVID-19 pandemic: An umbrella review of meta-analyses. Prog. Neuro Psychopharmacol.
Biol. Psychiatry 2021, 107, 110247–110253, doi:10.1016/j.pnpbp.2021.110247
and development on therapeutic agents and vaccines for COVID-19 and related human coronavirus diseases. ACS Cent. Sci.
2020, 6, 315–331, doi:10.1021/acscentsci.0c00272.
98. Yanow, S.K.; Good, M.F. Nonessential research in the new normal: The impact of COVID-19. Am. J. Trop. Med. Hyg. 2020, 102,
1164–1165, doi:10.4269/ajtmh.20-0325.
99. Udugama, B.; Kadhiresan, P.; Kozlowski, H.N.; Malekjahani, A.; Osborne, M.; Li, V.Y.C.; Chen, H.; Mubareka, S.; Gubbay, J.B.;
Chan, W.C.W. Diagnosing COVID-19: The disease and tools for detection. ACS Nano 2020, 14, 3822–3835,
doi:10.1021/acsnano.0c02624.
100. Yu, H.; Li, C.; Wang, X.; Duan, J.; Yang, N.; Xie, L.; Yuan, Y.; Li, S.; Bi, C.; Yang, B.; et al. Techniques and strategies for potential
protein target discovery and active pharmaceutical molecule screening in a pandemic. J. Proteome Res. 2020, 19, 4242–4258,
doi:10.1021/acs.jproteome.0c00372.
101. Gabster, B.P.; van Daalen, K.; Dhatt, R.; Barry, M. Challenges for the female academic during the COVID-19 pandemic. Lancet
2020, 395, 1968–1970, doi:10.1016/S0140-6736(20)31412-4.
102. Filardo, G.; Graca, B. Da; Sass, D.M.; Pollock, B.D.; Smith, E.B.; Martinez, M.A.M. Trends and comparison of female first authorship in high impact medical journals: Observational study (1994-2014). BMJ 2016, 352, i847, doi:10.1136/bmj.i847.
103. Laborde, B.D.; Martin, W.; Swinnen, J.; Vos, R. COVID-19 risks to global food security. Science 2020, 369, 500–502.
104. Erokhin, V.; Gao, T. Impacts of COVID-19 on trade and economic aspects of food security: Evidence from 45 developing countries. Int. J. Environ. Res. Public Health 2020, 17, 5775-5803, doi:10.3390/ijerph17165775.
105. Singh, D.R.; Sunuwar, D.R.; Adhikari, B.; Szabo, S.; Padmadas, S.S. The perils of COVID-19 in Nepal: Implications for population
health and nutritional status. J. Glob. Health 2020, 10, 010378–010381, doi:10.7189/jogh.10.010378.
106. UNICEF. The State of Foodsecurity and Nutrition in the World 2020. Transforming Food Systems for Affordable Healthy Diets; FAO:
Rome, Italy, 2020.
107. Cullen, M. COVID-19 and the Risk to Food Supply Chains: How to Respond? FAO. Recuper. 2020. Available online: http//www.
fao. org/3/ca8388en/CA8388EN. pdf (accessed on 19 October 2020).
108. Ipek, Y.; Aytekin, N.; Buyukkayhan, D.; Aslan, I. Food policy, nutrition and nutraceuticals in the prevention and management
of COVID-19: Advice for healthcare professionals. Trends Food Sci. Technol. 2020, 105, 186–199, doi:10.1016/j.tifs.2020.09.001.
109. Pulighe, G.; Lupia, F. Food first: COVID-19 outbreak and cities lockdown a booster for a wider vision on urban agriculture.
Sustain. 2020, 12, 5012-5015, doi:10.3390/su12125012.
110. Aldaco, R.; Hoehn, D.; Laso, J.; Margallo, M.; Ruiz-salmón, J.; Cristobal, J.; Kahhat, R.; Villanueva-rey, P.; Bala, A.; Batlle-bayer,
L.; et al. Food waste management during the COVID-19 outbreak: A holistic climate, economic and nutritional approach. Sci.
Total Environ. 2020, 742, 140524–140536, doi:10.1016/j.scitotenv.2020.140524.
111. Strasser, B.; Gostner, J.M.; Fuchs, D. Mood, food, and cognition: Role of tryptophan and serotonin. Curr. Opin. Clin. Nutr. Metab.
