Giardia duodenalis (also named
G. lamblia or
G. intestinalis) is a protozoan parasite that infects humans and many animals through oro-fecal transmission [
79,
80,
81].
G. duodenalis is widely distributed in the environment as a resistant cystic form; once ingested, these cysts differentiate into trophozoite (a flagelled replicative form) by excystation in the correct GI tract conditions [
82]. The resulting enteropathogen can reach the colon and can cause giardiasis, one of the most common intestinal infectious diseases worldwide [
83,
84]. Considered a public health concern, several anti-infectious molecules have been developed to treat giardiasis [
81]. However, the emergence of drug resistant strains limits the efficacy of the available treatments [
81]. Recent reports established a strong interaction between
G. duodenalis and the gut microbiota. In fact, it was highlighted that giardiasis susceptibility is highly influenced by the composition of the gut microbiota [
85,
86,
87]. In turn,
G. duodenalis colonization leads to gut microbiota composition changes [
86]. Intriguingly, Riba et al. (2020) reported that
Giardia infection alters the enteric microbiota composition in neonatal mice and modulates BAs and lipid metabolism, leading to reduced body weight gain and growth, as noted in infected infants [
88]. Previous studies investigated the effect of probiotic bacteria (
L. johnsonii La1,
L. gasseri CNCM I-4884) in the field of giardiasis [
89,
90,
91]. Both strains promote immune response, protect against
Giardia-mediated tissue injury, and prevent trophozoite proliferation in murin models [
89,
91]. Of note,
L. gasseri is more effective in vivo than
L. jonshoni since
L. gasseri reduces the cystic pool of the parasite [
89]. Other lactobacillus strains, including
L. casei MTCC 1423 and
L. rhamnosus, have been tested in a murine model, showed similar protective effects, and reduced the severity/duration of giardiasis [
92,
93,
94]. Interestingly, Shukla et al. (2020) reported an anti-giardia effect and enhanced mucosal immunity by the probiotic protein from
L. rhamnosus as well as the heat-killed strain [
95]. Although the underlying mechanism remains poorly understood [
96,
97,
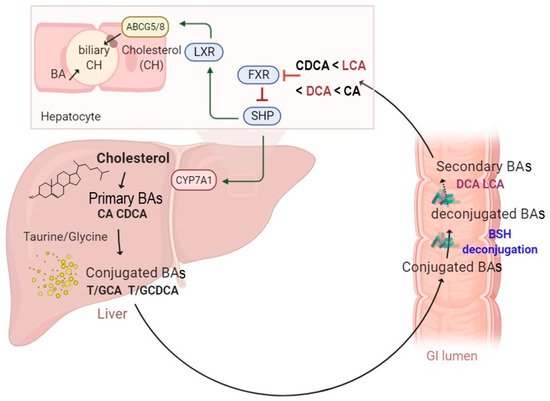
98], recent reports demonstrate a potential association between BSH activity and the protective effect against
G. duodenalis infection [
99,
100]. As BSH activity allows for the conversion of primary BAs into deconjugated bile acids, it was suggested that the subsequent release of secondary BAs has a toxic effect and may alter parasite growth and survival. To address this hypothesis, the direct effects of conjugated and deconjugated BAs on the parasite were tested. Both tauro- and glyco-conjugated BAs were inert and did not inhibit parasite growth, while deconjugated BAs (DC and CDC) were toxic in a dose-dependent manner and exhibited a significant deleterious effect on the parasite [
99]. Moreover, the simultaneous incubation of
G. duodenalis with unconjugated BAs and BSH from
C. perfringens allowed for the conversion of incubated BAs into their conjugated forms and consequently led to a killing effect on the parasite [
99]. In addition, engineered
E. coli to express BSH from
L. johnsonii confirmed that BSH antagonized
Giardia proliferation in vitro in a dose dependent manner as well as in vivo [
100]. Altogether, these results support the promising prospect of using BSH active probiotics as a new therapeutic strategy to treat/prevent
G. dudenalis infection.
Another example of a gastrointestinal infectious disease includes
Clostridioides difficile infection (CDI).
C. difficile is a spore-forming pathogen that might colonize the gut of patients treated by broad-spectrum antibiotics [
101,
102]. CDI includes a broad range of disorders ranging from diarrhea to colitis and toxic megacolon [
101]. Their incidence, severity, and costs are in continuous increase. In addition, they have evolved as a significant cause of mortality during the past decade [
101,
103,
104]. Upon germination, vegetative cells are generated from spores, and the bacterium produces toxins that result in tissues damage, inflammation, and diarrhea [
105,
106]. In the GI tract, the germination process is mediated by a host-derived molecule including BA sensing through the bile acid germinant receptor [
105,
107,
108,
109]. In fact, TCA, CA, and DCA activate germination, while CDCA acts as a competitive inhibitor [
110]. Other studies indicate that DCA is a potent inhibitor of this process, as reported with
C. scindens. Upon administration, this strain enhances the resistance to infection in a DCA dependent fashion [
111]. Recent reports revealed that severe and relapsing CDI patients display high levels of TCA, followed by a reduced abundance of BSH-producing species [
112,
113]. However, fecal transplantation is effective in treating these patients and increases their resistance to CDI [
112,
113,
114]. Further analysis demonstrates that, following FMT, key bacterial genera responsible for BSH production are recovered, BSH activity and BSH gene copy numbers are balanced, and secondary BAs are restored [
112,
113]. Interestingly, unlike patients pre-FMT, the BA profiles, similar to that in patients post-FMT, were able to inhibit spores outgrowth into vegetative forms [
115]. In addition, supernatants from either engineered
E. coli expressing highly active BSH or naturally BSH-producing organisms (
Bacteroides ovatus,
Collinsella aerofaciens,
Bacteroides vulgatus, and
Blautia obeum) effectively reduced TCA-mediated
C. difficile germination. These effects were also confirmed in a recurrent CDI mouse model, using the recombinant
E. coli strain for BSH [
112]. These distinctive features pave the way towards the potential use of BSH active probiotics to treat CDI. However, active research must be conducted in this field to unravel the molecular mechanism of how secondary BAs may inhibit
C. difficile outgrowth, colonization, and the subsequent inhibition of infection.