Lipid mediators, produced from phospholipids, are critical influencers of apoptosis. Their generation is enhanced by the action of ROS [
47]. Phospholipids are structural elements of biological membranes, and the lipid bilayer represents an important platform for proteins involved in cell signaling that affect intercellular communication, gene expression, and immune response [
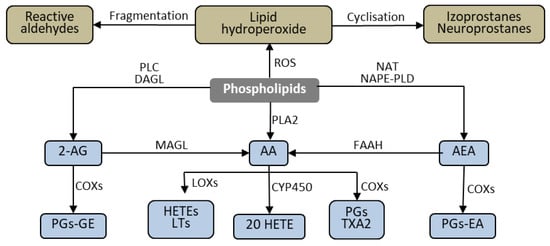
48]. However, under the influence of biological, chemical, and physical pathological factors, membrane phospholipids are metabolized to lipid mediators through ROS- and enzyme-dependent mechanisms . These mediators—through various metabolic pathways—can modulate the process of apoptosis [
47].
2.1. ROS-Dependent Lipid Peroxidation Products
Phospholipids containing polyunsaturated fatty acids (PUFAs), including arachidonic, linolenic, eicosapentaenoic, and docosahexaenoic acids, are particularly susceptible to ROS-dependent modifications [
48]. These modifications are initiated mainly by hydroxyl or hydroperoxide radicals generated from superoxide, which is an essential product of cellular metabolism, including the respiratory chain reactions and the activities of NADPH and xanthine oxidases. Superoxide is metabolized by the antioxidant enzymes and transition metal ions to hydroperoxide and hydroxyl radicals, influenced by the intensity of cellular metabolism and the action of exogenous factors [
49]. Pathological metabolism or increased activity of exogenous factors can result in increased ROS and the subsequent production of lipid peroxide radicals and lipid hydroperoxides.
Oxidative fragmentation of the alkyl chain of lipid hydroperoxides causes the formation of α,β-unsaturated reactive aldehydes, including 4-hydroxynenenal (4-HNE), 4-hydroxyhexenal (4-HHE), and malonic dialdehyde (MDA) [
50,
51]. Due to their electrophilic nature, these aldehydes have the ability to form complexes with the nucleophilic centers of proteins, phospholipids, and DNA, allowing them to they can modify their structure and functions. In this way, the formed aldehydes can participate in diverse cellular activities, such as transmitting signals in a variety of pathways [
52,
53,
54].
One of the best-known products of ROS-dependent phospholipid metabolism is 4-HNE. 4-HNE contributes to the modeling of cellular signals, including those associated with the process of apoptosis. As evidence of this, research has demonstrated that 4-HNE can modify the structure of the MDM2 protein, breaking down the MDM2-p53 complex. Consequently, p53 is activated and translocates to the nucleus, where it stimulates the transcription of proapoptotic proteins, including Bax (responsible for the release of proapoptotic factors from the mitochondrion) and effector caspase-3 [
55].
4-HNE may also interact with other proteins; for example, it forms adducts with His196, His267, Cys311, and Ser473 residues of AKT kinase, which results in a reduction in AKT sensitivity to phosphorylation. Additionally, modification of Ser473, considered to be the primary AKT regulatory site, leads to a decrease in the activity of the protein [
56,
57]. Because AKT has antiapoptotic effects through inhibiting several proapoptotic factors (including Acinus, AKS1, Bad, Bax, caspase-9) and activating antiapoptotic proteins (CREB and IKKα), suppression of AKT activity leads to a significant increase in apoptosis. Moreover, 4-HNE reduces the antioxidant capacity of cells by modifying glutathione (GSH) and GSH-Px structures, increasing oxidative stress [
58]. These conditions favor the phosphorylation of MAPK ERK1/2, resulting in the activation of this pathway and increased apoptosis. Although the mechanism of this phenomenon is not fully understood, the contribution of oxidative stress is demonstrated by the finding that antioxidants partially abolish 4-HNE-induced apoptosis [
59]. Similar to the proapoptotic activity of 4-HNE are the actions of another product of oxidative lipid fragmentation, 4-HHE [
60]. However 4-HNE is also known for its dual functionality, as in low concentrations (below 10 μM), it can stimulate cell growth without significantly affecting apoptosis. To achieve these effects, 4-HNE must interact with EGF, as cells grown in conditions without EGF do not show a similar effect [
61,
62].
4-HNE and 4-HHE also strongly activate caspase-2 and caspase-3 and, to a certain degree, caspase-8. Inhibition of any of these caspases results in a significant reduction in the level of apoptosis, suggesting that each of them plays a significant role in apoptosis induced by 4-HNE and 4-HHE [
60]. These findings indicate the involvement of 4-HNE and 4-HHE in the receptor pathway of apoptosis. Of particular relevance are the recent findings of novel anti-cancer, selective, concentration-dependent proapoptotic mechanisms of 4-HNE, through its inactivation of cancer-specific membrane-associated catalase [
63]. In vitro, 4-HNE causes apoptosis selectively in NOX1-expressing tumor cells through the inactivation of membrane-associated catalase. Thus, 4-HNE reactivates subsequent intercellular signaling through the NO/peroxynitrite and HOCl pathways, followed by the mitochondrial pathway of apoptosis. Moreover, high concentrations of 4-HNE can induce both necrosis and apoptosis of tumor cells, while at lower concentrations, 4-HNE can activate amplificatory pathways based on singlet oxygen formation through hydrogen peroxide and peroxynitrite interaction, with activation of the FAS receptor and caspase-8.