Care 2016, 19, 55–61, doi:10.1097/MCO.0000000000000237.
112. Rodríguez-Pérez, C.; Molina-Montes, E.; Verardo, V.; Artacho, R.; García-Villanova, B.; Guerra-Hernández, E.J.; Ruíz-López,
M.D. Changes in dietary behaviours during the COVID-19 outbreak confinement in the Spanish COVIDiet study. Nutrients
2020, 12, 1730-1748, doi:10.3390/nu12061730.
113. Bendall, C.L.; Mayr, H.L.; Opie, R.S.; Itsiopoulos, C.; Mayr, H.L.; Opie, R.S.; Itsiopoulos, C. Central obesity and the Mediterranean diet: A systematic review of intervention trials. Crit. Rev. Food Sci. Nutr. ISSN 2018, 58, 3070–3084,
doi:10.1080/10408398.2017.1351917.
114. Cheikh Ismail, L.; Osaili, T.M.; Mohamad, M.N.; Al Marzouqi, A.; Jarrar, A.H.; Abu Jamous, D.O.; Magriplis, E.; Ali, H.I.; Al
Sabbah, H.; Hasan, H.; et al. Eating habits and lifestyle during COVID-19 lockdown in the United Arab Emirates: A crosssectional study. Nutrients 2020, 12, 3314–3333.
115. Cicero, A.F.G.; Fogacci, F.; Giovannini, M.; Mezzadri, M.; Grandi, E.; Borghi, C.; Brisighella Heart Study Group. COVID-19-
related quarantine effect on dietary habits in a northern italian rural population: Data from the brisighella heart study. Nutrients
2021, 13, 309–318.
116. Marty, L.; de Lauzon-Guillain, B.; Labesse, M.; Nicklaus, S. Food choice motives and the nutritional quality of diet during the
COVID-19 lockdown in France. Appetite 2021, 157, 105005, doi:10.1016/j.appet.2020.105005.
117. Jia, P.; Zhang, L.; Yu, W.; Yu, B.; Liu, M.; Zhang, D.; Yang, S. Impact of COVID-19 lockdown on activity patterns and weight
status among youths in China: The COVID-19 impact on lifestyle change survey (COINLICS). Int. J. Obes. 2021, 45, 695–699,
doi:10.1038/s41366-020-00710-4.
118. Górnicka, M.; Drywień, M.E.; Zielinska, M.A.; Hamułka, J. Dietary and lifestyle changes during COVID-19 and the subsequent
lockdowns among polish adults: A cross-sectional online survey plife COVID-19 study. Nutrients 2020, 12, 2324–2343.
119. AlMughamis, N.; AlAsfour, S.; Mehmood, S. Poor eating habits and predictors of weight gain during the COVID-19 quarantine
measures in Kuwait: A cross sectional study [version 1; peer review: 2 approved with reservations]. FlooResearch 2020, 9, 914–
924, doi:10.12688/f1000research.25303.1.
120. Bhutani, S.; Cooper, J.A. COVID-19–related home confinement in adults: Weight gain risks and opportunities. Obesity 2020, 28,
1576–1577, doi:10.1002/oby.22904.
121. Muscogiuri, G.; Barrea, L. Nutritional recommendations for COVID-19 quarantine. Eur. J. Clin. Nutr. 2020, 74, 850–851,
doi:10.1038/s41430-020-0635-2.
122. Martín Giménez, V.M.; Inserra, F.; Ferder, L.; García, J.; Manucha, W. Vitamin D deficiency in African Americans is associated
with a high risk of severe disease and mortality by SARS-CoV-2. J. Hum. Hypertens. 2020, 1–3, doi:10.1038/s41371-020-00398-z.
123. Grant, W.B.; Lahore, H.; McDonnell, S.L.; Baggerly, C.A.; French, C.B.; Aliano, J.L.; Bhattoa, H.P. Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths. Nutrients 2020, 12, 988,
doi:10.3390/nu12040988.
124. Butler, J.R.A.; Davila, F.; Alders, R.; Bourke, R.M.; Crimp, S.; McCarthy, J.; McWilliam, A.; Palo, A.S.M.; Robins, L.; Webb, M.J.;
et al. A rapid assessment framework for food system shocks: Lessons learned from COVID-19 in the Indo-Pacific region. Environ. Sci. Policy 2021, 117, 34–45, doi:10.1016/j.envsci.2020.12.011.
