3. Vaccine Development
As vaccines are considered the most promising way to eradicate the SARS-CoV-2 virus, several teams are intensively working on vaccine development [
151]. Vaccines are being developed with different technologies, some well-known and others completely new for human vaccines, such as peptide and nucleic acid technologies.
Currently, there are two messenger RNA (mRNA) vaccines and two vector vaccines to prevent COVID-19, all authorized by the European Medicines Agency (EMA). The first mRNA vaccine, Comirnaty (BNT162b2), developed by BioNTech and Pfizer, was authorized by December 2020 [
152]. In January 2021, the EMA approved the COVID-19 vaccine Moderna (mRNA-1273), which was developed by the National Institute of Allergy and Infectious Diseases (NIAID) in collaboration with Moderna Biotech Spain, S.L. [
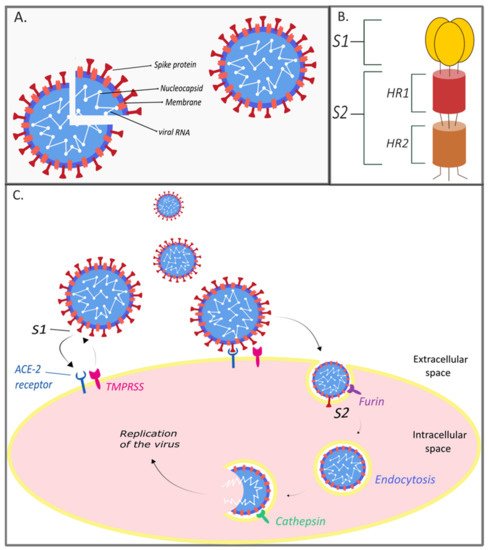
153]. Both contain lipid nanoparticle (LNPs)-encapsulated mRNA, which encodes the spike protein of SARS-CoV-2 [
154]. This technique does not include parts of the virus, only the sequence of spike protein encoded to mRNA. For successful delivery, novel lipid nanoparticles are used to protect the protein sequence. After intramuscular application, the LNPs are removed by myocytes and the mRNA is released and translated to endogenously synthesized spike protein. The mRNA is very sensitive, and therefore is broken down shortly after vaccination. These vaccines activate T cells cytotoxicity as well as B cells response, which ultimately causes strong cellular immunity [
154,
155,
156,
157].
The technology of adenovirus-based vectors is an already proven method of vaccine preparation, in a relatively short time, through modification of an adenovirus vector carrier through the insertion of a “gene of interest” such as the code of a spike protein. The Vaxzevria (previously COVID-19 vaccine AstraZeneca/Oxford) is an adenovirus vaccine (ChAdOx) that has been authorized by the EMA since January 2021. It is a chimpanzee adenovirus-vectored vaccine encoding the SARS CoV 2 spike glycoprotein (ChAdOx1-S, ChAdOx1 nCoV-19), manufactured by the Serum Institute of India and SKBio [
158]. Results from four clinical trials in the United Kingdom, Brazil, and South Africa showed that Vaxzevria was safe and effective at preventing COVID-19, as well as resulting in robust neutralizing antibody and T-cell responses [
159,
160,
161,
162]. In March 2021, with the increase in vaccination across the population, some serious adverse reactions occurred with ChAdOx1 nCov-19 (AstraZeneca) and Janssen (Johnson & Johnson) vaccines. In very rare cases, their use has led to the development of immune thrombotic thrombocytopenia (very similar to heparin-induced autoimmune thrombocytopenia, HIT) caused by anti-platelet factor 4 (anti-PF4) antibodies that activate platelets. These pathological changes may cause unusual clotting such as cerebral venous thrombosis [
163,
164]. More data on this pathophysiology are therefore crucial for preventing these harmful effects. Nonetheless, EMA issued a statement that the benefits of Vaxzevria continue to outweigh its risks, and the vaccine can continue to be administered.
The COVID-19 vaccine Janssen is another vector vaccine, developed by Johnson & Johnson, that received authorization in the EU in March 2021 [
165]. This vaccine is composed of replication-incompetent human adenovirus that encodes a SARS-CoV-2 full-length spike glycoprotein and provokes a similar immune response after vaccination as Vaxzevria.
For the Sputnik V vaccine, which is already registered in more than 55 countries, an EMA rolling review started on the 4th March [
166,
167]. Unlike the COVID-19 vaccine Janssen, Sputnik V includes two different types of human adenovirus vectors (rAd26 and rAd5), which ensure lasting immunity [
168].
All approved vaccines within the EU are safe, while differing in efficacy ranging from 72 to 95%. Most vaccines are given in two doses, except for Johnson & Johnson (Janssen), who state that a single dose will provide protection against the disease. Likewise, they differ in other factors such as time required for full immune response, protection against COVID-19 in the aged and young population, suitability for the elderly, and storage properties.
Expectations from EU-approved vaccines to produce nationwide immunity against COVID-19 as well as identifying their side effects and possible health risks need to be monitored in further large-scale randomized clinical trials.
Several vaccines have been developed and tested in other countries apart from in Europe. India‘s first COVD-19 vaccine Covaxin (Bharat Biotech) is an inactivated vaccine developed using whole-virion-inactivated, Vero cell-derived platform technology. It has demonstrated 81% efficacy [
169]. These types of inactivated vaccines have also been developed in China, namely, Synopharm and Sinovac, showing similar efficacy in COVID-19 prevention [
170]. American Novavax has developed a unique protein-based vaccine, NVX-CoV2373 (trade name COVOVAX), requiring two doses with an efficacy of 86% (UK variant) and 60% (South African variant) [
171].
Vaccination is crucial for achieving a sufficient level of protection against the virus, especially for immunocompromised patients and patients with comorbidities. For this reason, cancer patients who are at an even higher risk of severe COVID-19 infection should be prioritized for vaccination against SARS-CoV-2. These patients are advised to use mRNA vaccines (BNT162b2, Pfizer-BioNTech vaccine), which have a better safety profile and therefore a lower risk of adverse reactions in these patients [
172]. However, the efficacy of these human vaccines in these patients is questionable [
173]. The BNT162b2 vaccine was shown to be effective and safe in a study of 134 patients and older adults with various frailty and disability profiles, providing protection regardless of their condition [
174]. On the other hand, several studies have found lower levels of antibodies in patients with multiple myeloma after the first dose of this vaccine than in the vaccine trials [
175,
176]. These findings further increase the emphasis of the second dose in cancer patients. However, large prospective and well-designed clinical trials regarding efficacy and safety among immunocompromised patients are necessary.