The anti-cancer pathways of 4-HNE may be useful for understanding its potential roles in the control of malignant cells and for the optimization of therapeutic approaches. In support of this is the recent finding that 4-HNE production is increased in non-malignant cells in the vicinity of human hepatocellular carcinoma or lung metastases of remote cancer. This highlights the possible role of 4-HNE as a natural anti-cancer substance as well as a detrimental factor in (neuro) degenerative and inflammatory processes [
64,
65,
66,
67,
68]. Finally, the quantities of 4-HNE protein adducts are of high importance for the cytotoxic/apoptotic effects of 4-HNE since they represent a reservoir for the persistent presence of 4-HNE, even in the absence of oxidative stress [
65,
69]. The amount of 4-HNE protein adducts is age-dependent and negatively correlates with the amount of GSH [
70,
71]. Therefore, differences in GSH metabolism and overall antioxidant capacities between cancer cells and their non-malignant counterpart cells are crucial for the selective anti-cancer cytotoxic/apoptotic effects of 4-HNE, and for the oxidative stress-related anti-cancer effects of cytostatic drugs and other biomedical remedies [
64,
68,
72,
73,
74,
75].
Apoptosis induced by factors causing oxidative stress is often accompanied by an increase in the level of another lipid peroxidation product—MDA [
76,
77,
78]. However, there is currently no evidence that MDA is directly involved in the process of apoptosis, although it might be involved in the stimulation of lipid metabolic pathways that affect apoptosis.
An alternative to the formation of reactive aldehydes is the intramolecular cyclization of lipid hydroperoxides. This causes the formation of prostaglandin derivatives, including isoprostanes (mainly from arachidonic acid) and neuroprostanes (mainly from docosahexaenoic acid), which are characterized by the presence of a cyclopentane ring [
79,
80]. Cyclic derivatives increase the production of ROS in mitochondria and further disturb the redox balance by oxidizing endogenous antioxidants, in particular, GSH [
80]. The generated ROS can modify DNA, causing the oxidation of nitrogenous bases—especially guanine, which causes GA or GT conversion—and double-strand breaks, leading to the activation of the p53 protein, which initiates the mitochondrial pathway of apoptosis [
81,
82]. MAPK ERK1/2 also participates in isoprostane-induced apoptosis. Therefore, inhibition of MAPK ERK1/2 results in a significant reduction, but not complete inhibition, of isoprostane-induced apoptosis [
80]. Isoprostanes interact with cells through several mechanisms, including by reacting with residues Phe196/184 and Asp193 on the thromboxane-like prostanoid (TP) receptors of which they are partial agonists [
83]. The activation of TP receptors by their full agonists causes the inhibition of apoptosis [
84]. However, it is not clear yet whether isoprostanes, as partial agonists, stimulate or inhibit the process of apoptosis through reactions with TP. Thus, the mechanisms of interaction of lipid peroxidation products in the process of apoptosis remain an open question.
2.3. Cross Talk between Lipids, Glucose, and Glutamine
Higher levels of both lipids and glucose are typical metabolic changes in diabetes and metabolic syndrome. However, increased levels of fatty acids, especially in the presence of glucose, increases ROS production, which ultimately leads to cell death [
146]. However, inhibition of some enzymes involved in lipid metabolism, such as acyl-CoA synthase, protects cells from fatty acid-induced apoptosis under elevated glucose conditions, suggesting that it is not the lipids, but their metabolites, that are responsible for this reaction [
147]. Despite the suggestion that elevated levels of fatty acids or glucose are not toxic, prolonged exposure to high levels of glucose and fatty acids would cause the accumulation of free fatty acid-derived long-chain acyl-CoA esters (FACoAs) and various lipid signaling molecules in cells, causing apoptosis [
148]. Lipids are able not only to modify the function of local cells but also because lipid mediators activate JNKs, can inhibit transcription of insulin [
149], which is a survival protein, and its absence causes increased apoptosis in the human organism [
150,
151]. On the other hand, insulin can be glycated when the glucose level is high, which causes the protein to become toxic to cells, which prevents β-Hydroxybutyric acid (BHB) production [
151]. BHB also blocks apoptosis by reducing MAPK p38 and MAPK JNK activity, as well as generating reactive oxygen species [
152].
Increased metabolism of glutamine to glutamate is observed in cancer cells. Glutamate is then converted into α-ketoglutarate and incorporated into the tricarboxylic acid (TCA) cycle, which leads to the production of the energy necessary to carry out cellular processes [
153]. However, stopping this process is not sufficient to cause cancer death. This is probably due to this pathway being compensated by increased lipid metabolism [
154].