125. Cao, W.; Fang, Z.; Hou, G.; Han, M.; Xu, X.; Dong, J. The psychological impact of the COVID-19 epidemic on college students
in China. Psychiatry Res. 2020, 287, 112934–112938, doi:10.1016/j.psychres.2020.112934.
126. Lee, J. Mental health effects of school closures during COVID-19. Lancet Child Adolesc. Health 2020, 4, 421, doi:10.1016/S2352-
4642(20)30109-7.
127. Rundle, A.G. COVID-19–related school closings and risk of weight gain among children. Obesity 2020, 28, 1008–1009,
doi:10.1002/oby.22813.
128. Kaur, S.P.; Gupta, V. COVID-19 Vaccine: A comprehensive status report. Virus Res. 2020, 288, 198114–198126
129. Chan, W.C.W. Nano research for COVID-19. ACS Nano 2020, 14, 3719–3720, doi:10.1021/acsnano.0c02540.
130. Palestino, G.; García-silva, I.; González-ortega, O.; Palestino, G.; García-silva, I.; González-ortega, O.; Rosales-mendoza, S. Can
nanotechnology help in the fight against. Expert Rev. Anti. Infect. Ther. 2020, 18, 849–864, doi:10.1080/14787210.2020.1776115.
131. Talebian, S.; Wallace, G.G.; Schroeder, A.; Stellacci, F.; Conde, J. Nanotechnology-based disinfectants and sensors for SARSCoV-2. Nat. Nanotechnol. 2020, 15, 618–621, doi:10.1038/s41565-020-0751-0.
132. Kramps, T.; Probst, J. Messenger RNA-based vaccines: Progress, challenges, applications. Wiley Interdiscip. Rev. RNA 2013, 4,
737–749, doi:10.1002/wrna.1189.
133. Mishra, S.K.; Tripathi, T. One year update on the COVID-19 pandemic: Where are we now? Acta Trop. 2020, 105778–105790,
doi:10.1016/j.actatropica.2020.105778.
134. Paltiel, A.D.; Schwartz, J.L.; Zheng, A.; Walensky, R.P. Clinical outcomes of a COVID-19 vaccine: Implementation over efficacy.
Health Aff. 2021, 40, 1377, doi:10.1377/hlthaff.2020.02054.
135. Helm, D. The environmental impacts of the Coronavirus. Environ. Resour. Econ. 2020, 76, 21–38, doi:10.1007/s10640-020-00426-
z.
136. Bauwens, M.; Compernolle, S.; Stavrakou, T.; Müller, J.; Van Gent, J; Eskes, H. Impact of coronavirus outbreak on NO2 pollution
assessed using TROPOMI and OMI observations. Geophys. Res. Lett. 2020, 47, e2020GL087978, doi:10.1029/2020GL087978.
137. Singu, S.; Acharya, A.; Challagundla, K.; Byrareddy, S.N. Impact of social determinants of health on the emerging COVID-19
pandemic in the United States. Front. Public Health 2020, 8, 406–415, doi:10.3389/fpubh.2020.00406.
138. Hoffart, A.; Johnson, S.U.; Ebrahimi, O.V. Loneliness and social distancing during the COVID-19 pandemic: Risk factors and
associations with psychopathology. Front. Psychiatry 2020, 11, 589127–589135, doi:10.3389/fpsyt.2020.589127.
139. Usher, K.; Marriott, R.; Smallwood, R.; Walker, R.; Shepherd, C.; Hopkins, K.; Skeffington, P.; Reid, C.; Jackson, D. COVID-19
and social restrictions: The potential mental health impact of social distancing and isolation for young Indigenous Australians.
Australas. Psychiatry 2020, 28, 599–600, doi:10.1177/1039856220943018.
140. Čavoški, A. An ambitious and climate-focused Commission agenda for post COVID-19 EU. Environ. Polit. 2020, 29, 1112–1117,
doi:10.1080/09644016.2020.1784010
141. Rowan, N.J.; Galanakis, C.M. Unlocking challenges and opportunities presented by COVID-19 pandemic for cross-cutting disruption in agri-food and green deal innovations: Quo Vadis? Sci. Total Environ. 2020, 748, 141362, doi:10.1016/j.scitotenv.2020.141362.
This entry is adapted from the peer-reviewed paper 10.3390/ijerph18115645
