Chromosome instability (CIN) is an increased rate where chromosome acquire alterations due to errors in cell division. CIN creates genetic and cytogenetic diversity and is a common feature in hematological malignancies such as acute myeloid leukemia (AML). Low to moderate levels of CIN seems to be well tolerated and can promote cancer proliferation, genetic diversity, and tumor evolution. However, high levels of CIN seems to be lethal, where enhancing CIN could improve AML treatment. However, little is known about CIN in AML.
- chromosomal instability
- acute myeloid leukemia
- cytogenetic heterogeneity
- aneuploidy
- complex karyotype
- TP53
- centrosome dysfunction
- MYC
- telomere dysfunction
- therapeutic targets
- aging
- synthetic lethality
Note: The following contents are extract from your paper. The entry will be online only after author check and submit it.
. Introduction
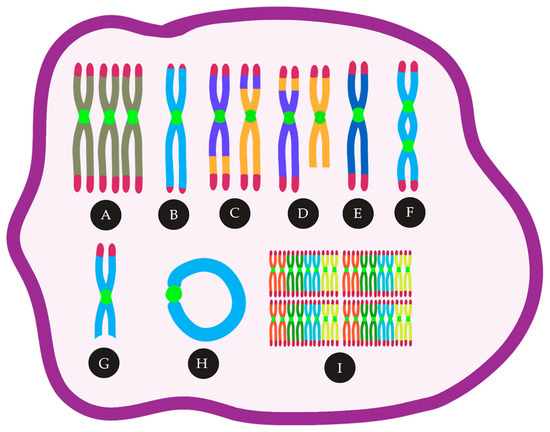
2. Mechanisms and Consequences of CIN
2.1. Aneuploidy and CIN in AML, Mechanism and Consequence — An Inter-Relationship
2.2. Chromosome Segregation Errors
2.2.1. Defects in the Spindle Assembly Checkpoint (SAC)
2.2.2. Cohesion Defects
2.2.3. Centrosome Dysfunction and Assembly of Multipolar Mitotic Spindles
2.3. DNA Double-strand Breaks
2.4. Telomere Dysfunction
2.5. Complex Chromosomal Rearrangements
2.6. Epigenetic Regulation
This entry is adapted from the peer-reviewed paper 10.3390/cancers13112655
